An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Overview of Systematic Reviews: Yoga as a Therapeutic Intervention for Adults with Acute and Chronic Health Conditions
Marcy c mccall, alison ward, nia w roberts, carl heneghan.
- Author information
- Article notes
- Copyright and License information
*Marcy C. McCall: [email protected]
Academic Editor: Stefanie Joos
Received 2012 Dec 20; Revised 2013 Feb 21; Accepted 2013 Mar 21; Issue date 2013.
This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objectives . Overview the quality, direction, and characteristics of yoga interventions for treatment of acute and chronic health conditions in adult populations. Methods . We searched for systematic reviews in 10 online databases, bibliographic references, and hand-searches in yoga-related journals. Included reviews satisfy Oxman criteria and specify yoga as a primary intervention in one or more randomized controlled trials for treatment in adults. The AMSTAR tool and GRADE approach evaluated the methodological quality of reviews and quality of evidence. Results . We identified 2202 titles, of which 41 full-text articles were assessed for eligibility and 26 systematic reviews satisfied inclusion criteria. Thirteen systematic reviews include quantitative data and six papers include meta-analysis. The quality of evidence is generally low. Sixteen different types of health conditions are included. Eleven reviews show tendency towards positive effects of yoga intervention, 15 reviews report unclear results, and no, reviews report adverse effects of yoga. Yoga appears most effective for reducing symptoms in anxiety, depression, and pain. Conclusion . Although the quality of systematic reviews is high, the quality of supporting evidence is low. Significant heterogeneity and variability in reporting interventions by type of yoga, settings, and population characteristics limit the generalizability of results.
1. Introduction
Over 30 million people practice yoga, a spiritual and health discipline of Indian origin [ 1 ]. In January 2007, yoga therapy was defined as the “process of empowering individuals to progress toward improved health and well-being through the application of the philosophy and practice of Yoga” [ 2 ]. Nearly 14 million Americans (6.1% of the population) say that a doctor or therapist has recommended yoga to them for their health condition [ 3 ]. In the United Kingdom, national healthcare services promote yoga as a safe and effective way to promote physical activity, improving strength, balance, and flexibility as well as a potential benefit for people with high blood pressure, heart disease, aches and pains, depression, and stress [ 4 ].
Yoga research in medical health literature continues to increase. Over 2000 journal articles in yoga therapy have been published online ( http://www.ncbi.nlm.nih.gov/pubmed ). In 2012, 274 new yoga articles were added to PubMed, with 46 results after a “systematic review” title search on the US National Library of Medicine. However, the quality and direction of evidence for yoga therapy is unclear. In one clinical review, results show psychological symptoms and disorders (anxiety, depression, and sleep), pain syndromes, autoimmune conditions (asthma, diabetes, and multiple sclerosis), immune conditions (lymphoma and breast cancer), pregnancy conditions, and weight loss are all positively affected by yoga [ 6 ]. An overview from 2010 includes 21 systematic reviews that yield unanimous positive results for just two conditions—cardiovascular risk reduction and depression [ 7 ].
The aim of this overview is to systematically collect, summarize, and evaluate key findings in yoga systematic reviews to determine the strength of evidence in adult health conditions. Components of yoga interventions, the quality and direction of evidence will be investigated for the first time.
2.1. Criteria for Considering Reviews for Inclusion
2.1.1. types of reviews.
Systematic reviews of yoga as a primary intervention to treat any health condition with at least one randomized-controlled trial (RCT) of yoga are included. Any review assessing multiple health conditions is excluded. Included reviews must satisfy all Oxman criteria as follows: state a replicable search method; adequately attempt to retrieve all relevant data; collect the data in a systematic way; analyze and present the results appropriately; consider sources of bias and the quality of evidence [ 48 ]. To allow for sufficient in-depth analysis of each systematic review, publications after June 1, 2012, are not included though considered in the discussion and limitations of the overview.
2.1.2. Types of Participants
As the population of interest, adult participants with a diagnosed and existing acute or chronic health condition are included. Systematic reviews with asymptomatic or otherwise healthy participants and children (<18 years) are excluded to limit the heterogeneity in an already comprehensive overview.
2.1.3. Types of Interventions
Any type of yoga as defined by review authors compared to a control group receiving no intervention or interventions other than yoga is included. A definition for yoga or yoga therapy in research has not been standardized though for the purposes of this overview, authors define yoga as “any movement meditation technique that includes breathing techniques (pranayama) or one or more of the following: physical postures specific to yoga, meditation or chanting (mantra) in the name of yoga.” Allied health or healing arts that are similar to, but do not call themselves, yoga are not included. Martial arts or alternative healing modalities including Karate, Tai Chi, Qigong, reiki, massage, stretching alone, pilates, and acupuncture are not included. Talk therapies including psychological, social, and cognitive behavioral modification strategies are excluded. Systematic reviews that include multiple interventions with yoga are included when the yoga data can be isolated.
2.2. Outcomes
After consultation amongst the authors (M. C. McCall, C. Heneghan, A. Ward), the following list of outcomes are identified for analysis and will be included if authors note them as either primary or secondary outcomes.
2.2.1. Primary Outcomes
All-cause mortality.
Direction and magnitude of disease progression.
Surrogate markers and biomarkers that correlate with disease progression (i.e., blood pressure, resting heart rate, and endocrine levels).
Number of clinical visits and/or hospital utilization rates.
Changes in medication or prescription patterns.
2.2.2. Secondary Outcomes
Self-reported measures of health, coping or other (i.e., HRQL).
Psychosocial or behavioral outcomes.
Cost effectiveness and related evaluations.
2.3. Search Methods for Identification of Reviews
An electronic search of 10 online health databases including Medline, Cochrane Library, and CINAHL was designed by combining natural language and MeSH terms for yoga as the key components, see the Appendix (M. C. McCall, N. Roberts). In addition, hand-searches of relevant journals and journalistic books including The Science of Yoga [ 49 ] and Yoga as Medicine [ 50 ] were conducted. Websites of known yoga research institutes were visited. References and bibliographies of found reviews were searched for additional titles.
2.4. Data Collection and Analysis
2.4.1. selection of reviews.
The first reviewer screened titles, abstracts, and full articles found from electronic and other sources. A second reviewer (C. Heneghan) provided supervision and random assessment of the selection process.
2.4.2. Data Extraction and Management
One reviewer (M. C. McCall) systematically collected and extracted the data to standardized digital collection forms. Two other reviewers (C. Heneghan, A. Ward) independently assessed the accuracy of the data collection. Consensus through discussion or eventual consultation of a third-party resolved any discrepancies. Any missing data is considered a limitation of the overview. In reviews that include multiple interventions and yoga, data is collected on a separate database to allow for independent analysis. In multiple intervention reviews, only yoga-specific data is reported.
2.5. Assessment of Methodological Quality of Included Reviews
We address two aspects of quality for the included reviews: the quality of evidence included in the reviews and the quality of the systematic reviews themselves. The first reviewer performed the quality assessments with supervision from a second author.
2.5.1. Quality of Evidence in Included Reviews
The authors sought to record “Grade of Recommendations Assessment, Development and Evaluation” (GRADE) from systematic reviews. When other measures of quality were employed, judgments by first author (M. C. McCall) were made to downgrade or upgrade the quality of evidence based on the amount of potential bias due to study design and other criteria specified in the GRADE toolbox [ 51 ]. Insufficient data was reported in instances where adequate information was unavailable.
2.5.2. Quality of Included Reviews
The authors implemented the “assessment of multiple systematic reviews” (AMSTAR) measurement tool [ 52 ].
2.6. Data Synthesis
Characteristics of all included reviews and the overview of reviews tables summarize the key findings of data collection. The summary of results includes a narrative analysis and quantitative information, where possible. Given sufficient data, the following subgroups are identified for analysis: gender, age, ethnicity, interventions by type of practice, mode of delivery, setting, duration of sessions, duration of interventions, and intensity in terms of physiological effort such as caloric expenditure or cardiovascular output.
3.1. Description of Included Reviews
Twenty-six systematic reviews are included in this overview. Six systematic reviews provide quantitative data with meta-analyses, seven reviews provide descriptive data with no pooled analysis, and 13 reviews contain qualitative descriptions of results. Twelve systematic reviews include only yoga interventions. Figure 1 outlines the selection process in an article flow diagram. Refer to Table 1 for characteristics of included reviews. See additional Table 2 for full list of reviews and reasons for exclusion. The systematic reviews include evidence from 125 primary studies, of which 92 studies include only yoga interventions.
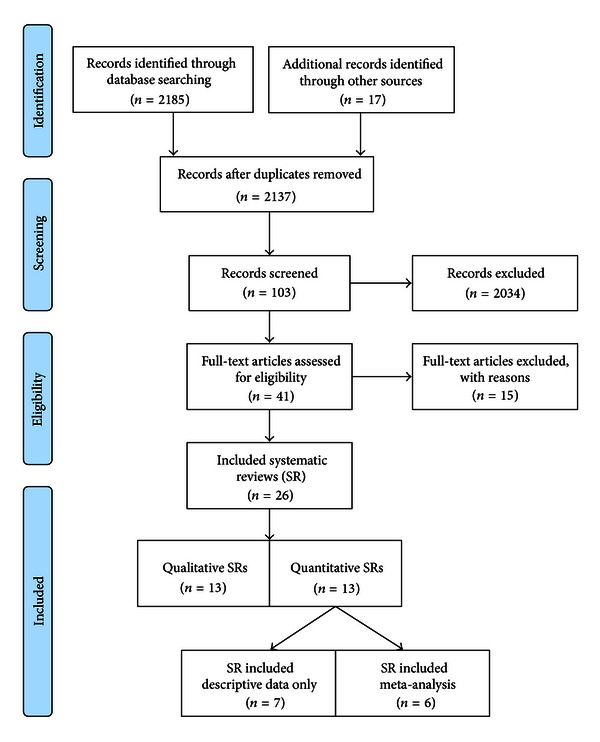
Flowchart of systematic review selection [ 5 ].
Characteristics of included systematic reviews.
Italics: systematic reviews including only yoga interventions.
Normal: systematic reviews including yoga interventions plus other interventions.
Characteristics of excluded reviews (ordered by review author).
3.1.1. Population
The total number of participants across all studies is 5915. Six reviews do not include studies with sample sizes greater than 50 participants at baseline. The age range of participants is 18 to 77 years. Mean age, gender, ethnicity, or socioeconomic status of the sample population is unavailable due to insufficient reporting, although the majority of participants are women.
Twelve systematic reviews investigate only yoga interventions and include the following health conditions: anxiety (4 reviews), pain management (2 reviews), with one review each in depression, epilepsy, psychiatric disorder, diabetes, arthritis, and relief of menopause symptoms. The 14 systematic reviews that include yoga therapy in combination with other interventions measured health outcomes in carpal tunnel syndrome and diabetes risk factors (2 reviews each), with one review each in anxiety, asthma, chronic kidney disease, fibromyalgia, hypertension, low back pain, menopause, pain management in labor, chronic pain, and osteoarthritis.
3.1.2. Length of Intervention and Followup
Of 25 reporting systematic reviews, one (with 2 primary studies) includes only trials ≥24 weeks duration. Follow-up measures are mentioned in eight of the 26 reviews, where four report on primary studies that include follow-up measures ≥12 weeks, two report follow-up measures <12 weeks, and two report no follow-up evaluations.
3.1.3. Characteristics of Intervention
Twenty-two systematic reviews include any type of yoga intervention. Two systematic reviews include only Kundalini yoga [ 18 , 19 ] one systematic review each includes only Restorative yoga [ 9 ] and Yoga of Awareness [ 20 ]. The other types of yoga intervention are listed in Box 2 include: Viniyoga, Integrated yoga, Raj, Iyengar, Kriya, Sahaja, Siddha Samadhi, hot, water, and Tibetan yoga. Modified, non-descriptive, or unspecified yoga interventions are included in 12 systematic reviews. Interventions of Ashtanga, power, or flow yoga are not found. The most prevalent yoga intervention by type includes Iyengar (9 reviews), Hatha (7 reviews) Restorative (5), and Kundalini and Integrated yoga (3 reviews each).
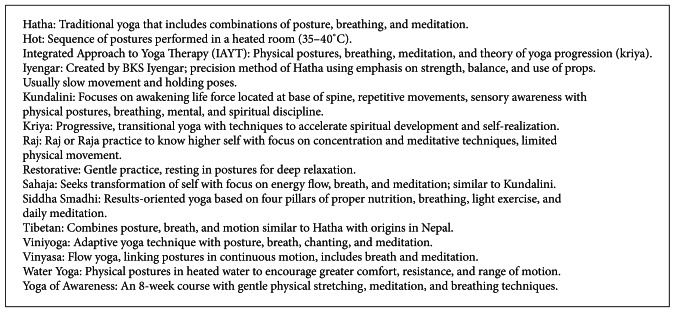
Types of yoga intervention.
Nine of the systematic reviews do not report on the type of delivery mechanism of yoga used in their primary studies. Instructor-led yoga is identified in a majority of cases (17 reviews), independent or home study (13 reviews), book-led yoga (5 reviews), audio-led yoga (4 reviews), and video-led yoga in one review. No review evaluates the effect of yoga by type or delivery mechanism for a specific health condition. Twenty reviews report the duration and frequency of yoga sessions. The duration of yoga sessions varies between 20 and 300 minutes, an intervention of 60 minutes in length most prevalent. Seven reviews include yoga interventions with <3 yoga sessions per week, three reviews include only yoga interventions with ≥3 sessions per week, and 10 reviews include both frequencies of yoga sessions. Systematic reviews do not report on the intensity of yoga interventions in terms of physiological effort such as cardiac output or caloric expenditure.
3.1.4. Comparisons
Fourteen of the 26 systematic reviews (28 primary studies) report a waitlist as comparison for treatment for yoga. Other kinds of exercise are compared to yoga in 11 systematic reviews (19 primary studies), nine systematic reviews (16 primary studies) identify usual care, while medicinal intervention is noted in three reviews (4 primary studies). Four systematic reviews (19 studies) do not report the use of control groups or comparisons. Other comparisons reported in the reviews include disseminating reading material (5 reviews, 5 studies), sham yoga (3 reviews, 5 studies), talk therapy (2 reviews, 3 studies), and lectures (2 reviews, 2 studies).
3.2. Methodological Quality of Included Reviews
3.2.1. quality of included reviews.
The overall quality of systematic reviews is high (AMSTAR average = 9.4). Fifteen of the reviews are considered of very high quality (AMSTAR ≥ 10), 6 of high quality (AMSTAR 8–9.9), 5 reviews of medium quality (4–7.9 AMSTAR), and no systematic review scores below 4 points. See Table 3 for the AMSTAR ratings of the included systematic reviews. All 26 reviews scored in five of eleven methodological criteria including (refer to Box 1 ): identification of a priori design, using duplicate referees for study selection and data extraction, implementing a comprehensive literature search, considering the status of publication for inclusion, and the assessment and documentation of the scientific quality of evidence. The characteristics of included studies, respective quality, and the methods to combine findings of those studies are appropriate in 21 reviews. Lists of excluded studies and conflicts of interest are inconsistently reported (16 reviews only). A statistical investigation to determine a likelihood of bias is most poorly reported (2 of 12 yoga—only reviews).
Overview of reviews: quality and outcomes summary.
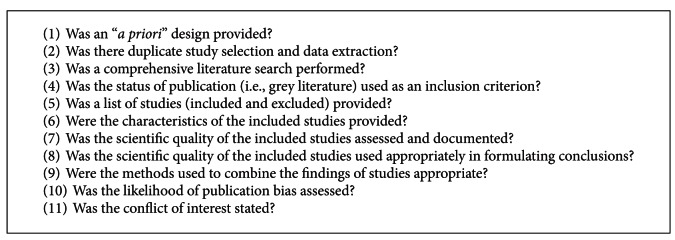
The AMSTAR tool criteria.
