

Methadone Clinic Business Plan [Sample Template]
By: Author Tony Martins Ajaero
Home » Business ideas » Healthcare and Medical » Drug & Alcohol Rehab

Do you want to start a methadone clinic and need to write a plan? If YES, here is a sample methadone clinic business plan template & FREE feasibility report.
If you are drawn towards helping people with one for or addiction or the other overcome their addiction challenges, then you are likely going to succeed when you open a methadone clinic in your city. Please note that Methadone treatment is not a “quick fix” for treating opioid addiction.
Suggested for You
- Dental Clinic Business Plan [Sample Template]
- Medical Clinic and Practice Business Plan [Sample Template]
- Weight Loss Clinic Business Plan [Sample Template]
- Wholesale Pharmacy Business Plan [Sample Template]
- Aesthetic Clinic Business Plan [Sample Template]
The National Institute on Drug Abuse (NIDA) notes that when it comes to methadone maintenance, 12 months is considered to be the minimum length of treatment, and for some patients, treatment can go for many years in order to maintain sobriety.
If you are indeed interested in opening a methadone clinic, you should know what licensing and certification requirements would be needed from you by the state in which you would be operating from, especially as licensing caries depending on the state.
Asides licensing, you would need to know the minimum personnel that would be needed for your methadone clinic depending on the scale of business you intend to run.
At a minimum, you would require a licensed therapist, psychiatrist, nurses, and certified staff that would meet the staff-to-client ration that would meet the guidelines of the state you would be operating in.
A Sample Methadone Clinic Business Plan Template
1. industry overview.
Methadone treatment is one of the most effective and available treatment methods for opioid addiction in the united states of America and elsewhere in developed countries. As a matter of fact, one of the most well-known, but often misunderstood treatment options for opioid addiction is methadone.
The FDA-approved and highly-regulated methadone, which is distributed at outpatient clinics, manages withdrawal symptoms and side effects of opioid withdrawal and can help aid in the overall recovery process. Methadone clinic provides medication assisted treatment (MAT) that includes methadone for patients who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers.
Please note that methadone is administered by medical staff once a day, in a liquid solution. Methadone is only to be provided at a licensed methadone clinic under the guidance of trained healthcare providers.
Methadone clinic is a business that is grouped under the mental health and substance abuse centers industry and players in this industry includes establishments that primarily provide residential care and treatment for patients with mental illnesses, drug addiction and alcoholism.
Industry services include lodging, supervision, evaluation and counseling. Medical services may be available, though these are incidental to counseling, mental rehabilitation and support services. The mental health and substance abuse centers industry is indeed a very large industry and pretty much thriving in developed countries such as United States of America, France, United Kingdom, Germany, Australia and Italy et al.
Statistics has it that in the United States of America alone, there are about 8,216 licensed and registered mental health and substance abuse centers (methadone clinics inclusive) responsible for employing about 231,941 employees and the industry rakes in a whooping sum of $18 billion annually with an annual growth rate projected at 4.6 percent between 2014 and 2019.
It is important to state that the company holding the largest market share in the Drug & Alcohol Rehabilitation Clinics industry is Acadia Healthcare Company Inc.
A recent report released by IBISWorld shows that over the five years to 2019, industry revenue is estimated to grow an annualized 4.6 percent to $17.6 billion. In 2019 alone, revenue is estimated to grow 3.0 percent. Due to a broad range of focuses and treatment approaches offered by programs, profit margins vary significantly between operators.
Some of the factors that encourages entrepreneurs to open their own methadone clinic could be that the business is a thriving business and most methadone clinics get support and grants from government and donor agencies.
In conclusion, in order to become successful as a methadone clinic operator, you should be able to find it pretty easy to connect with people and constructively discuss their problems and issues. Excellent written and verbal communications skills and an analytical approach will serve you well in this line of business. Plus, you should know how to reach out to your target market and partner with the government and NGOs.