3.2.2. Quality of Evidence in Included Reviews
The quality of evidence ranges from very poor/low to moderate quality (see Table 3 ). No high-quality evidence is included in the reviews. Systematic review authors implement a diverse set of tools to evaluate evidence, including Jadad scores, CONSORT guidelines, and PEDro scales. In 16 systematic reviews, the GRADE approach is applied to uniform results, while 10 reviews did not provide sufficient data to independently assess their quality of evidence.
3.3. Effects of Interventions
3.3.1. all-cause mortality.
Outcome results for all-cause mortality are not studied in the reviews. The absence of data could be due to characteristics of study design including length of trials (typically 3–6 months) and small sample sizes ( n < 50). The population samples usually include middle-aged adults receiving treatment for chronic illnesses; thus, mortality may be limited in such groups, or yoga therapy may have no effect on reducing mortality.
3.3.2. Direction and Magnitude of Disease Progression
Nine reviews measure the direction and magnitude of disease progression. These chronic diseases include anxiety [ 18 , 19 ], depression [ 27 ], treatment of psychiatric disorder [ 11 ], clinical outcomes in arthritis [ 14 ] and osteoarthritis [ 23 ], carpal tunnel syndrome [ 26 ], epilepsy [ 30 ], and asthma [ 29 ]. Included studies of yoga therapy are characteristically short in duration, which will contribute to the lack of available evidence to analyze this outcome.
3.3.3. Surrogate Markers and Biomarkers That Correlate with Disease Progression (i.e., Blood Pressure, Resting Heart Rate, and Endocrine Levels)
Five systematic reviews measure surrogate markers that correlate with disease progression including blood pressure [ 12 ], body mass index [ 9 ], metabolic and anthropometric measures for diabetes mellitus [ 16 ], fasting blood glucose [ 8 ] and muscular strength [ 15 ]. Higher quality research with controlled clinical trials report a 6.9% reduction in fasting glucose of adults with diabetes and 7.8% reduction in body weight, with reductions in systolic and diastolic blood pressures ranging from 3.9 to 13.9% and 5.8 to 15.8% for adults with diabetes or at risk of CVD [ 16 ]. Although an average decrease of 3/5 mmHg is found in hypertensive patients, Dickinson et al. suggest no good evidence exists to confirm yoga therapy is effective for treatment of hypertension as studies are too small to detect any effect on morbidity or mortality. Study designs lack blinding and use inadequate randomization techniques, thus potential biases and limitations characterizing most of these studies hinder interpretation of findings [ 8 , 9 , 15 , 16 ].
3.3.4. Number of Clinical Visits and/or Hospital Utilization Rates
Systematic reviews do not report changes in number of clinical visits and/or hospital utilization rates with yoga intervention. Although a number of interventions are implemented in a clinical setting (9 of 26 reviews), it is possible that primary researchers did not collect data regarding hospital referral rates, perhaps due to limited resources or short-time horizons.
3.3.5. Changes in Medication or Prescription Patterns
Two systematic reviews measure changes in medication with yoga intervention [ 16 , 28 ]. One author concludes that yoga may be beneficial in decreasing medication usage in diabetes [ 16 ]; the second study concludes with caution that yoga may decrease medication usage in pain conditions, although results were not statistically significant [ 28 ].
3.3.6. Self-Reported Measures of Health, Coping or Other (i.e., HRQL)
Twelve systematic reviews include self-reported measures for pain management [ 10 , 13 , 20 , 22 , 24 , 25 , 28 , 31 , 33 ], menopausal symptoms [ 17 , 21 ], perceived stress [ 25 ], psychological wellbeing, and quality of life for cancer patients [ 22 , 32 ]. Seven review authors conclude positive effects [ 10 , 17 , 20 , 22 , 24 , 28 , 32 ]. One RCT with treatment of low-back pain shows that Iyengar yoga ( n = 60) can reduce pain intensity (64%), functional disability (77%), and pain medication usage (88%) versus the education control group with usual care [ 10 ]. The overview of various pain conditions (headaches, back pain, muscle soreness, labor, and arthritis) yields a moderate effect size of yoga as measured by visual analog scales and questionnaires (VAS, CMDQ, and PPI) at SMD −0.74 (95%CI, − 0.97 to − 0.52; P < 0.0001) [ 10 ]. Quality of life for cancer patients in yoga groups approaches significance ( P = 0.06) with an SMD −0.29 (95% CI, −0.58 to 0.01) while psychological health outcomes (anxiety, depression, distress, stress) show a pooled effect size of SMD −0.95 (95% CI, − 1.63 to − 0.27; P = 0.006) as measured by HADS, PSS, STAI, POMS, CES-D, PANAS, IES, SCL-90-R, SOSI and the distressed mood index. An earlier review (search date of April 2008) reports encouraging preliminary results for cancer patients with effect sizes that range from 0.04 to 4.67 (anxiety) and 0.17 to 7.44 (depression) in favor of yoga with concurrent treatment, though statistical significance and measuring tools are not reported [ 32 ].
Attributed to the lack of scientific rigor in large-scale and long-term studies, four reviews conclude neutral or unknown effects of yoga intervention for pain in carpal tunnel syndrome [ 13 ], pain in low back [ 31 ], in older adults [ 25 ], and for labor management [ 33 ].
3.3.7. Psychosocial or Behavioral Outcomes
Systematic reviews do not report results on psychosocial or behavioral outcomes.
3.3.8. Cost Effectiveness and Related Evaluations
Systematic reviews do not include results on cost effectiveness and related evaluations. This narrow focus is in part due to early research development and potential lack of funding to implement trials with several outcome measures.
3.4. Quantitative Reports
3.4.1. meta-analyses.
Of the six reviews that included a meta-analysis of results, three investigate outcomes in pain [ 10 , 20 , 31 ], one review each in psychiatric disorders [ 11 ], menopausal symptoms [ 21 ], and psychological health in cancer patients [ 22 ]. For pain studies, interventions include Hatha, Iyengar, Yoga of Awareness, water yoga, Viniyoga, and unspecified yoga programs. Comparisons with physical activity, education sessions, waiting lists, routine care, and talk therapy show unanimously positive results for yoga in pain reduction [ 10 , 20 , 31 ]. These results suggest a moderate effect size of yoga to reduce acute pain in adult populations SMD −0.74 (95% CI, −0.97 to −0.52), in fibromyalgia patients SMD −0.54 (95% CI, −0.96 to −0.11) and low-back pain versus education, self-care, and no exercise. Conversely, yoga did not indicate positive results for menopausal symptoms including pain, psychological wellbeing, and quality of life [ 21 ].
As an adjunct therapy, Cabral et al. conclude that yoga improves treatment of depression, anxiety, posttraumatic stress disorder (PTSD), and schizophrenia, with a pooled effect size of SMD −3.25 (95% CI, − 5.36 to − 1.14; P = 0.002). Pranayama techniques are implicated as most important for anxiety and stress-related disorders [ 11 ]. See Table 4 for overview of reviews with pooled results.
Overview of reviews—primary outcomes (yoga meta-analyses).
n.r: not reported; BDI: Beck Depression Inventory; VAS: Visual Analogue Scale; MENSI: Menopausal Self-inventory; MPQ: McGill pain questionnaire; PPI: Present Pain Index; CMDQ: Cornell Musculoskeletal Discomfort Questionnaire; HADS: Hospital Anxiety and Depression Scale; PSS: Perceived Stress Scale; STAI: State of Trait Anxiety Inventory; SOSI: Symptoms of stress inventory; POMS: Profile of Mood States; SCL-90-R: Symptoms Checklist Revised; CES-D: Center for Epidemiologic Studies Depression Scale; PANAS: Positive and Negative Affect Schedule; IES: Impact of Events Scale; DMI: Distressed Mood Index; SF-36: Medical Outcomes Study Short-Form Health Survey; SF-12: The 12-Item Short Form Health Survey; FACT_B: Functional Assessment of Cancer Therapy-Breast; FACT_G: Functional Assessment of Cancer Therapy-General; EORTC QLQ-C30: European Organization for research and Treatment of Cancer Quality of Life Questionnaire Version 3.0; MBSR: Mindfulness-based stress reduction.
*Average Jadad score.
**Average PEDro scale.
3.4.2. Independent Study Reports (No Pooled Analysis)
Descriptive quantitative data of yoga primary studies is provided in seven reviews. Three of these reviews test the direction and magnitude of disease progression with yoga intervention for anxiety [ 18 ], asthma symptoms [ 29 ], and seizure frequency in epileptics [ 30 ]. Heiwe and Jacobson [ 15 ] measure muscular strength for chronic kidney disease patients. Self-reported measure of pain is included in two reviews [ 13 , 32 ] and perceived stress [ 24 ].
Anxiety outcome measures in the quantitative reviews include Y-BOCS, HAS, IPAT, TAS, ACL, STAI, and SNAQ (see Box 3 ). In general, review results show small reduction in means for yoga groups versus control groups, although the study design varies. One nonrandomized controlled study ( n = 71) reports anxiety neurosis (HAS) decreases with yoga treatment versus placebo capsule SMD 0.89 (95% CI, 0.34 to 1.44; P = 0.001). A smaller randomized control trial measures Y-BOCS ( n = 22) reports SMD 1.10 (95% CI, − 0.02 to 2.22; P = n.r). In patients with cancer, a number of yoga interventions decrease anxiety scores (HADS, PSS, STAI SOSI, POMS, and SCL-90-R). One study reports a decrease of anxiety of SMD −0.76 (95% CI, − 1.34 to − 0.19; P = 0.009) in comparison to wait-list controls. In the two reviews that assess clinical anxiety as an outcome ( n = 1087), results range from having no beneficial effect on STAI scores SMD 0.33 (95% CI, −0.31 to 0.97) to a significant effect size of SMD −4.78 (95% CI, − 5.83 to − 3.74; P = n.r) on HADS and PSS validated questionnaires. Variations in scientific characteristics including the type and duration of intervention and size of samples may account for the variation in results. Weekly Tibetan yoga showed no benefit, while integrated yoga methods including asana, pranayama, and guided relaxation for 90 minutes per week show the greatest benefit in anxious participants.
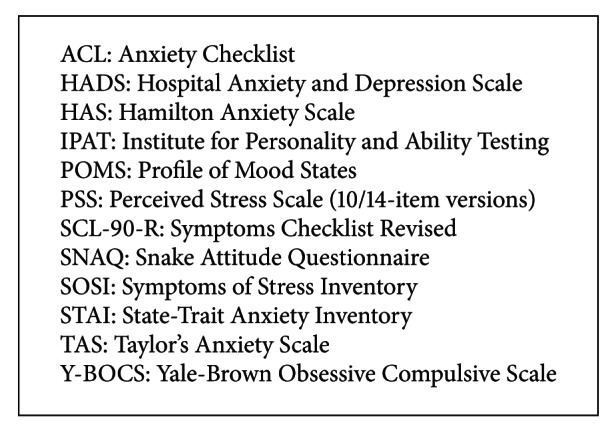
Summary of anxiety outcome measures.
In pain reviews, Gerritsen et al. review conservative treatment outcomes for carpal tunnel syndrome and report no significant differences in pain after 8 weeks of yoga intervention. Smith et al. [ 33 ] suggest that women receiving yoga report increased satisfaction with pain relief, increased satisfaction with the childbirth experience with reduced pain intensity outcomes in self-reported visual analogue scales (VASTC, MCQ, VASPS) of MD −6.12 (95% CI, −11.77 to − 0.47; P = 0.034) in latent phase labor versus usual care ( n = 66). See Box 4 for summary of measures for pain outcomes.
Summary of outcome measures for pain.
In asthmatic populations, one small study ( n = 36) reports a decrease in exacerbations (episodes per week) WMD −1.27 (95% CI, −2.26 to 0.28) following yoga breathing techniques, although results are not statistically significant [ 29 ]. The hypothesis that yoga breathing can reduce asthmatic episodes is neither confirmed nor refuted with results and further randomized controlled trials are requested.
In one study of epileptic patients ( n = 20), sahaja yoga intervention (versus sham yoga) increases probability of being seizure-free following six months of treatment by 40% with OR 14.54 (95% CI, 0.67 to 316.69; P = 0.089). The same study shows a greater than 50% reduction of seizure duration after six months in 7 of 10 yoga participants versus 0 of 10 sham yoga participants, OR 45.00 (95% CI, 2.01 to 1006.75; P = 0.016). The review author includes a second study that compares Acceptance Commitment Therapy (ACT) and yoga in-seizure outcomes. Five of 10 ACT participants versus 4 of 8 yoga participants are seizure-free after six months, with 50% or greater reduction in seizure duration in 6 of 10 (ACT) and 4 of 8 (yoga) groups, respectively. The review authors conclude that no reliable conclusions can be drawn regarding the efficacy of yoga for treatment of epilepsy due to the small number and size of studies.
In a review on chronic kidney disease populations, a small yoga study ( n = 37) does not show any significant increase in muscular strength for yoga versus control (no exercise/placebo exercise). This review studies a special population in which yoga-related studies are limited.
3.5. Subgroup Analysis
The most commonly cited health outcomes in yoga research are self-reported measures in pain (7 reviews), anxiety (6 reviews), and diabetes management (3 reviews). Five reviews measuring pain outcomes after yoga intervention report positive results. Iyengar (9 reviews), Hatha (7 reviews), and Restorative yoga (5 reviews) through instructor-led sessions (17 reviews) are most common in yoga interventions by type. Six positive effects are concluded in each of the groups of Hatha and Iyengar systematic reviews.
The Büssing et al. review includes meta-analyses on effects sizes for pain according to study design, duration of treatment, quality of study, and type of pain condition. Results suggest that randomized controlled trials with SMD −0.82 (95% CI, −1.20 to 0.53) and higher quality evidence SMD −0.88 (95% CI, 1.55 to −0.21) have marginally better pain outcomes than overall effects at −0.74 (95% CI, −0.97 to −0.52), while treatment duration appears to be similar to these overall effects in short, medium, and long interventions. Authors suggest improvements are most consistent for back pain and rheumatoid arthritic conditions. The remaining reviews do not provide enough data to perform subgroup analyses for gender, age, setting, or physiological intensity of yoga intervention.
4. Discussion
4.1. summary of main results.
The following 13 chronic health conditions in adult populations are included in this overview: anxiety, arthritis, asthma, carpal tunnel syndrome, diabetes, epilepsy, fibromyalgia, hypertension, kidney disease, metabolic syndrome, pain, psychological health in cancer patients, and psychiatric disorders. Acute health conditions are included for women in pregnancy, labor, and menopause.
4.1.1. Interventions and Outcomes
Systematic reviews list some components of yoga interventions: breathing exercises (pranayama), physical postures (asanas), meditation (dhyana) and some yoga philosophy including sahaja (spontaneous movement), yama (personal restraint), and niyama (observance of yoga) teachings. Inconsistent reporting of changes in effect sizes of yoga by intervention type, delivery mechanism, setting, frequency, or duration of sessions highlights a serious gap in the literature and serious limitation in the overview findings. Of 13 systematic reviews that report geographical location, all include data collected from patients in North America, five include participants from Asia, and three reviews include studies from Europe. Fifteen reviews did not provide information on the setting of the intervention. Nine systematic reviews included delivery in a clinic or hospital setting, while two include a home-based intervention and one community-based intervention.
As yoga research remains in the early stages of development, researchers appear to be more concentrated on outcome effects with clinical endpoints. However, traditional yoga practitioners claim that positive influence occurs in several health-related areas such as eliminating alcohol use, encouraging vegetarian diets, and providing an opportunity to increase social cohesion and positive group effects. These outcomes could relate more to mediating effects of yoga and warrant further investigation.
4.1.2. Unclear Effects of Yoga—15 Systematic Reviews
The following outcomes were associated with unclear effects following yoga intervention: anxiety [ 18 , 19 ], arthritis [ 14 , 23 ], asthma [ 29 ], body mass index [ 9 ], diabetes management [ 8 , 16 ], muscular strength [ 15 ], epilepsy [ 30 ], hypertension [ 12 ], and in pain for the elderly population [ 25 ]. Conclusions for menopause and carpal tunnel syndromes were split between positive and unclear effects. The more recent reviews in both instances show positive effects.
4.1.3. Positive Effects of Yoga—11 Systematic Reviews
Seven of the systematic reviews assess pain management as a primary outcome. Of these reviews, 5 authors conclude positive effects of yoga [ 10 , 20 , 28 , 31 , 33 ]. Positive results for the treatment fibromyalgia are noted in one systematic review [ 20 ]. Potential improvements for anxiety and quality of life in cancer patients are noted in two reviews [ 22 , 33 ]. One systematic review in psychiatric disorders concludes that yoga may be an effective and far less toxic adjunct treatment option for severe mental illness to prevent weight gain and patients' risk for cardiovascular disease [ 11 ].
4.1.4. Adverse Effects of Yoga—No Systematic Reviews
Systematic reviews universally report that yoga is safe and no adverse effects of yoga treatment are reported. As yoga therapy in the reviews was usually instructor-led in a clinical setting, yoga delivered without a trained instructor may increase risk of injury and other adverse events.
4.1.5. Size of Effect
In pooled analyses, statistical data report positive effects in five of six primary health outcomes for pain and various psychiatric disorders (depression, anxiety, PTSD, and schizophrenia). Effect sizes range from SMD −0.54 (95% CI, − 0.96 to − 0.11; P = 0.01) for pain in fibromyalgia patients (VAS) and SMD −3.25 (95% CI, − 5.36 to − 1.14; P = 0.002) in various psychiatric disorders (BDI, HADS, etc.). In the first instance, water yoga and awareness of yoga versus waitlist and treatment shows benefit. Ten studies using integrated yoga, Sudarshan, Kriya, Hatha, and Iyengar techniques favor yoga over other treatments and control groups, although the details are not reported. Most of the systematic reviews cite methodological weaknesses for unclear results, attributing this to small sample sizes and limited numbers of high-quality studies available for review. To investigate the impact of study size and quality on yoga's effect size on health outcomes, see Figure 2 . Although limited by six quantitative data points, it does not appear that study size correlates with yoga's size of effect.
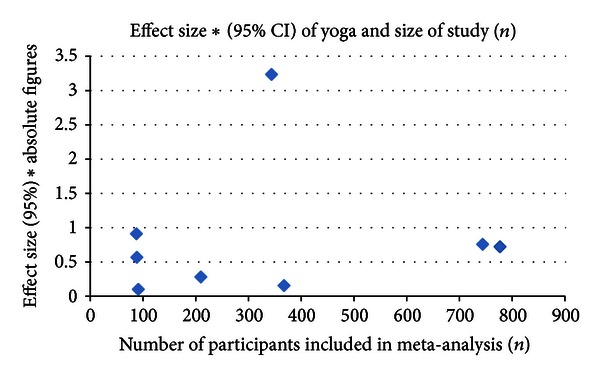
Effect size of yoga in comparison to study size.
4.2. Limitations of This Review
4.2.1. data characteristics.
The quality and quantity of evidence is a limitation to this overview. Though the quality of systematic reviews is high (9.4 AMSTAR), the quality of evidence included in reviews is generally low (GRADE). Important variables such as population statistics including gender, age, duration of interventions, comorbidities, and socioeconomic status are often not reported, limiting the potential for subgroup and meta-analyses. Of the primary and secondary outcome measures reviewed, no reports for all-cause mortality, hospital referral rates, cost effectiveness, or psychosocial behavioral changes are included which suggests at least four areas of potential investigation.
In two reviews that assess publication bias, one funnel plot that includes pain outcomes [ 10 ] did not reveal any significant symmetry, while the other review for psychiatric disorders indicates an asymmetric plot and publication bias [ 11 ]. The remaining 24 reviews do not provide results of Egger's regression, funnel plot, or critical analysis of publication bias; therefore, the degree to which positive outcomes are influenced by publication bias is not known.
As all reports are written in English and the majority of reviews found on electronic databases include studies from the Western hemisphere, it is possible that existing reviews have been missed. The transferability of results may be limited due to only partial descriptions of interventions such as asana, pranayama, and meditative techniques. A broader definition of “systematic review” might increase the number of reviews included from diverse backgrounds, though strict criteria in terms of systematic review quality limits the inclusion of low-quality reports. Missing data for follow-up measures, characteristics of yoga intervention, and components of yoga therapy limit the confidence and number of conclusions that can be drawn, though this lack of data may be due to weakness in sources from primary studies and not necessarily a flaw in systematic review methodology.

4.2.2. Sources of Heterogeneity
Review authors identify types of yoga intervention, population characteristics, outcome measures, and study designs as sources of heterogeneity. As a result of this heterogeneity, most reviews consider independent studies in their analyses. Results are pooled in only six instances, where statistical heterogeneity was found in three cases and one did not report. As a complex intervention, some heterogeneity is inevitable with yoga and in fact desirable to replicate real-life circumstances. Study designs could be improved to focus on specific interventions.
4.2.3. Duplication of Primary Studies
Duplication of primary studies appears in 40 cases across 17 reviews (yoga-only reviews: [ 8 , 11 , 14 , 18 , 21 , 27 , 28 , 53 ]; multiple interventions: [ 13 , 16 , 17 , 23 – 26 , 31 , 33 ]). The highest incidence of primary study overlap occurs in pain [ 25 , 53 ] and menopause reviews [ 17 , 21 ]. In further analysis, when the Garfinkel studies are removed, two systematic reviews are eliminated from this review [ 23 , 26 ]. For pain, the more recent Bussing study concludes positive effects with yoga intervention, while Morone concludes unclear effects using similar studies. The removal of these two studies from the pool of results does not appear to change the net positive effects of yoga for pain conditions. In menopause, although 4 of 7 articles in each review are duplicates, authors' conclude different results: Lee et al. [ 21 ] suggest unclear effects of yoga, while Innes et al. [ 17 ] suggest positive effects of yoga on menopausal symptoms.
4.2.4. Date of Search
The rate of publication for yoga systematic reviews is increasing rapidly. In an updated search (March 1, 2013), nine of 17 new titles pass initial screening for inclusion. Screening of abstracts identifies seven of these reviews that would need to be collected for further inclusion analysis, of which three focus on adult cancer [ 54 – 56 ], one on chronic obstructive pulmonary disease [ 57 ], one for depression [ 58 ], one for anxiety [ 59 ], and one for phantom limb pain [ 60 ]. These reviews suggest positive impact of yoga for primary outcomes with no adverse effects, though authors unanimously state that more and better-quality research is needed. In a recent overview of yoga, authors conclude there is relatively high-quality evidence to suggest that yoga may have beneficial effects for pain-associated disability and mental health [ 53 ], conclusions that are further substantiated by this overview.
5. Conclusion
5.1. implications for practice.
Yoga for treatment of acute and chronic health conditions is not likely to exacerbate symptoms in an experimental setting, although clear effect sizes and probabilities for beneficial outcomes in a specified population are not available at this time. Cumulative findings indicate that Hatha and Restorative yoga have the highest correlation with positive outcomes for managing pain symptoms, anxiety, and depression. Home study and instructor-led yoga (practiced 60 minutes 3 times per week) appear to have similar positive impacts.
5.2. Implications for Research
This overview adds a comprehensive and methodical examination of yoga interventions in adult populations for treatment of acute and chronic health conditions. The findings do support earlier claims that depression, pain, and anxiety could be positively affected by yoga intervention, though evidence is positive but less significant in populations with cardiovascular risk factors, fibromyalgia, or autoimmune disease. It is evident that systematic reviewers and primary research teams should include more information with regards to the characteristics of yoga intervention, including type, frequency, duration, and physiological intensity of practice. Video-led yoga needs to be explored further as one review includes this delivery mechanism and yields positive results, though the sample size is small and adverse effects are not measured. Health outcomes in other adult populations for asthma, arthritis, carpal tunnel syndrome, epilepsy, diabetes, kidney disease, and menopausal women remain uncertain. Two earlier reviews (before June 1, 2012) and three newer systematic reviews investigate yoga's effect for adult cancer. These papers should inform future investigations in terms of patient-relevant outcomes such as pain management, immunological responses, anxiety, and health-related quality of life.
Yoga is a complex intervention that includes physical movement, breathing techniques, meditation, visualization and philosophical underpinnings that may influence attitudes, beliefs and social interaction. A new hypothesis informed by results of this overview, together with an emerging trend of increased yoga research for cancer populations, suggest the complex and varied nature of yoga may better serve patients who experience a cluster of symptoms that include psychological distress, fatigue, pain and a compromised health-related quality of life. Further study into these effects should include analysis of adherence rates, outcomes in morbidity, mortality rates, disease progression markers, physical function and long-term follow-up.
Acknowledgments
This overview was performed in partial requirement of a research doctorate in Evidence-Based Health Care, Department of Continuing Education, Kellogg College at the University of Oxford. Special thanks are due to Professor Mike Clarke and other Evidence-Based Health Care faculty and students for their support in developing the question and research methods.
Electronic Search Protocol
Identification of Relevant Databases:
Cochrane Library
The Electronic Search Performed in May 2012
Online access via SOLO [ http://solo.bodleian.ox.ac.uk with SSO password]
Enter free text terms, MeSH descriptors and set filters
Scan results for relevant titles
Scan titles for relevant abstracts
Scan abstract for relevant review articles
Save citations with abstracts to a file and transfer to reference management database [sente]
Collect relevant articles in.pdf and save to file on external and internal computer hard drives under review identification label
Store the external hard drive in separate location under lock and key. Two key holders.
Cochrane Database of Systematic Reviews (via Cochrane Library, Wiley)
1 or 2 or 3 or 4 or 5 or 6.
MEDLINE (1946-), EMBASE (1974-), AMED (1985-), PsycINFO (1960-) (via OVID)
MeSH descriptor; Meditation; Relaxation Therapy; Mind Body Medicine explode all trees
(yoga OR yogi* OR asana OR pranayama OR dhyana OR meditation)
MeSH descriptor; Meta-analysis; Review explode all trees
(systematic OR review OR meta-analysis)
CINAHL (via EBSCOHost)
limit: publication type (meta-analysis); exclude (MEDLINE results)
IndMED ( http://indmed.nic.in ); CAMQuest ( http://www.cam-quest.org/en/ )
Scopus (via SciVerse; Elsevier)
limit: publication type (review)
- 1. Dangerfield A. Yoga wars. BBC News Magazine, 2009, http://news.bbc.co.uk/1/hi/7844691.stm .
- 2. Taylor M. What is yoga therapy? An IAYT definition. Yoga Therapy in Practice, 2012, http://www.iayt.org/site_Vx2/publications/articles/IAYT%20Yoga%20therapy%20definition%20Dec%202007%20YTIP.pdf .
- 3. Macy D. Yoga Journal Releases 2008 “Yoga in America” market study. Yoga Journal Magazine, 2008, http://www.yogajournal.com/advertise/press_releases/10 .
- 4. National Health Service. NHS: your health, your choices. A Guide to Yoga, 2012, http://www.nhs.uk/livewell/fitness/pages/yoga.aspx .