2. Executive Summary
Jason Collins® Methadone Clinic, Inc. is a standard and licensed methadone clinic that will be located in the heart of Rio Rancho – New Mexico in a neatly renovated and secured spacious clinic facility. Our methadone clinic is specifically designed and equipped with the needed facilities / gadgets to give comfort and security to all our patients irrespective of the religious affiliations, their race, and health condition.
Jason Collins® Methadone Clinic, Inc. will carry out standard methadone maintenance and treatments, in coordination with the other medication assisted treatment programs (including individual, group and family counseling, 12-step programs, and community-based resources), with the aim to effectively fight opioid addiction.
We will manage withdrawal symptoms and side effects of opioid withdrawal and can help aid in the overall recovery process. We will adhere to all standards and regulations to ensure patients get the exact methadone dosage they need in the time they need it in order to achieve their goals of long-term sobriety.
Jason Collins® Methadone Clinic, Inc. is a family owned and managed business that believe in the passionate pursuit of excellence and financial success with uncompromising services and integrity which is why we have decided to venture into the mental health and substance abuse centers industry by establishing our own methadone clinic.
We are certain that our values will help us drive the business to enviable heights and also help us attract the numbers of inpatients and outpatients customers that will make our facility fully occupied year in year out.
Despite the fact that we are a methadone clinic, we are going to be a health conscious and customer-centric with a service culture that will be deeply rooted in the fabric of our organizational structure and indeed at all levels of the organization.
With that, we know that we will be enables to consistently achieve our set business goals, increase our profitability and reinforce our positive long-term relationships with our clientele (inpatient and outpatient clines), partners (vendors), and all our employees as well.
Jason Collins® Methadone Clinic, Inc. is a family business that is owned and managed by Dr. Jason Collins and his immediate family.
Dr. Jason Collins is a licensed therapist, and psychiatrist with well over 25 years of experience working for leading brand in the industry. He has a Master’s Degree in Public Health and he is truly passionate when it comes to treating people who are addicted to drugs, and opioids et al.
3. Our Products and Services
Jason Collins® Methadone Clinic, Inc. is set to operate a standard methadone clinic in Rio Rancho – New Mexico. The fact that we want to become a force to reckon with in the mental health and substance abuse centers industry means that we will provide our patients with the needed treatments and care.
In all that we do, we will ensure that our inpatients and outpatients are satisfied and are willing to recommend our clinic to their family members and friends.
We are in the methadone clinic line of business to deliver excellent services and to make profits and we are willing to go the extra mile within the law of the United States to achieve our business goals, aims and objectives. We will offer the following services;
- Provide medication assisted treatment (MAT) that includes methadone for patients who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers
- Provide standard methadone maintenance and treatments, in coordination with the other medication assisted treatment programs (including individual, group and family counseling, 12-step programs, and community-based resources), with the aim to effectively fight opioid addiction
- Manage withdrawal symptoms and side effects of opioid withdrawal and can help aid in the overall recovery process.
4. Our Mission and Vision Statement
- Our vision is to become the number one choice when it comes to methadone maintenance and treatments in the whole of New Mexico and also to be amongst the top 5 methadone clinic facilities in the United States of America within the next 5 years.
- Our mission is to build a methadone clinic that will contribute in no smaller measure in reducing addictions and mental health ailments by providing medication assisted treatment (MAT) that includes methadone for patients who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers in the whole of Rio Rancho – New Mexico and environs.
- We want to meet and surpass the needs of all our patients and to build a profitable and successfully business.
Our Business Structure
Jason Collins® Methadone Clinic, Inc. is a business that will be built on a solid foundation. From the outset, we have decided to recruit only qualified professionals (methadone clinic workers administrator, nurse’s aides, medication management counselors, psychiatrists, and rehabilitation counselors) to man various job positions in our organization.
We are quite aware of the rules and regulations governing the mental health and substance abuse centers industry which is why we decided to recruit only well experienced and qualified employees as foundational staff of the organization.
We hope to leverage on their expertise to build our business brand to be well accepted in New Mexico and the whole of the United States.
When hiring, we will look out for applicants that are not just qualified and experienced, but homely, honest, customer centric and are ready to work to help us build a prosperous business that will benefit all the stake holders (the owners, workforce, and customers).