- 5. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS Medicine. 2009;6(6)e1000097 [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Field T. Yoga clinical research review. Complementary Therapies in Clinical Practice. 2011;17(1):1–8. doi: 10.1016/j.ctcp.2010.09.007. [ DOI ] [ PubMed ] [ Google Scholar ]
- 7. Ernst E, Lee MS. How effective is yoga? A concise overview of systematic reviews. Focus on Alternative and Complementary Therapies. 2010;15(4):274–279. [ Google Scholar ]
- 8. Aljasir B, Bryson M, Al-Shehri B. Yoga practice for the management of type II diabetes mellitus in adults: a systematic review. Evidence-Based Complementary and Alternative Medicine. 2010;7(4):399–408. doi: 10.1093/ecam/nen027. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 9. Anderson JG, Taylor AG. The metabolic syndrome and mind-body therapies: a systematic review. Journal of Nutrition and Metabolism. 2011;2011:8 pages. doi: 10.1155/2011/276419.276419 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 10. Büssing A, Ostermann T, Lüdtke R, Michalsen A. Effects of yoga interventions on pain and pain-associated disability: a meta-analysis. Journal of Pain. 2012;13(1):1–9. doi: 10.1016/j.jpain.2011.10.001. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Cabral P, Meyer HB, Ames D. Effectiveness of yoga therapy as a complementary treatment for major psychiatric disorders: a meta-analysis. Primary Care Companion For Central Nervous System Disorders. 2011;13(4) doi: 10.4088/PCC.10r01068. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 12. Dickinson HO, Campbell F, Beyer FR, et al. Relaxation therapies for the management of primary hypertension in adults: a Cochrane review. Journal of Human Hypertension. 2008;22(12):809–820. doi: 10.1038/jhh.2008.65. [ DOI ] [ PubMed ] [ Google Scholar ]
- 13. Gerritsen AA, De Krom MCTFM, Struijs MA, Scholten RJPM, De Vet HCW, Bouter LM. Conservative treatment options for carpal tunnel syndrome: a systematic review of randomised controlled trials. Journal of Neurology. 2002;249(3):272–280. doi: 10.1007/s004150200004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Haaz S, Bartlett SJ. Yoga for arthritis: a scoping review. Rheumatic Disease Clinics of North America. 2011;37(1):33–46. doi: 10.1016/j.rdc.2010.11.001. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 15. Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database of Systematic Reviews. 2011 doi: 10.1002/14651858.CD003236.pub2.CD003236 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 16. Innes KE, Vincent HK. The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus: a systematic review. Evidence-Based Complementary and Alternative Medicine. 2007;4(4):469–486. doi: 10.1093/ecam/nel103. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 17. Innes KE, Selfe TK, Vishnu A. Mind-body therapies for menopausal symptoms: a systematic review. Maturitas. 2010;66(2):135–149. doi: 10.1016/j.maturitas.2010.01.016. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 18. Kirkwood G, Rampes H, Tuffrey V, Richardson J, Pilkington K. Yoga for anxiety: a systematic review of the research evidence. British Journal of Sports Medicine. 2005;39(12):884–891. doi: 10.1136/bjsm.2005.018069. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Krisanaprakornkit T, Krisanaprakornkit W, Piyavhatkul N, Laopaiboon M. Meditation therapy for anxiety disorders. Cochrane Database of Systematic Reviews. 2006;(1) doi: 10.1002/14651858.CD004998.pub2.CD004998 [ DOI ] [ PubMed ] [ Google Scholar ]
- 20. Langhorst J, Klose P, Dobos GJ, Bernard K, Häuser W. Efficacy and safety of meditative movement therapies in fibromyalgia syndrome: a systematic review and meta-analysis of randomized controlled trials. Rheumatology International. 2012;33(1):193–207. doi: 10.1007/s00296-012-2360-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Lee MS, Kim JI, Ha JY, Boddy K, Ernst E. Yoga for menopausal symptoms: a systematic review. Menopause. 2009;16(3):602–608. doi: 10.1097/gme.0b013e31818ffe39. [ DOI ] [ PubMed ] [ Google Scholar ]
- 22. Lin KY, Hu YT, Chang KJ, Lin HF, Tsauo JY. Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. Evidence-Based Complementary and Alternative Medicine. 2011;2011 doi: 10.1155/2011/659876.659876 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 23. Mahendira D, Towheed TE. Systematic review of non-surgical therapies for osteoarthritis of the hand: an update. Osteoarthritis and Cartilage. 2009;17(10):1263–1268. doi: 10.1016/j.joca.2009.04.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 24. Marc I, Toureche N, Ernst E, et al. Mind-body interventions during pregnancy for preventing or treating women’s anxiety. Cochrane Database of Systematic Reviews. 2011;(7) doi: 10.1002/14651858.CD007559.pub2.CD007559 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 25. Morone NE, Greco CM. Mind-body interventions for chronic pain in older adults: a structured review. Pain Medicine. 2007;8(4):359–375. doi: 10.1111/j.1526-4637.2007.00312.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 26. Muller M, Tsui D, Schnurr R, Biddulph-Deisroth L, Hard J, MacDermid JC. Effectiveness of hand therapy interventions in primary management of carpal tunnel syndrome: a systematic review. Journal of Hand Therapy. 2004;17(2):210–228. doi: 10.1197/j.jht.2004.02.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Pilkington K, Kirkwood G, Rampes H, Richardson J. Yoga for depression: the research evidence. Journal of Affective Disorders. 2005;89(1–3):13–24. doi: 10.1016/j.jad.2005.08.013. [ DOI ] [ PubMed ] [ Google Scholar ]
- 28. Posadzki P, Ernst E, Terry R, Lee MS. Is yoga effective for pain? A systematic review of randomized clinical trials. Complementary Therapies in Medicine. 2012;19(5):281–287. doi: 10.1016/j.ctim.2011.07.004. [ DOI ] [ PubMed ] [ Google Scholar ]
- 29. Ram FSF, Holloway EA, Jones PW. Breathing retraining for asthma. Respiratory Medicine. 2003;97(5):501–507. doi: 10.1053/rmed.2002.1472. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Ramaratnam S, Sridharan K. Yoga for epilepsy. Cochrane Database of Systematic Reviews. 2000;(2) doi: 10.1002/14651858.CD001524.CD001524 [ DOI ] [ PubMed ] [ Google Scholar ]
- 31. Slade SC, Keating JL. Unloaded movement facilitation exercise compared to no exercise or alternative therapy on outcomes for people with nonspecific chronic low back pain: a systematic review. Journal of Manipulative and Physiological Therapeutics. 2007;30(4):301–311. doi: 10.1016/j.jmpt.2007.03.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 32. Smith KB, Pukall CF. An evidence-based review of yoga as a complementary intervention for patients with cancer. Psycho-Oncology. 2009;18(5):465–475. doi: 10.1002/pon.1411. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Smith CA, Levett KM, Collins CT, Crowther CA. Relaxation techniques for pain management in labor. Cochrane Database of Systematic Reviews. 2011 doi: 10.1002/14651858.CD009514.CD009514 [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Alexander GK, Taylor AG, Innes KE, Kulbok P, Selfe TK. Contextualizing the effects of yoga therapy on diabetes management: a review of the social determinants of physical activity. Family and Community Health. 2008;31(3):228–239. doi: 10.1097/01.FCH.0000324480.40459.20. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 35. Beddoe AE, Lee KA. Mind-Body interventions during pregnancy. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2008;37(2):165–175. doi: 10.1111/j.1552-6909.2008.00218.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 36. Brotto LA, Mehak L, Kit C. Yoga and sexual functioning: a review. Journal of Sex and Marital Therapy. 2009;35(5):378–390. doi: 10.1080/00926230903065955. [ DOI ] [ PubMed ] [ Google Scholar ]
- 37. Burgess J, Ekanayake B, Lowe A, Dunt D, Thien F, Dharmage SC. Systematic review of the effectiveness of breathing retraining in asthma management. Expert Review of Respiratory Medicine. 2011;5(6):789–807. doi: 10.1586/ers.11.69. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: a systematic review. Journal of the American Board of Family Practice. 2005;18(6):491–519. doi: 10.3122/jabfm.18.6.491. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Kozasa EH, Harumi E, Hachul H, et al. Mind-body interventions for the treatment of insomnia: a review. Revista Brasileira de Psiquiatria. 2010;32(4):437–443. doi: 10.1590/s1516-44462010000400018. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Krisanaprakornkit T, Ngamjarus C, Witoonchart C, Piyavhatkul N. Meditation therapies for attention-deficit/hyperactivity disorder (ADHD) Cochrane Database of Systematic Reviews. 2010;6 doi: 10.1002/14651858.CD006507.pub2.CD006507 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Lynton H, Kligler B, Shiflett S. Yoga in stroke rehabilitation: a systematic review and results of a pilot study. Topics in Stroke Rehabilitation. 2007;14(4):1–8. doi: 10.1310/tsr1404-1. [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Mehta P, Sharma M. Yoga as a complementary therapy for clinical depression. Complementary Health Practice Review. 2010;15(3):156–170. [ Google Scholar ]
- 43. Posadzki P, Ernst E. Yoga for asthma? A systematic review of randomized clinical trials. Journal of Asthma. 2011;48(6):632–639. doi: 10.3109/02770903.2011.584358. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Shen YHA, Nahas R. Complementary and alternative medicine for treatment of irritable bowel syndrome. Canadian Family Physician. 2009;55(2):143–148. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 45. Steurer-Stey C, Russi EW, Steurer J. Complementary and alternative medicine in asthma—do they work? A summary and appraisal of published evidence. Swiss Medical Weekly. 2002;132(25-26):338–344. doi: 10.4414/smw.2002.09972. [ DOI ] [ PubMed ] [ Google Scholar ]
- 46. Towheed TE. Systematic review of therapies for osteoarthritis of the hand. Osteoarthritis and Cartilage. 2005;13(6):455–462. doi: 10.1016/j.joca.2005.02.009. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Vickers AJ, Smith C. Analysis of the evidence profile of the effectiveness of complementary therapies in asthma: a qualitative survey and systematic review. Complementary Therapies in Medicine. 1997;5(4):202–209. [ Google Scholar ]
- 48. Oxman AD. Checklists for review articles. British Medical Journal. 1994;309(6955):648–651. doi: 10.1136/bmj.309.6955.648. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 49. Broad WJ. The Science of Yoga: The Myths and the Rewards. New York, NY, USA: Simon & Schuster; 2012. [ Google Scholar ]
- 50. McCall T. Yoga as Medicine. New York, NY, USA: Bantam Dell a Division of Random House; 2007. [ Google Scholar ]
- 51. Guyatt G, GRADE working group Guidelines-best practices using the GRADE framework. 2012, http://www.gradeworkinggroup.org/publications/JCE_series.htm .
- 52. Shea BJ, Grimshaw JM, Wells GA, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology. 2007;7, article 10 doi: 10.1186/1471-2288-7-10. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 53. Büssing A, Michalsen A A, Khalsa SBS, Telles S, Sherman KJ. Effects of yoga on mental and physical health: a short summary of reviews. Evidence-Based Complementary and Alternative Medicine. 2012;2012:7 pages. doi: 10.1155/2012/165410.165410 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 54. Côté A, Daneault S. Effect of yoga on patients with cancer: our current understanding. Canadian Family Physician. 2012;58(9):475–479. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 55. Mishra SI, Scherer RW, Snyder C, Geigle PM, Berlanstein DR, Topaloglu O. Exercise interventions on health-related quality of life for people with cancer during active treatment. Cochrane Database of Systematic Reviews. 2012 doi: 10.1002/14651858.CD008465.pub2.CD008465 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 56. Stan DL, Collins NM, Olsen MM, Croghan I, Pruthi S. The evolution of mindfulness-based physical interventions in breast cancer survivors. Evidence-Based Complementary and Alternative Medicine. 2012;2012:15 pages. doi: 10.1155/2012/758641.758641 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 57. Holland AE, Hill CJ, Jones AY, McDonald CF. Breathing exercises for chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews. 2012 doi: 10.1002/14651858.CD008250.pub2.CD008250 [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 58. D'Silva S, Poscablo C, Habousha R, Kogan M, Kligler B. Mind-body medicine therapies for a range of depression severity: a systematic review. Psychosomatics. 2012;53(5):407–423. doi: 10.1016/j.psym.2012.04.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Vøllestad J, Nielsen MB, Nielsen GH. Mindfulness and acceptance-based interventions for anxiety disorders: a systematic review and meta-analysis. The British Journal of Clinical Psychology. 2012;51(3):239–260. doi: 10.1111/j.2044-8260.2011.02024.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Moura VL, Faurot KR, Gaylord SA, et al. Mind-body interventions for treatment of phantom limb pain in persons with amputation. American Journal of Physical Medicine and Rehabilitation. 2012;91(8):701–714. doi: 10.1097/PHM.0b013e3182466034. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (764.2 KB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry
Affiliation.
- 1 a Department of Psychology , University of Connecticut , Storrs , CT , USA.
- PMID: 25559560
- DOI: 10.1080/17437199.2014.981778
Yoga is increasingly used in clinical settings for a variety of mental and physical health issues, particularly stress-related illnesses and concerns, and has demonstrated promising efficacy. Yet the ways in which yoga reduces stress remain poorly understood. To examine the empirical evidence regarding the mechanisms through which yoga reduces stress, we conducted a systematic review of the literature, including any yoga intervention that measured stress as a primary dependent variable and tested a mechanism of the relationship with mediation. Our electronic database search yielded 926 abstracts, of which 71 were chosen for further inspection and 5 were selected for the final systematic review. These five studies examined three psychological mechanisms (positive affect, mindfulness and self-compassion) and four biological mechanisms (posterior hypothalamus, interleukin-6, C-reactive protein and cortisol). Positive affect, self-compassion, inhibition of the posterior hypothalamus and salivary cortisol were all shown to mediate the relationship between yoga and stress. It is striking that the literature describing potential mechanisms is growing rapidly, yet only seven mechanisms have been empirically examined; more research is necessary. Also, future research ought to include more rigorous methodology, including sufficient power, study randomisation and appropriate control groups.
Keywords: clinical interventions; methodology; mindfulness; stress reduction; yoga.
Publication types
- Systematic Review
- C-Reactive Protein / analysis
- Hydrocortisone / analysis
- Interleukin-6 / analysis
- Meditation*
- Stress, Psychological / blood
- Stress, Psychological / psychology
- Stress, Psychological / therapy*
- Treatment Outcome
- IL6 protein, human
- Interleukin-6
- C-Reactive Protein
- Hydrocortisone
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- For authors
- Browse by collection
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 11, Issue 12
- Effectiveness and safety of yoga to treat chronic and acute pain: a rapid review of systematic reviews
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- http://orcid.org/0000-0002-2698-9211 Roberta Crevelário de Melo 1 ,
- http://orcid.org/0000-0003-4639-4060 Aline Ângela Victoria Ribeiro 2 ,
- http://orcid.org/0000-0002-5038-6808 Cézar D Luquine Jr 1 ,
- Maritsa Carla de Bortoli 1 ,
- Tereza Setsuko Toma 1 ,
- Jorge Otávio Maia Barreto 3
- 1 Center for Health Technologies SUS/SP, Instituto de Saúde , Secretaria da Saude do Estado de Sao Paulo , Sao Paulo , Brazil
- 2 Institute of Philosophy and Human Sciences , State University of Campinas , Campinas , Brazil
- 3 Fundacao Oswaldo Cruz , Brasília , Brazil
- Correspondence to Dr Jorge Otávio Maia Barreto; jorgeomaia{at}hotmail.com
Background Pain is a sensation of discomfort that affects a large part of the population. Yoga is indicated to treat various health conditions, including chronic and acute pain.
Objective To evaluate the effectiveness and safety of yoga to treat acute or chronic pain in the adult and elderly population.
Study selection A rapid review was carried out, following a protocol established a priori. Searches were carried out in September 2019, in six databases, using PICOS and MeSH (Medical Subject Headings) and DeCS (Descritores em Ciências da Saúde) terms. Systematic reviews were included, and methodological quality was assessed using Assessing the Methodological Quality of Systematic Reviews. The results were presented in a narrative synthesis.
Findings Ten systematic reviews were selected. Two reviews were assessed as of high methodological quality, two as of low quality, and six of critically low quality. Results were favourable to yoga compared with usual daily care, particularly in low back and cervical pain cases. There was little evidence about the superiority of yoga compared with active interventions (exercises, pilates or complementary and complementary medicine). It was also less consistent in pain associated with fibromyalgia, osteoarthritis, rheumatoid arthritis, carpal tunnel and irritable bowel syndromes. There was an improvement in the quality of life and mood of the participants, especially for yoga compared with usual care, exercises and waiting list.
Conclusions Overall, the results were favourable to yoga compared with usual care in low back and cervical pain cases. The evidence is insufficient to assert yoga’s benefits for other pain conditions, as well as its superiority over active interventions. The findings must be considered with caution, given their low methodological quality and the small samples in the primary studies reported in the included systematic reviews. Thus, more studies must be carried out to improve the reliability of the results.
- complementary medicine
- public health
- pain management
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. Not applicable.
This is an open access article distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited, appropriate credit is given, any changes made indicated, and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/ .
https://doi.org/10.1136/bmjopen-2020-048536
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
Strengths and limitations of this study
This research followed a validated methodological guideline.
Only the selection done duplicated and independently. The data extraction and quality assessment were performed by one reviewer and verified by another.
No analyses were performed on the overlap of primary studies of the included systematic reviews.
The systematic reviews included had their methodological quality assessed with the Assessing the Methodological Quality of Systematic Reviews tool.
This review report adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommendations.
Pain is a major biopsychosocial problem worldwide because it affects the quality of life of individuals and causes considerable economic impact. 1 Pain is a of subjective nature and can be described as an ‘unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage’. 2 Although there is still no consensus on the definition of pain, according to the International Association for the Study of Pain it can be classified as either acute (lasts from a few seconds to 30 days) or chronic (more than 3 months to several years). 3–5
In 2017, the USA, Germany, France, Italy, Spain, UK and Japan reported an estimated 119 619 121 cases of acute pain related to surgery, trauma or other disease conditions. 6 In the USA, acute pain was reported by 41 766 061 patients after surgery and by 34 068 366 patients with traumatic injury. Between the European countries studied, Germany and the UK registered the highest number of acute pain cases. 6
Pain is frequent in elderly people. Among residents from long-term care facilities, 49%–83% report that they were regularly in pain. 7 More than 63% of older patients seen in primary healthcare also complain about acute pain. These symptoms were responsible for 69% of the accounted disability in daily routine life activities. 7
A systematic review (SR) showed that low-back pain is the most prevalent, affecting 51%–84% of the general population, followed by cervical pain (15.4%–45.3%). 1 Pain can become a chronic condition that impacts an estimated 10%–55% of the population worldwide. 8–10 Accordingly, pain episodes in Europe, for example, compromise up to 3.0% of gross domestic product, with an annual cost higher than cancer and many heart diseases. 1
In this context, non-pharmacological therapies, such as yoga, have been indicated to manage acute or chronic pain. Yoga is an integrative mind–body practice of oriental origin that involves three main elements: body positions (asana), techniques for controlling and/or regulating breathing (pranayama), and meditation and/or relaxation (samyama). 11 Currently, there are several yoga types, which differ mainly due to variations in the intensity, difficulty and duration of the postures, in addition to variations in the meditation and breathing techniques. ‘Hatha yoga’ and ‘integrative yoga’ are the terms commonly used to refer to several types of yoga practice, including those most used in Western societies, such as Iyengar and Vinyasa yoga or Viniyoga. 11 Such yoga types have been used for many purposes, like physical rehabilitation and comprehensive care for emotionally traumatised individuals. 12
The number of people who practice yoga has been increasing in recent years in Western countries. For example, in the USA, a study reported that approximately 31 million adult Americans have already practised yoga for the prevention of diseases and back pain relief. 13 In Brazil, a survey carried out by the Ministry of Health (MoH) in 2004 showed that 14.6% of the municipalities and states offered yoga at that time, mainly in primary healthcare. 14 Also, yoga was incorporated into the National Policy of Integrative and Complementary Practices in Health, 14 which instituted the offer of traditional and complementary medicines in the Brazilian Unified Health System (SUS). 15 The incorporation of yoga in the SUS is officially justified by possible cognitive, musculoskeletal, endocrine and respiratory benefits. 15 16 For that reason, the number of healthcare providers offering yoga sessions in the SUS increased from 565 in 2017 to 7732 in 2019, as well as the number of patients assisted (from 3870 to 43 459, respectively). 17
Rapid review of SRs carried out by demand of the Brazilian MoH. Rapid reviews are appropriate to provide decision makers with the best available evidence in a short time. 18 A research protocol was previously prepared, describing the eligibility criteria, articles selection, data extraction and methodological quality assessment ( online supplemental file 1 ). This review adhered the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 reporting guidelines. 19
Supplemental material
Eligibility criteria.
The research question was developed following PICOS framework: P=adults and elderly with acute or chronic pain; I=yoga; C=usual treatment, placebo, or no treatment; O=reduction or control of acute or chronic pain and adverse events; S=SRs, with or without meta-analysis. Searches and selection of studies were guided by the following question: What is the effectiveness and safety of yoga practice to treat acute or chronic pain in an adult population, compared with usual treatments, placebo, or no treatment, based on the evidence of SRs?
We searched by SRs of randomised controlled trials (RCT), quasi-RCT, observational studies or qualitative studies, with or without meta-analysis, published in English, Spanish and Portuguese, with no restriction to publication date. Overviews, scoping reviews, integrative reviews, synthesis of evidence for policies, health technology assessment studies, economic assessment studies and primary studies were excluded. Studies that presented pain as a secondary outcome or did not present a clear report on the results were excluded.
Searches were carried out on 27 September 2019, by two researchers, in indexed databases PubMed, Health Systems Evidence (HSE), Epistemonikos, VHL (Virtual Health Library) Regional Portal, Health Evidence (HE) and Embase. The search strategies combined keywords from the PICOS acronym, using MeSH (Medical Subject Headings) terms in Pubmed and DeCS (Descritores em Ciências da Saúde) terms in the VHL, adapting them to HSE, Epistemonikos, HE and Embase. The terms used were: “yoga”, “acute pain”, “chronic pain”, “ioga”, “dolor agudo”, “dolor crónico”, “dor aguda” and “dor crônica”. The SR filter was used in three databases (PubMed, Epistemonikos, VHL Regional Portal) ( online supplemental file 2 ).
Study selection and data extraction
The SRs retrieved were uploaded to Rayyan reference management web application. 20 The screening process followed the steps of excluding duplicates and then reading titles and abstracts. The eligible articles were read in full. Those that did not meet the objectives of this rapid review were excluded. Using an Excel spreadsheet, the following data were extracted from the included studies: authorship, publication year, aims, intervention, comparators, results, limitations, conflicts of interest and last year searched. Both the study selection and data extraction were carried out by two reviewers independently. Conflicts were resolved by a third reviewer.
Quality assessment
Two reviewers independently assessed the methodological quality of studies with the Assessing the Methodological Quality of Systematic Reviews (AMSTAR 2) tool. 21 Assessment disagreements between reviewers were resolved through consensus. To classify the overall confidence in the results of the SRs, the ‘critical domains’ considered were the same suggest by the authors of AMSTAR 2 in their original article: study protocol (item 2); comprehensive search strategy (item 4); list of excluded studies with justification (item 7); adequate technique to assess the risk of bias in each study included in the review (item 9); appropriate methods for meta-analysis (item 11); risk of bias in each study when interpreting the results (item 13); and publication bias (item 15). Cohen’s kappa statistic was calculated to estimate each domain’s inter-rater reliability (IRR).
Synthesis of results
Results were analysed based on the effect size measures informed by the SRs (MD: means difference; RR: risk ratio; SMD: standardised means difference; 95% CI; I 2 : heterogeneity measure). A narrative synthesis of the results was prepared for each outcome about benefits and adverse events.
Patient and public involvement
No patients or public participated in any stage of this review. Results were presented to decision makers.
The PRISMA flow diagram shows the selection process ( figure 1 ). Searches yielded 693 references, of which 250 remained for screening of titles and abstracts after duplicates were removed. Records were excluded after screening because they were a duplicate (4.8% out of 250), full-text not available (1,2%) or for not meeting at least one of the eligibility criteria: outcome (40.4%), not an SR (27.6%), population (14%) or intervention (2,8%). Twenty-three reviews were read in full to check eligibility and 13 were excluded for the following reasons: not an SR, 22–29 not an yoga intervention 30–33 or necessary data unavailable for extraction. 34 Thus 10 SRs were included, 12 35–43 eight with meta-analysis ( online supplemental file 3 ).
- Download figure
- Open in new tab
- Download powerpoint
Study selection flow diagram, adapted from Preferred Reporting Items for Systematic Reviews and Meta-Analyses. 19
Studies characteristics
Primary studies included in the SRs were conducted in the USA (5), 35–39 India (4), 36–39 Sweden (3), 35 38 39 Germany (2), 36 39 China (2), 38 39 Korea (2), 38 39 England (2), 37 38 Brazil (2), 35 38 Spain (1) 35 and Turkey (1). 39 Five reviews did not present this information. 12 40–43
The studies included in the reviews analysed different types of yoga, the most frequent ones being yoga iyengar, 12 37 38 40 42 43 hatha yoga 37–39 42 43 and viniyoga, 37 38 40–43 yogic mind resonance technique, 39 yoga of awareness, 35 43 yoga‐based special techniques 37 yogic meditation 37 and two reviews did not specify a yoga type used. 12 40
Yoga was combined with home practice, 35–38 41–43 daily mostly, educational resources (booklets, guides, newsletters) about yoga 37 38 41–43 or pain, 37 CDs (Compact Disc) or DVDs (Digital Versatile Disc), 35 38 42 43 physiotherapy, 36 39 relaxation, 35 40 education, 40 occupational therapy sessions 37 and usual care. 37 38 41 42
The person responsible for the practice was mentioned to be an experienced yoga teacher, 36 37 42 43 but this information was not available for the majority of SRs included. 12 35 36 39–41
The duration of sessions ranged from 15 min 41 to 3 hours 12 and frequency varied from one 12 to seven times 43 per week. The follow-up of participants continued for the minimum of 1 42 and maximum of 24 38 weeks.
Comparisons were made to usual care, 12 35–37 40 42 educational interventions, 12 37 38 41–43 standard medical care 42 ; exercises, 12 37–39 41 and delayed treatment. 35 Yoga interventions were also compared with waiting list controls, mostly unspecified, 12 37 40 43 but in one case there was a subsequent offer of intervention or treatment at some point or at the end of the study. 38 Other integrative practices such as Tai-chi or pilates 39 or no intervention 12 40 were compared as well.
SRs described results on the following outcomes: pain, functional capacity, psychosocial outcomes, quality of life, specific back deficiency, overall clinical improvement and adverse events. The effectiveness of yoga was assessed in reducing low-back pain 12 38 41 42 ; cervical pain 36 39 ; pain associated with fibromyalgia 35 ; pain associated with irritable bowel syndrome 12 ; pain associated with carpal tunnel syndrome 12 ; pain caused by musculoskeletal conditions 43 ; and chronic non-malignant pain. 40
Pain after yoga was measured using the following scales and questionnaires: Visual Analogue Scale 12 35–40 42 43 ; Numeric Rating Scale 12 38 39 42 43 ; Aberdeen Back Pain Scale 12 37 38 42 ; McGill Pain Questionnaire and variations 12 38 39 42 ; Pain Bothersomeness Scales 12 42 43 ; Pain Analogue Scale 36 ; Pain Diary 12 ; Joint tenderness and hand pain during activity 40 ; Brief Pain Inventory 38 ; Pain Disability Index 38 ; Simple Descriptive Pain Intensity Scale 43 ; Neck Pain and Disability Scale 39 ; Neck pain-related disability 36 ; Oswetry disability index pain 12 37 ; Northwick Park Questionnaire 39 ; Pain and Disability Chronic Pain Grade Scale 39 ; Pressure Pain Threshold 39 ; Pain and physical function Western Ontario and McMaster Universities 40 ; Symptom bothersomeness. 40
Two SRs were of high methodological quality, 37 38 two were assessed as low quality, 35 42 and six of critically low quality. 12 36 39–41 43 Overall IRR before consensus was estimated from an average of Cohen’s kappa (κ) through AMSTAR 2 domains (mean κ=0.59). Figure 2 details the assessment of each AMSTAR 2 item.
Summary of quality using Assessing the Methodological Quality of Systematic Reviews.
Yoga reduced low-back pain, 12 37 38 41 42 cervical pain, 36 39 pain associated with fibromyalgia, 35 pain associated with irritable bowel syndrome, 12 pain associated with carpal tunnel syndrome, 12 pain caused by musculoskeletal conditions 43 and chronic non-malignant pain. 40
Low-back pain
Six SRs evaluated the effectiveness of yoga in reducing low-back pain in patients with chronic pain 12 37 38 41 42 or low-back pain in general. 43 Comparisons were made to usual care, exercise, educational interventions, attention control and waiting list individuals.
Compared with usual care, medical care or education, 42 yoga decreased low-back pain in the short term, that is, right after the intervention and 12 weeks after randomisation, (6 RCT, 584 patients, SMD=−0.48; 95% CI −0.65 to −0.31; I 2 =0%) and in the long term a year after randomisation (6 RCT, 564 patients, SMD=−0.33; 95% CI −0.59 to −0.07; I 2 =48%). In comparison to attention control or waiting list, 38 yoga was associated with moderately larger effects on short term, 1 to <6 months (5 RCT, 770 patients, pooled difference=−1.10; 95% CI −1.77 to −0.42; I 2 =74%) and intermediate term, ≥6 to <12 months (2 RCT, 271 patients, pooled difference=−1.17; 95% CI −1.91 to −4.44; I 2 =26%). Also, yoga showed a intermediate-term effect of large magnitude (26–32 weeks) for non-specific chronic low-back pain control (2 trials, 88 participants, pooled SMD=0.92; 95% CI 0.47 to 1.37; heterogeneity not reported) compared with education through a self-care book without physical exercises. 41 Moreover, yoga showed a moderate overall effect on reducing low-back pain (4 RCT, number of participants not informed, SMD=−0.61; 95% CI −0.97 to −0. 26; I²=63%) compared with passive interventions (usual daily care, waiting list, educational or social environment). 43
Compared with no exercise, 37 the results favoured yoga as way of reducing low-back pain in the follow-up of 4–6 weeks (2 RCT, 40 participants, MD=−10.83; 95% CI −20.85 to −0.81; I 2 =0%), 3–4 months (5 RCT, 458 participants, MD=−4.55; 95% CI −7.04 to −2.06; I 2 =0%), and at 6 months (4 RCT, 414 participants, MD=−7.81; 95% CI −13.37 to −2.25; I 2 =64%). At 12 months, the differences were not statistically significant. These results were moderate confidence at 6 months, but low to very low confidence in other follow-up points.
Furthermore, results favoured yoga compared with the practice of exercises after 1 week intensive practice (1 RCT, 80 participants, MD=−14.50; 95% CI −22.92 to −6.08; heterogeneity not applicable), 4 weeks (1 RCT, 54 participants, MD=−15.00; 95% CI −19.90 to −10.10; heterogeneity not applicable) and 7 months (1 RCT, 54 participants, MD=−20.40, 95% CI −25.48 to −15.32; heterogeneity not applicable). However, these results analyse single studies with small samples. 37 A second SR that compared yoga to physical exercise 38 found heterogeneous results not statistically significant.
A review without meta-analysis 12 reported that yoga effectively reduced chronic low-back pain. However, two studies included in the review pointed out that there was no evidence of pain improvement.
Low-back pain-related disability
Yoga practice compared with usual daily care, medical care or education 42 contributed to reduce specific disability associated with low-back pain in the short term, right after the intervention and 12 weeks after randomisation (8 RCT, 689 patients, SMD=−0.59; 95% CI −0.87 to −0.30; I 2 =59%) and long term a year after randomisation (5 RCT, 574 patients, SMD=−0.35; 95% CI −0.55 to −0.15; I 2 =20%). Also, yoga showed a moderate effect on improving functionality in patients with low-back pain compared with reading self-care books and exercises (8 RCT, number of participants not informed, SMD=−0.64; 95% CI −0.89 to −0.39; I 2 =62%). 43
In the same way, results favoured yoga when it was compared with no exercise. 37 Improvement was observed in the follow-ups of 4–6 weeks (5 RCT, 256 participants, SMD=−0.45; 95% CI −0.71 to −0.19; I 2 =0%), 3–4 months (7 RCT, 667 participants, SMD=−0.40; 95% CI −0.66 to −0.14; I 2 =54%), 6 months (6 RCT, 630 participants, SMD=−0.44; 95% CI −0.66 to −0.22; I 2 =34%) and 12 months (2 RCT, 365 participants, SMD=−0.26; 95% CI −0.46 to −0.05; I 2 =0%). The evidence, however, was considered of moderate confidence at 6 months and of low confidence for the other periods. When yoga was compared with exercise no differences were observed in specific back functionality. 37
Low-back pain clinical improvement
Concerning clinical improvement, yoga did better compared with no exercise after 4–6 weeks (2 RCT, 141 participants, RR=2.62; 95% CI 1.22 to 5.67; I 2 =0%), at 3 months (3 RCT, 168 participants, RR=3.18; 95% CI 1.86 to 5.44; I 2 =0%), and at 6 months (1 RCT, 128 participants, RR=2.53; 95% CI 1.36 to 4.71; heterogeneity measure not applicable). 37 However, such evidence was considered of low confidence. Otherwise, yoga compared with exercise showed no statistically significant difference in clinical improvement. 37
Cervical pain
A meta-analysis 36 showed better short-term (not specified) effects of yoga on the intensity of neck pain compared with usual care (3 RCT, 182 participants, SMD=−1.28; 95% CI −1.81 to −0.75; I 2 =62 %). Yoga also showed better results than exercises (8 RCT and 1 q-RCT, 488 participants, SMD=−1.26; 95% CI −1.83 to −0.68; I 2 =87%). However, authors found no statistically significant differences comparing yoga to pilates or complementary and complementary medicine. 39
Cervical pain-related disability
Compared with usual care, yoga showed better short-term (not specified) effects on cervical pain-related disability (3 RCT, 182 participants, SMD=−0.97; 95% CI −1.44 to −0.50; I 2 =55%). 36 In comparison to exercise, 39 yoga was superior in reducing disability (6 RCT and 1 q-RCT, 363 participants, SMD=−0.97, 95% CI −1.55 to −0.38; I 2 =82%), but there was no significant difference when compared with pilates or complementary and complementary medicine.
Pain associated with fibromyalgia syndrome
Practicing yoga reduced the pain associated with fibromyalgia syndrome in the short term (not specified) compared with late or usual treatment (2 RCT, 88 patients, SMD=−0.54; 95% CI −0.96 to −0.11; I 2 =0). 35
Pain associated with osteoarthritis and rheumatoid arthritis, and carpal tunnel and irritable bowel syndromes
Yoga significantly improved hand pain associated with osteoarthritis (after 8 weeks) and rheumatoid arthritis (after 40 days) compared with passive interventions. 43 One SR included one study that showed improvement in pain and physical function assessments in osteoarthritis. Also, a second study found improvement in joint sensitivity and hand pain during yoga. 40
An SR considered yoga and standard care (eg, wearing a wrist splint) equally beneficial to carpal tunnel syndrome pain based in one primary study. 12 Another study in the same review reported that yoga was not an effective treatment option for irritable bowel syndrome pain. 12
Quality of life and mood
Compared with usual care, yoga improved quality of life (2 RCT, 128 participants, SMD=0.57; 95% CI 0.17 to 0.97; I 2 =20%) and mood (2 RCT, 128 participants, SMD=−1.02; 95% CI −1.38 to −0.65; I 2 =0%) in patients with cervical pain. 36
Yoga compared with delayed treatment control in patients with fibromyalgia improved the quality of life (1 RCT, 53 participants, SMD=−0.71, 95% CI −1.27 to −0.15, heterogeneity measure not applicable) and depression (1 RCT, 53 participants, SMD=−0.84, 95% CI −1.41 to −0.28, heterogeneity measure not applicable) at the end of the treatment. 35
Yoga compared with non‐exercise controls improved the physical quality of life after 6 months (1 RCT, 259 participants, SMD=0.26, 95% CI 0.01 to 0.50, heterogeneity measure not applicable), and depression decrease 4–6 weeks after the intervention (1 RCT, 16 participants, SMD = −1.23, 95% CI −2.39 to −0.06, heterogeneity measure not applicable). The intervention also decreased depression in participants with chronic low-back pain after 6 months (1 RCT, 90 participants, SMD=−0.47, 95% CI −0.89 to −0.05, heterogeneity measure not applicable) and 12 months (1 RCT, 90 participants, SMD=−0.50, 95% CI −0.92 to −0.08, heterogeneity measure not applicable). 37
Yoga compared with exercises improved quality of life (3 RCT, 434 participants, MD=3.46, 95% CI 95% 0.75 to 6.16, I 2 =61%) and mood (4 RCT, 351 participants, SMD=0.61, 95% CI 0.95 to 0.27, I²=58%) in patients with chronic cervical pain. 39 Yoga compared with exercise controls showed an effect in the physical quality of life of chronic low-back pain patients after 4 weeks (1 RCT, 54 participants, SMD=1.68, 95% CI 1.06 to 2.31, heterogeneity measure not applicable) and after 7 months (1 RCT, 54 participants, SMD 1.34, 95% CI 0.75 to 1.94, heterogeneity measure not applicable). Yoga compared with exercise controls improved the mental quality of life after 4 weeks (1 RCT, 54 participants, SMD=0.79, 95% CI 0.24 to 1.35, heterogeneity measure not applicable) and after 7 months (1 RCT, 54 participants, SMD=1.33, 95% CI 0.74 to 1.92, heterogeneity measure not applicable). 37
Safety of yoga
Seven SRs reported information about adverse events associated with yoga. Three showed that yoga was not associated with serious adverse events. 35 36 42 Nevertheless, yoga was associated with increased low-back pain in some patients and an unspecified severe adverse event, 43 increased pain and herniated disc, 12 and a case of cellulitis. 38 Moreover, one SR found no differences between reports of adverse events comparing yoga to other exercises. 37
Overall, SRs favoured yoga compared with usual care, particularly in low back 42 43 and cervical 36 pain. Alternatively, there is little evidence about the superiority of yoga compared with active interventions. 37–39 Furthermore, the effectiveness of yoga was unclear for other conditions identified, such as pain associated with fibromyalgia, 35 osteoarthritis, 40 43 rheumatoid arthritis, 40 carpal tunnel and irritable bowel syndromes. 12 Considering the seven SRs that provided information about safety, 12 35–38 42 43 three reported no adverse events and another three found no severe adverse events (cellulitis, 38 herniated disc 12 and unspecified severe adverse event) 43 related to the intervention. Hence, the results of this rapid review suggest yoga can benefit health without harm.
In Brazil, the MoH has regulated integrative and complementary practices in the Unified Health System to promote health and quality of life through less invasive techniques.
A Brazilian study highlighted the positive effects of integrative and complementary practices such as yoga in primary healthcare. It indicated that such interventions are easy to implement, mainly because they grant autonomy and allow patients to cope with illness. However, it should be noted that the lack of infrastructure and poor communication with other health services may damage its effectiveness. 44
Comparison with other evidence
Similarly to what this rapid review found, the overview by Fishbein and Saper 11 points out that yoga is not related to high rates of serious adverse events. However, yoga should be performed according to each individual’s health condition. The study also indicates that the small sample size and lack of appropriate methods conducting primary studies diminish the quality of the evidence about the benefits of yoga.
Furthermore, a second overview targeting adults with acute and chronic health problems showed the benefits of yoga to pain control. The findings also stress the lack of robustness of the studies, which compromises the evidence. 45
Strengths and limitations
This rapid review was carried out in 45 days, simplifying steps from a traditional SR. Nonetheless, the shortcuts employed have followed a validated methodological guideline and the risks of them leading to inaccurate findings were considered.
The lack of information about the quality of primary studies included in the SRs decreased confidence in their results. It is noteworthy that even SRs themselves lack methodological rigour, since most of them were rated low or critically low overall confidence. The results are also based on primary studies with small samples, significant heterogeneity regarding the design of interventions, and considerable risk of bias. Hence, it is difficult to evaluate the effectiveness of yoga, and many uncertainties remain concerning its benefit.
Yoga can be an effective and safe practice to control chronic and acute pain, primarily in patients with low back or chronic cervical pain. Otherwise, the results were not very consistent for people with pain associated with osteoarthritis, rheumatoid arthritis, fibromyalgia, carpal tunnel and irritable bowel syndromes. Overviews of SRs highlighted the benefit of yoga for controlling acute and chronic pain, which corroborates the findings of this review. Therefore, more research is needed to increase the quality and strength of these results.
Ethics statements
Patient consent for publication.
Not applicable.
Ethics approval
This study does not involve human participants.
Acknowledgments
To the team of the National Coordination of Integrative and Complementary Practices of the Ministry of Health (CNPICS/DESF/SAPS/MS), for presenting the original demand for the production of this rapid review.
- Henschke N ,
- Kamper SJ ,
- International Association for Study of Pain (IASP)
- Ministério da Saúde (Brasil)
- Cohen M , et al
- Research and Markets
- Brettschneider C , et al
- Vasconcelos FH ,
- Souza DFdaSde ,
- Siqueira FV
- Toscano JJO ,
- Zefferino ACG ,
- Fishbein DB ,
- Crawford C ,
- Schoomaker E , et al
- Steel A , et al
- Ministério da Saúde
- Tricco AC ,
- Langlois EV
- McKenzie JE ,
- Ouzzani M ,
- Hammady H ,
- Fedorowicz Z , et al
- Reeves BC ,
- Wells G , et al
- Gaylord S ,
- Buben A , et al
- Kinser PA ,
- Jallo N , et al
- Friedly J , et al
- Coeytaux RR ,
- McDuffie J , et al
- Kelley GA ,
- Antunes PDC ,
- Lagranha DM ,
- Sousa MFde , et al
- Budhrani-Shani P ,
- Arcari P , et al
- Faurot KR ,
- Gaylord SA , et al
- Borges MG , et al
- Langhorst J ,
- Dobos GJ , et al
- Brinkhaus B , et al
- Wieland LS ,
- Pilkington K , et al
- Skelly AC ,
- Jiang J , et al
- Morone NE ,
- Haller H , et al
- Stebbings S ,
- Cherkin D , et al
- Galvanese ATC ,
- Barros NFde ,
- d’Oliveira AFPL
- McCall MC ,
- Roberts NW , et al
Supplementary materials
Supplementary data.
This web only file has been produced by the BMJ Publishing Group from an electronic file supplied by the author(s) and has not been edited for content.
- Data supplement 1
- Data supplement 2
- Data supplement 3
Twitter @czrlqn
Contributors AÂVR and RCdM contributed to eligibility and extraction processes, article text development, research reports construction and final manuscript elaboration. CDLJ and MCdB contributed to manuscript revision. JOMB and TST coordinated the study. All authors contributed, revised and approved the final article. JOMB is the guarantor of the study.
Funding The Brazilian Ministry of Health commissioned this rapid review as part of the PRES008-FIO-18 project, developed by the Oswaldo Cruz Foundation (Fiocruz). This publication was also supported by a project funded by the Ministry of Health of Brazil (TED MS/SCTIE-Fiocruz # 43/2016).
Competing interests This rapid review was commissioned and subsidized by the Ministry of Health, but the authors declare that the funding body did not interfere in the conduct of the review or the presentation of its results.
Provenance and peer review Not commissioned; externally peer reviewed.
Supplemental material This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Read the full text or download the PDF:
- Posts (RSS)
- Comments (RSS)
- Mission Statement
- Board and Contact
- Weight, Glucose, Hypertension, Cholesterol
- Yoga as a self-care strategy
- Mindfulness-based stress reduction and health benefits.
- Meditation as psychotherapy
- Yoga for anxiety
- Yoga for depression
- Hatha Yoga for Depression
- Does Mindfulness Meditation Improve Anxiety and Mood Symptoms?
- An introduction to kundalini yoga meditation techniques that are specific for the treatment of psychiatric disorders.
- Yoga in cardiac health
- Psychophysiologic effects of hatha yoga on musculoskeletal and cardiopulmonary function
- The influence of yoga-based programs on risk profiles in adults with type 2 diabetes mellitus
- Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga
- Meditation practices for health
- Yoga for menopausal symptoms
- Hatha yoga therapy management of urologic disorders
- An evidence-based review of yoga as a complementary intervention for patients with cancer
- Hemodynamic observations on a yogic breathing technique claimed to help eliminate and prevent heart attacks
- Therapeutic effects of yoga for children
- Clinical trials of meditation practices in health care
- Yoga in stroke rehabilitation
- Yoga as a therapeutic intervention
- Using yoga to treat disease
- Benchmarks used in researching yoga’s effect
Literature Review of Research on Yoga Benefits
- Yoga for Arthritis
- Yoga as Adjunctive Therapy for Migraines
- Hatha Yoga to treat Stress, Anxiety and Attentional Suppression
- Pranayama and Yoga Nidra for Cancer Treatment and Treatment-Related Anxiety and Depression
- The Benefits of Yoga and Meditation for Cellular Health and Aging
- Queer and Trans Yoga: Practices of Utopia in Hostile Times
- Yoga for Postnatal Mental Health
- Kundalini Yoga – cognitive benefits for older women at risk of Alzheimer’s disease
- Easing Fatigue and Anxiety Related to Multiple Sclerosis
- Iyengar Yoga and Rheumatoid Arthritis
- Laughter Yoga in Cancer Patients
- Yoga as an Exercise Prescription for the Pregnancy or Postpartum Period
- Yoga Impact on Insomnia and Systolic Blood Pressure
- Effects of Yoga in People with Type 2 Diabetes
- Creativity and Yoga Nidra
- Effects of yoga and meditation in children with ADHD
- Yoga for Trauma Survivors
- Short In-Class Survey to Measure Success!
- Teacher and Student Mid-Term and End-Term Surveys
- Want a Yoga Program at Your Organization?
- How Studios Can Help
- Become a Member
- Join Our Board
- Sponsor a Class
- Teaching Yoga in Service Settings
- What to Teach, Where, and How: Yoga Class Preferences of a Non-Studio-Based Outreach Yoga Community
- Motivations for Service
- 10 Commandments of Yoga Outreach
- Program Set Up Guide
- Site Visits
- Breathing Guide
- Responding to Abreactions
- Program Set Up Questionnaire
- Training Directory
- Yoga Activist Trainings
- Evaluate Trainings
- Request Scholarships
- What is a Yoga Outreach Teacher?
- What is a Yoga Outreach Understudy?
- Your First Yoga Class
- Student Practice Guides
- Grants & Features
- Fundraising
- Yoga Outreach Organization Directory
- Donate Mats
- Requesting Mats
- Program Reach
- Internships
- Donate Now!
At the request of Jasmine Chehrazi, Founder of YogaActivist.org , a group of nine graduate students enrolled in the Master of Public Health (M.P.H.) program at The George Washington University conducted a literature review on the health benefits of yoga. The review provides YogaActivist.org with information needed to further develop its network of studio-supported yoga outreach programs to diverse communities, both locally and nationally. Specifically, the review highlights the dynamic interplay between stress, weight, and other disease indicators—all of which can be addressed, if not mitigated, through routine participation in yoga.
The group of M.P.H. students searched for relevant articles in academic, peer-reviewed journals, including, but not limited to, the Journal of General Internal Medicine, Journal of Psychiatric Practice, Alternative Therapies in Health and Medicine, International Journal of Nursing Studies, Journal of Affective Disorders, Rehabilitation Oncology, and Topics in Clinical Nutrition. The search was by no means exhaustive, but the group found and summarized 19 different articles demonstrating the effectiveness of yoga in promoting physiological and mental health, as well as in controlling disease and disease indicators. While the 19 studies differ in study type, design, purpose, sample size, target population, yoga method(s) and technique(s), length of follow-up, and overall findings, they together demonstrate the widespread applicability of yoga to diverse populations, irrespective of gender, age, race/ethnicity, weight, or health status.
Through the literature review, the nine students found documentation of yoga’s effectiveness in treating musculoskeletal conditions, improving mental health, reducing stress and anxiety, increasing cortisol levels (associated with self-esteem and tenacity and lower levels of nervousness and depression), improving pulmonary function among asthmatic children, increasing exercise self-efficacy, reducing and/or controlling blood pressure, slowing weight gain, controlling diabetes mellitus, and improving overall mood. Such benefits extend to individuals across the life span. While yoga alone is insufficient to reverse disease or substantially improve health status, the literature suggests that yoga, when combined with other intervention measures, can reap significant physiological and mental health benefits for diverse populations. Yoga is a personal, non-competitive physical activity. When practiced correctly and routinely, yoga provides individuals of all ages with the motivation and self-efficacy needed to live and maintain healthier lifestyles.
Below is a summary of each of the 19 articles regarding the effectiveness of yoga interventions in promoting health. The summaries are categorized by the primary health or behavioral objective of each study.
Yoga and Mental Health
1) Lee SW, Mancuso CA, Charlson ME. Prospective study of new participants in a community-based mind-body training program. J Gen Intern Med. 2004;19(7):760-5.
FINDING: A 3-month yoga program improved mental health scores and other quality of life measures. Yoga Type: Dahn-hak. 1) stretching exercises for large muscle groups and shoulders, neck,hips, back, and knees, 2) postures are held for “energy accumulation 3) 5- to 10-minute meditation intended to facilitate “energy awareness”, 4) repetition of the large muscle group stretches. Yoga Frequency/Duration : 1-hour class offered 2-to-3 times per week for 3 months.
OBJECTIVE: To measure changes in health-related quality of life associated with 3 months of mind-body training as practiced in community-based settings.
METHODS: A prospective cohort study was done in eight centers for the practice of mind-body training in the metropolitan New York City area with 194 adults, and 171 completed the follow-up survey. Participants typically attended a 1-hour class two to three times per week. They were given a questionnaire before the classes began and 3 months later with questions about mental and physical health from validated survey instruments.
RESULTS: At baseline, new participants reported lower scores than U.S. norms for 7 of 8 domains of the Medical Outcomes Study SF-36 general health questionnaire. After 3 months of training, within patient change scores improved in all domains (P< .0001), including a change of +15.5 in the mental health domain. In hierarchical regression analysis, younger age, baseline level of depressive symptoms and a history of hypertension were independent predictors of greater improvement in the SF-36 mental health score. Five participants (2.9%) reported a musculoskeletal injury.
2) Uebelacker LA, Epstein-Lubow G, Gaudiano, BA. Hatha. Yoga for depression: critical review of the evidence for efficacy, plausible mechanisms of action, and directions for future research. J Psychiatr Pract. 2010;16:22–33.
FINDING: A review of eight clinical trials showed the yoga may help treat depression. Note: Methodological concerns with most trials. Yoga Type : Some asana-focused, some meditation-focused Yoga Frequency/Duration : Varied in length from 3 days to 12 weeks and in intensity from daily to once per week.
OBJECTIVE: Review the literature of studies evaluating the efficacy of yoga for the treatment of depression and possible mechanisms .
METHODS: Studies were included in the review if they were clinical trials with one of the intervention arms involving a predominantly yoga intervention and a requirement for participants to have a diagnosed depressive disorder or elevated depression symptoms.
RESULTS: Eight trials were found. The number of participants ranged from 28 to 89. Of the five studies that compared yoga to no/minimal treatment, four found some evidence that yoga was superior to the control group, and the final one did not directly compare the two groups. Studies varied in length of intervention from 3 days to 12 weeks and in intensity from daily to once per week, and different types of yoga were used (some asana-focused and some meditation-focused). Effect sizes of differences varied widely, and methodological differences and flaws threatening internal validity make it difficult to draw generalizable conclusions.
3) Birdee GS, Legedza, AT, Saper RB. Characteristics of yoga users: results of a national survey. J Gen Intern Med . 2008;23(10):1653-1658.
FINDING: A national survey of yoga users showed it to be helpful for overall health and well being, mental health, and musculoskeletal conditions. Yoga Type: N/A Yoga Frequency/Duration : Self-report that person had practiced yoga during past 12 months (and not tai chi or qi gong)
OBJECTIVE: To characterize yoga users, medical reasons for use, perceptions of helpfulness, and disclosure of use to medical professionals.
METHODS: A cross-sectional study was done using data from the National Health Interview Survey Alternative Medicine Supplement with 31,044 respondents. Survey participants were asked if they had practiced yoga during the past 12 months. If they had practiced yoga, but not tai chi or qi gong, they were asked whether they practiced yoga for medical conditions and if it helped their condition and also how important yoga was in maintaining their general health and well-being.
RESULTS: The prevalence of yoga use for health in the U.S. was 5.1percentwith a mean age of 39.5. Most yoga users (58%) felt that yoga was an important part of maintaining their health and well-being. A smaller percentage of yoga users reported using yoga to treat specific medical conditions (16%). Among medical conditions, 10.5percentand 3.3percentof yoga users reported using yoga to specifically treat musculoskeletal and mental health conditions, respectively. A majority of these yoga users reported yoga as helpful for their mental health (83%) and musculoskeletal condition (76%).
4) Woolery A, Myers H, Sternlieb B, Zeltzer L. A yoga intervention for young adults with elevated symptoms of depression. Alter Ther Health Med . 2004;10(2):60-63.
FINDING: A 5-week program of yoga showed reductions in depression and anxiety among young adults. Yoga Type : Iyengar Yoga Frequency/Duration : Two 1-hour classes per week for 5 weeks
OBJECTIVE: To determine the short-term effect of yoga on mood in mildly depressed young adults.
METHODS: Twenty-eight 18-29 year olds with mild depression were randomly assigned to an intervention group or a wait-list control group. The intervention group participated in a 5-week yoga program of two 1-hour classes per week. Measurements of depression and anxiety levels were made using the Beck Depression Inventory (BDI), State Trait Anxiety Inventory (STAI), and Profile of Mood States (POMS) survey instruments before classes began, midway through the program and at the program’s completion. Morning cortisol levels were also taken at the same time points.
RESULTS: The yoga group showed a significantly greater reduction in depression compared to the control group (p<.001). A similar pattern was seen for trait anxiety (p<.001) Significant pre- to post-class reductions were seen in depression-dejection, tension-anxiety, anger-hostility, fatigue-inertia, confusion-bewilderment, and total mood disturbance. Yoga participants also showed higher morning cortisol levels, which are associated with self-esteem, hardiness, and tenacity, and lower levels of nervousness and depression.
5) Chen KM, Chen MH, Chao HC, Hung HM Lin, HS, et al. Sleep quality, depression state, and health status of older adults after silver yoga exercises: cluster randomized trial. Inter J Nurs Stud. 2008;4:154-163.
FINDING: A 6-month yoga program improved sleep quality, depression, and perceived health status among older adults who reside in the community. Yoga Type : Warm up, hatha yoga gentle stretching, relaxation, and guided-imagery meditation. Yoga Frequency/Duration : 70 minutes three times per week for six months.
OBJECTIVE: To test the effects of six months of silver yoga exercises in promoting the mental health of older adults in senior activity centers, especially among the indicators of sleep quality, depression, and self-perception of health status.
METHODS: A cluster randomized trial was conducted in eight senior citizen activity centers in southern Taiwan. Participants were randomly assigned into either the experimental (n = 62) or the control (n = 66) group based on their attendance at selected senior activity centers. A 70-minute silver yoga exercise program was implemented three times per week for six months as the intervention for the participants in the experimental group.
RESULTS: The mental health indicators of the participants in the experimental group were significantly improved in comparison to the participants in the control group after the silver yoga interventions (all p < .05). Many of the indicators improved after three months of the intervention and were maintained throughout the six month study. These indicators included subjective sleep quality (as measured by the Pittsburgh Sleep Quality Index (PSQI) score), daytime dysfunction, physical and mental health perception, and depression state.Silver yoga exercise sessions were taught 3 times per week, for 70 minutes each session, over 6 months. Each 70-minute session included a warm up, hatha yoga gentle stretching, relaxation, and guided-imagery meditation. No additional details regarding postures or sequence are provided. For consistency over the course of the intervention, yoga instructors followed a pre-recorded tape made by the principal investigator which verbally guided them through the sequence of postures for each session.
6 ) Gupta N, Khera S, Vempati RP, Sharma R, Bijlani RL. Effect of yoga based lifestyle intervention on state and trait anxiety. Indian J Physiol Pharmacol. 2006;50(1): 41-47.
FINDING: Short educational program for stress management and lifestyle modification based on yoga leads to reduction in anxiety. Yoga Type : Asanas and pranayama Yoga Frequency/Duration : 8-day outpatient course, 3-4 hours/day, over 10 days (with a 2-day weekend break)
OBJECTIVES: To study the short-term impact of a comprehensive, yet brief, lifestyle intervention based on yoga in diseased and normal individuals.
METHODS: The research subjects had a history of hypertension, coronary artery disease, diabetes mellitus, obesity, psychiatric disorders and thyroid disorders. The intervention consisted of asanas, pranayanama, relaxation techniques, group support, individualized advice, lectures and films on philosophy of yoga, and the place of yoga meditation in daily life, meditation, and stress management.
RESULTS: Outcome measures were anxiety scores taken on the first and last days of the course. Among diseased individuals, improvement was seen in anxiety levels.
7) Galantino ML, Cannon N, Hoelker T, Iannaco J, Quinn L. Potential benefits of walking and yoga on perceived levels of cognitive decline and persistent fatigue in women with breast cancer. Rehab Oncol. 2007;25(3):3-12.
FINDING: Exercise, specifically walking and yoga, have been proven effective in enhancing quality of life and decreasing fatigue in breast cancer populations. Yoga Type : variable Yoga Frequency/Duration : variable
OBJECTIVE: To investigate available evidence for the effect of walking and yoga on breast cancer survival following chemotherapy.
METHODS: Authors searched randomized clinical controlled trials, systematic reviews, cohort studies, and case series for information regarding the effect of walking and yoga on quality of life, persistent fatigue, and perceived levels of cognitive decline in breast cancer populations.
RESULTS: Yoga proved to be beneficial in breast cancer populations, leading to improvements in sleep quality, strength, flexibility, and quality of life. The three main components of yoga—asanas (yoga physical postures), pranayama (breathing exercises/patterns), and dhyana (meditation)—have been shown to decrease fatigue and improve perceptions of vitality.
8 ) Janakiramaiah N, Gangadhar BN, Naga Venkatesha Murthy PJ, Harish MG, Subbakrishna DK, et al. Antidepressant efficacy of Sudarshan Kriya yoga (SKY) in melancholia: a randomized comparison with electroconvulsive therapy (ECT) and imipramine. J Affect Disord. 2000;57(1-3):255-259.
FINDING: Once daily practice of Sudarshan Kriya yoga (SKY) was found to be equally effective to medication and nearly as effective as electro-shock therapy in the remission of depression among patients. Yoga Type : Sudarshan Kriya yoga was used with some changes. To make it widely acceptable to patients and the medical profession, some of the adventitious components (e.g., briefing about positive attitudes to life ‘living in the present’, etc.) were dropped as were the meditative aspects. The physiological technique consisting of only specified rhythms of breathing. This adaptation for clinical purposes was designated Sudarshan Kriya Yoga. There were three sequential components interspersed with normal breating while sitting with eyes closed. The procedure closed with 10-15 minutes of Yoga Nidra (tranquil state) in supine position. Yoga Frequency/Duration : Six 45-minute sessions during mornings per week. For patients with marked diurnal retardation, afternoon sessions were also recommended. Mean number of sessions was 20.
OBJECTIVE: To investigate the efficacy of yoga practice as it compares to traditional treatments of clinical depression.
METHODS: Randomized, control study of 45 patients hospitalized with severe depression (as defined by the Beck Depression Inventory and Hamilton Rating Scale for Depression). The patients were divided into three groups with the first receiving electroconvulsive therapy three times weekly for four weeks. The second group was administered imiprimine, an antidepressant medication, at typical dosing. The last group was trained in SKY and encourages to practice it daily. Pre/Post test surveys focused on depressive effects.
RESULTS: Patients practicing SKY were noted to have a 67percentremission rate of their symptoms showed it to be as effective as imiprimine and nearly as effective as electroconvulsive therapy. Though compelling, the findings are subject to possible selection bias due to inadequate group sizes for statistical validity. However, they are highly suggestive that further investigation into the clinical efficacy of yoga practice is warranted and could present itself as a low-risk/high-reward alternative to traditional depression treatments.
9) Vedamurthachar A, Janakiramaiah N, Hegde JM, Shetty TK, Subbakrishna DK, et al. Antidepressant efficacy and hormonal effects of Sudarshan Kriya Yoga (SKY) in alcohol dependent individuals. J Affect Disord. 2006;94:249-253.
FINDING: Practice of yoga was found to demonstrate antidepressant effects in a randomized control trial among consenting patients participating in alcohol detoxification programs. Measures of cortisol, ACTH and prolactin revealed a possible biological mechanism for yoga’s effects. Yoga Type : The SKY consisted of three distinctive breathing periods (Pranayama):1. Ujjayi pranayama: Consists of slowdeep breathing. Each cycle includes breathing in, holding, breathing out and holding.2. Bhastrika pranayama consists of forced inhalation and exhalation 20 times. Ujjayi and Bhastrika pranayama requires about 12–15 min.3. Cyclical breathing consists of slow, medium, and fast cycles of breathing practiced for a total duration of 30min.These three procedures are done in sitting posture (Sukhasana) with eyes closed. This was followed by Yoga Nidra (lying in a tranquil state) for about 20 min. Yoga Frequency/Duration : One 65-minute session once per day for two weeks.
OBJECTIVE: To determine the effectiveness of yoga practice in the treatment of depression among individuals participating in alcohol dependence detoxification.
METHODS: After a week of detoxification management, subjects were recruited to participate in a randomized-control study. There were a total of 60 subjects who participated in a two-week study. The control group was provided standard detoxification, while the intervention group practiced daily sessions of breathing exercises and yoga practice. Effects were measured with the use of the Beck Depression Inventory (BDI) pre/post each session and morning plasma cortisol, ACTH and prolactin measures were taken prior to and following the two-week intervention.
RESULTS: Both the control and intervention groups displayed a reduction in self-reported depression symptoms according to the BDI. Additionally, there was a noted correlation between depression symptom reduction and reduction of morning plasma cortisol levels among the intervention group participants. Physical measures of cortisol suggest a biological pathway for the observed results among program participants. The small group size is a possible confounder of these results. Also, it was noted by those administering the study that depression symptoms declined in all patients over that same period. However, the level of reduction and the effects on cortisol measures suggest a biological pathway of depression reduction in those practicing yoga.
Yoga and Stress in Children
10) Mendelson T, Greenberg, MT, Dariotis, JK, Gould, LF, Rhoades, BL, et al. Feasibility and preliminary outcomes of a school-based mindfulness intervention for urban youth. J Abnorm Child Psychol. May 4, 2010; DOI:10.1007/s10802-010-9418-x.
FINDING: A 12-week intensive yoga program improved involuntary stress responses in 4 th and 5 th graders. Yoga Type : Yoga-inspired postures and movement series, including bending, stretching, and fluid movement. Poses were selected to enhance muscle tone and flexibility, and students were taught the health benefits of the poses. Students also practiced breathing, starting with beginner exercises and gradually moving to more advanced ones. These exercises trained the youths to use their breath to center and calm themselves. At the end of each class, youth lay on their backs with their eyes closed while the instructors guided them through a mindfulness practice, which involved attending to a specific focus for several minutes, such as paying attention to each breath or sending out positive energy to others. The brief period of discussion prior to the guided mindfulness practice in which instructors offered didactic information about topics such as identifying stressors, using mindfulness techniques to respond to stress, cultivating positive relationships with others, and keeping one’s mind and body healthy. This information was oftenwoven into the subsequent guided mindfulness practice (e.g., using the breath to create calm if something stressful has happened). Yoga Frequency/Duration : Four 45-minute session per week for 12 weeks.
OBJECTIVE: To assess the feasibility, acceptability, and preliminary outcomes of a school-based mindfulness and yoga intervention.
METHODS: Ninety-seven 4 th and 5 th graders in the inner city of Baltimore participated in a 4-day per week 12-week yoga and mindfulness program at school. Each yoga session lasted 45 minutes and occurred during a non-academic time period. Students were given a questionnaire to assess their stress response, depressive symptoms, and relations with peers and school, all of which used validated instruments.
RESULTS: Many students were eager to join the program, and a focus group showed that participants had a positive experience with the program. The intervention group’s survey responses showed significant improvements in involuntary stress responses as compared to controls (p<.001). Significant different were also seen on three subscales, including rumination, intrusive thoughts, and emotional arousal (p<.01).
11) Stueck M, Gloeckner N. Yoga for children in the mirror of science: working spectrum and practice fields of the training of relaxation with elements of yoga for children. Early Child Dev Care. 2005;175:371-377.
FINDING: In a small study, a 15-week program of yoga and relaxation training improved stress responses in preteens. Yoga Type : 1) Relaxation. Used technique called ‘journey through the body’, which consists of different concentration tasks on single body parts. Other used first relaxation techniques are breathing techniques from yoga (ujjayi, nadhi shodana, alternating breathing). 2) Yoga exercises. a) 23 different yoga exercises (based on Shivananda-Yoga, Rishikesh/India) b) individual complex of yoga exercises c) participants can develop their own complex yoga and instruct others. 3) Series of activities such as massage techniques (partner massage, ball massage), meditation (candle meditation), sensory exercises (discovering of objects by touching and smelling), and interactive exercises (‘trust game’, ‘jumping lotus flower’) as well as six different imagery techniques. Yoga Frequency/Duration : One 1-hour session per week for 15 weeks.
OBJECTIVE: To determine whether yoga can assist in reducing stress responses in preteens.
METHODS: Forty-eight 11-12-year olds with abnormal exam anxiety participated in the study with 21 students assigned to the experimental group to participate in a 15-session program of relaxation, yoga, and other meditation and social interaction exercises. Each session lasted one hour. A questionnaire with stress-related items was given to students before the sessions began, immediately after the 15-week program, and three months after the program ended.
RESULTS: Students involved in the program showed improvement in several stress measures. Significant effects were seen in a comparison immediately after the training: decreased aggression, decreased helplessness in school, decreased physical complaints, improved stress coping abilities. In a comparison 3-months later, the following effects were seen: improvements in emotional balance, decreased anxiety, decreased shyness in social contacts, and decreased impulsiveness. In the first post-test measurement, parents also reported their students as being calmer and more balanced (71.4%), less impulsive, aggressive and hot-tempered (38.1%), more concentrated (38.1%), and having fewer complaints (38.1%). Comparisons to the control group were not statistically measured.
Yoga and Attention Problems in Children
12) P eck HL, Kehle TJ, Bray MA, Theodore LA. Yoga as an intervention for children with attention problems. School Psych Rev. 2005;34z:415-424.FINDING: A small study showed an improvement in “time on task” for elementary school students with attention problems. Yoga Type : “Yoga Fitness for Kids” DVD by Gaiam (2003). Deep breathing, postures, and relaxation exercises. Poses included frog, downward dog and bridge. Movement in a gamelike manner interspersed between poses. Ended with guided imagery while lying on their backs. Yoga Frequency/Duration : Two 30-minute sessions per week for 3 weeks.
OBJECTIVE: To investigate the effectiveness of yoga for improving time on task in children with attention problems.
METHODS: Ten students ages 6-10 with attention problems (but not diagnosed with Attention Deficit Hyperactivity Disorder (ADHD)) participated in a 30-minute yoga videotape program twice per week for 3 weeks. Measurements were made of children’s “time on task”, defined as the percentage of intervals observed where the students had eye contact with the teacher or assigned task and performed the requested classroom assignments in 10-minute observations. Measurements occurred twice per week as follows: baseline for 3-7 weeks (varying by grade level), intervention for 3 weeks, and follow-up for 3 weeks. Measurements occurred at the same time each day, and a child of the same gender (for each child in the program) in each classroom was chosen as a comparison.
RESULTS: An improvement in the mean “time on task” was seen both immediately following the intervention (effect size 1.5 to 2.7) and in the follow-up period (effect size 0.77 to 1.95). No change was seen in the comparison group.
Yoga and Asthma in Children
13) Jain SC, Rai L, Valecha A, Jha, UK, Bhatnagar SO , Ram K . Effect of yoga training on exercise tolerance in adolescents with childhood asthma. J Asthma . 1991;28(6):437-442.
FINDING: Yoga training improved pulmonary function and exercise capacity in children and teens with asthma. Yoga Type : Yogic cleansing procedures, postures, and breathing. Yoga Frequency/Duration : Daily for 90 minutes in morning and 1 hour in evening for 40 days.
OBJECTIVE: To determine if yoga can improve pulmonary function and exercise capacity in children with asthma.
METHODS: A study of 46 children with a mean age of 15.8 years and a history of asthma was performed. Children participated in 40 days of yoga training, and measurements were made of forced expiratory volume, distance walked in a 12-minute time period and overall physical fitness as assessed by a modified Harvard Step Test. Twenty-six patients were followed for up to two years and asthma symptoms and medication requirements were measured.
RESULTS: Improvements were seen in expiratory volume, distance walked in a 12-minute time period and overall physical fitness. Of patients followed for up to two years, children showed a continued reduction in asthma symptoms and less need for medication. Fourteen of the children with mild asthma who continued yoga every day for 15-30 minutes remained asymptomatic.NOTE: This article was not available through GWU. The data were obtained from the abstract and from a review article: Galantino ML, Galbavy R, Quinn L. Therapeutic effects of yoga for children: a systematic review of the literature. Pediatr Phys Ther . 2008;20(1):66-80.
Yoga and Obesity, Diabetes, and Cardiovascular Disease
14) Kristal AR, Littman AJ, Benitez D, White E. Yoga practice is associated with attenuated weight gain in healthy, middle-ages men and women. Altern Ther Health Med. 2005;11(4):28-33.
FINDING: Practicing yoga for four or more years slowed weight gain in middle-ages adults. Yoga Type : N/A Yoga Frequency/Duration : Self-report of number of days per week and minutes per day they practiced yoga and the number of years. Yoga practice was grouped into three categories of increasing intensity.
OBJECTIVE: To examine whether yoga practice is associated with a lower mean 10-year weight gain after age 45.
METHODS: 15,550 adults ages 53 to 57 were recruited into the Vitamin and Lifestyle cohort study between 2000 and 2002. A validated physical activity questionnaire was given to the participants, which asked about a variety of activities including yoga. Participants reported the number of years in the last 10 years that they did each activity and the number of days per week and minutes per day. Yoga practice was grouped into three categories of increasing intensity. Self-reported weight and height were used to calculate participants’ current BMI, and the weight change was calculated from the difference between their current weight and their weight at age 45 (also by self-report).
RESULTS: Individuals with a BMI less than 25 who practiced yoga for four or more years had a 3.1 lb. lower weight gain than those who had not practiced yoga. Individuals who were overweight and practiced yoga for four or more years showed an 18.5 lb. lower weight gain. All models were adjusted for other physical activity, dietary factors, and other obesity-related variables.
15) Sahay BK. Role of yoga in diabetes. J Assoc of Physicians India . 2007; 55 :121-126.
FINDING: Yoga has a role in diabetes control and prevention. Yoga Type : Pranayama Yoga Frequency/Duration : N/A
OBJECTIVE: To assess the role of yoga on glycemic control, insulin kinetics, body composition, exercise tolerance, and co-morbidities including hypertension and dyslipidemia.
METHODS: Individuals with diabetes and without diabetes were randomized to different groups and performed yogic practices for 45 minutes each day, which was followed by relaxation practices.
RESULTS: The studies confirmed that yoga has a useful role in the control of diabetes mellitus. Fasting and postprandial blood glucose levels decreased significantly. There were significant changes in insulin kinetics and those of counter-regulatory hormones such as cortisol. There was a decrease in fatty acids. There was an increase in lean body mass and a decrease in body fat percentage. The number of insulin receptors was increased, and there was an improvement in insulin sensitivity and a decline in insulin resistance.
16) Yang K, Bernardo LM, Sereika SM, Conroy MB, Balk J, et al. Utilization of a 3-month yoga program for adults at high risk for type 2 diabetes: a pilot study. Evid Based Complement Alternat Med . Published on-line: August 18, 2009 doi:10.1093/ecam/nep117. 1-7.
FINDING: Yoga may help to lower adult risk for type 2 diabetes, reduce cardio-metabolic risk factors, and increase exercise self-efficacy. Yoga Type : Vinyasa Yoga Frequency/Duration : 1-hour sessions, 2 times per week, for 3 months. Each session began with a 5-7 min warm-up and ended with a 10 min relaxation period.
OBJECTIVE: To conduct a pilot study to assess the feasibility of implementing a 12-week yoga program among adults at high risk for type 2 diabetes.
METHODS: Twenty-three adults were randomly assigned to either a yoga intervention group, which participated in a 3-month yoga intervention with 1-hour Vinyasa style yoga sessions twice per week, or an educational group, which received general health educational materials every 2 weeks. Participants had to: (1) be between 45 and 65 years of age; (2) be non-exercisers (no more than 30 minutes twice per week) for the previous year; (3) have a family history of type 2 diabetes, and; (4) have at least one cardio-metabolic risk factor. All participants completed questionnaires and had blood tests at baseline and at the end of the 3-month program to measure blood pressure, blood glucose, insulin, lipid levels, and body weight, as well as to assess exercise self-efficacy.
RESULTS: Compared with the education group, the yoga group experienced improvements in weight, blood pressure, insulin, triglycerides, and exercise self-efficacy. Findings suggest that a yoga program would possibly help to lower adults’ risk for type 2 diabetes, as well as reduce cardio-metabolic risk factors for adults at high risk for type 2 diabetes.
17) Guarracino JL, Savino S, Edelstein S. Yoga participation is beneficial to obesity prevention, hypertension control, and positive quality of life. Top Clin Nutr . 2006;21(2):108-113.
FINDING: Yoga may be beneficial in controlling weight, blood pressure, and mood. Yoga Type : Hatha and relaxation yoga. Yoga Frequency/Duration : The majority of study participants (55.7%) had practiced yoga for less than 1 year, followed next by those who had practiced yoga for more than 5 years (31.4%). The majority of participants (57.1%) practiced yoga for 1-2 hours per week, followed by those who spent less than 1 hour per week practicing yoga (24.3%).
OBJECTIVE: To evaluate the effects of hatha and relaxation yoga on obesity, blood pressure, and quality of life.
METHODS: Seventy healthy women and men ages 18 years or older were recruited from 3 fitness centers in Massachusetts after completing a 1-hour yoga class and were asked to complete a survey. The survey was used to measure how the participants felt after the yoga class, and questions included those related to yoga frequency and duration, other physical activity and duration, past and present medication use, food consumption behavior, demographic information, and data related to height, weight, blood pressure, tricep skinfold, and waist and mid-arm circumference.
RESULTS: According to survey results of the 70 participants, hatha and relaxation yoga had a statistically significant role in controlling weight, hypertension, and mood. Of the participants, those who had practiced yoga for less than 1 year had a significantly higher systolic blood pressure (mean 117.13) than those who had practiced yoga for 1-4 years (mean 107.56). However, the survey participants’ mean BMI (24.41) was significantly different from the BMI used as a cutoff for determining obesity (30.0), thus suggesting that individuals who practice hatha and relaxation yoga may not generally be obese.
18) Yang K. A review of yoga programs for four leading risk factors of chronic diseases. Evid Based Complement Alternat Med . 2007;4(4):487-491.
FINDING: Yoga programs may be effective in reducing body weight, blood pressure, blood glucose, and cholesterol. Yoga Type : Other than duration and frequency, most articles did not describe the yoga sessions in detail. Of the few articles that did identify the type of yoga studied, the most common was Hatha yoga. Yoga Frequency/Duration : The most common duration and frequency of yoga sessions in the studies were 30-60 min per session, with sessions meeting daily for 4-10 weeks. Many studies also used sessions meeting 2-3 times per week for 8-12 weeks.
OBJECTIVE: To review published studies of yoga programs and to determine the effect of yoga interventions on chronic disease risk factors, such as overweight, hypertension, high glucose level, and high cholesterol.
METHODS: A systemic search was conducted, yielding 32 articles from electronic databases published between 1980 and 2007. Of the 32 articles reviewed, 12 described experimental studies, 18 described quasi-experimental studies, and 2 described observational studies. Only 7 of the studies were conducted in the United States, and only 16 of the studies focused on subjects with diabetes, hypertension, or cardiovascular disease.
RESULTS: In analyzing the 32 articles, the authors found that yoga interventions are generally effective in reducing body weight, blood pressure, blood glucose level, and cholesterol level. However, only a few studies examined long-term effects.
Yoga and other Health Issues
19) Pullen PR, Thompson WR, Benardot D, Brandon LJ, Mehta PK, et al. The Benefits of yoga for African American heart failure patients. Med Sci Sports and Exerc. 2010:42(4): 651-657.
FINDING: Yoga improves cardiovascular endurance for African Americans who have suffered from heart failure. Yoga Type : Pranayama and Asanas. Yoga Frequency/Duration : 5 minute warm-up, including breathing exercises a 40 minute period of postures, ending with a 15 minute relaxation phase. Patients attended a total of 16 supervised sessions over an 8-10 week period.
OBJECTIVE: To see if yoga can improve physical and psychological parameters (cardiovascular endurance (VO2peak), flexibility, quality of life (QoL) and inflammatory markers) among patients with heart failure (HF), particularly among African Americans.
METHODS: Forty patients (38 AA, 1 Asian, 1 Caucasian) with systolic or diastolic HF were randomized to the yoga group (YG, N=21) or the control group (CG, N=19). All patients were asked to follow a home walking program. Pre- and post-measurements included a treadmill stress test to peak exertion, flexibility, interleukin-6 (IL-6), C- reactive protein (CRP), and extra cellular-super oxide dismutase (EC-SOD). QoL was assessed by the Minnesota Living with Heart Failure Questionnaire (MLwHFQ).
RESULTS: Yoga therapy offered additional benefits to the standard medical care of predominantly AA HF patients by improving cardiovascular endurance, QoL, inflammatory markers and flexibility.

Yeehaw: Riding the Yoga-Coaster
As Danny Dwyer will tell you, his life is a mixture of great success and major failures – a roller coaster ride where he sometimes “felt like throwing his hands in the air and screaming, ‘Yeehaw!’ and other times was so full of fear so all [he] could do was hold on as tight as […]

Teacher Feature: Katy Jones
Katy Jones is the founder of Root to Rise Inc. of Oklahoma. Inspired by an online video about prison yoga she saw over a year ago on Facebook, Katy knew serving others through yoga was her calling. After attending a Prison Yoga Project training in LA, she brought yoga to her local prison in Oklahoma. Seeing […]

[email protected] © 2022 Yoga Activist | Design donated by David Onate

IMAGES
COMMENTS
A systematic review by Larson-Meyer examined the metabolic energy expenditure during Hatha yoga, the most widely practiced style of yoga in the United States. The review found that, while some specific yoga poses can be metabolically exerting (with energy expenditures >3 METS), most yoga practices fall under the American College of Sport ...
Conclusions: Yoga has been studied under a wide variety of clinicopathological conditions in the year 2020. This landscape review intends to provide an idea of the role of yoga in various clinical ...
Yoga is one of the integrative therapies that has come to light as having a substantial role in preventing and mitigating such disorders. It thus seems trite to analyze and discuss the research advancements in yoga for 2020. The present review attempts to distill recent research highlights from voluminous literature generated in 2020.
Several literature reviews have been conducted that examined the impact of yoga on specific health conditions including cardiovascular disease metabolic syndrome, diabetes, cancer, and anxiety. Galantino et al. published a systematic review of the effects of yoga on children. These reviews have contributed to the large body of research evidence ...
Instructor-led yoga is identified in a majority of cases (17 reviews), independent or home study (13 reviews), book-led yoga (5 reviews), audio-led yoga (4 reviews), and video-led yoga in one review. No review evaluates the effect of yoga by type or delivery mechanism for a specific health condition.
We reviewed 11 studies examining the effects of yoga practice on the brain structures, function and cerebral blood flow. Collectively, the studies demonstrate a positive effect of yoga practice on the structure and/or function of the hippocampus, amygdala, prefrontal cortex, cingulate cortex and brain networks including the default mode network ...
To examine the empirical evidence regarding the mechanisms through which yoga reduces stress, we conducted a systematic review of the literature, including any yoga intervention that measured stress as a primary dependent variable and tested a mechanism of the relationship with mediation. Our electronic database search yielded 926 abstracts, of ...
Background Pain is a sensation of discomfort that affects a large part of the population. Yoga is indicated to treat various health conditions, including chronic and acute pain. Objective To evaluate the effectiveness and safety of yoga to treat acute or chronic pain in the adult and elderly population. Study selection A rapid review was carried out, following a protocol established a priori ...
The data were obtained from the abstract and from a review article: Galantino ML, Galbavy R, Quinn L. Therapeutic effects of yoga for children: a systematic review of the literature. Pediatr Phys Ther. 2008;20(1):66-80. Yoga and Obesity, Diabetes, and Cardiovascular Disease
A number of systematic reviews of yoga interventions in a broad range of healthy and chronically ill populations, reported that yoga practice results in decreased stress, anxiety, and depression. 14, 15, 17, 58 Similarly, a 2016 bibliographic review concluded that yoga has beneficial effects on a variety of psychiatric and medical conditions.