As a matter of fact, profit-sharing arrangement will be made available to all our management staff and it will be based on their performance for a period of five years or more. This are the positions that will be available at Jason Collins® Methadone Clinic, Inc.;
- Chief Medical Director
- Facility Administrator (Human Resources and Admin Manager)
- Addiction Treatment Specialist / Nurse
- Sales and Marketing Executive
- Accounting Officer
- Security Officer
5. Job Roles and Responsibilities
Chief Medical Director:
- Increases management’s effectiveness by recruiting, selecting, orienting, training, coaching, counseling, and disciplining managers; communicating values, strategies, and objectives; assigning accountabilities; planning, monitoring, and appraising job results; developing incentives; developing a climate for offering information and opinions; providing educational opportunities.
- Creating, communicating, and implementing the organization’s vision, mission, and overall direction – i.e. leading the development and implementation of the overall organization’s strategy.
- Responsible for fixing prices and signing business deals
- Responsible for providing direction for the business
- Responsible for signing checks and documents on behalf of the company
- Evaluates the success of the organization
- Reports to the board.
Facility Administrator (Admin and HR Manager)
- Responsible for overseeing the smooth running of HR and administrative tasks for the organization
- Design job descriptions with KPI to drive performance management for clients
- Regularly hold meetings with key stakeholders to review the effectiveness of HR Policies, Procedures and Processes
- Maintains office supplies by checking stocks; placing and expediting orders; evaluating new products.
- Ensures operation of equipment by completing preventive maintenance requirements; calling for repairs.
- Defining job positions for recruitment and managing interviewing process
- Carrying out staff induction for new team members
- Responsible for training, evaluation and assessment of employees
- Responsible for arranging travel, meetings and appointments
- Updates job knowledge by participating in educational opportunities; reading professional publications; maintaining personal networks; participating in professional organizations.
- Oversee the smooth running of the daily home activities.
Addiction Treatment Specialist/Nurse
- Manage withdrawal symptoms and side effects of opioid withdrawal and can help aid in the overall recovery process
- Develop a treatment plan in consultation with other professionals, such as doctors, therapists, and psychologists
- Create rehabilitation or treatment plans based on clients’ values, strengths, limitations, and goals
- Assist patients in creating strategies to develop their strengths and adjust to their limitations
- Monitor patients progress and adjust the rehabilitation or treatment plan as necessary
- Advocate for the rights of people who are just coming out of drug addictions and alcoholism to live in the community and work in the job of their choice.
Marketing and Sales Executive
- Identify, prioritize, and reach out to new clients, and business opportunities et al
- Identifies development opportunities; follows up on development leads and contacts
- Writing winning proposal documents, negotiate fees and rates in line with organizations’ policy
- Responsible for handling business research, market surveys and feasibility studies for clients
- Responsible for supervising implementation, advocate for the customer’s needs, and communicate with clients
- Develop, execute and evaluate new plans for expanding increase sales
- Document all customer contact and information
- Represent Jason Collins® Methadone Clinic, Inc. in strategic meetings
- Help increase sales and growth for Jason Collins® Methadone Clinic, Inc.
Accountant/Cashier
- Responsible for preparing financial reports, budgets, and financial statements for the organization
- Provides managements with financial analyses, development budgets, and accounting reports; analyzes financial feasibility for the most complex proposed projects; conducts market research to forecast trends and business conditions.
- Responsible for financial forecasting and risks analysis.
- Performs cash management, general ledger accounting, and financial reporting for the organization
- Responsible for developing and managing financial systems and policies
- Responsible for administering payrolls
- Ensuring compliance with taxation legislation
- Handles all financial transactions for Jason Collins® Methadone Clinic, Inc.
- Serves as internal auditor for Jason Collins® Methadone Clinic, Inc.
Security Officers
- Ensure that the clinic facility is secured at all time
- Control traffic and organize parking
- Give security tips to staff members from time to time
- Patrols around the building on a 24 hours basis
- Submit security reports weekly
- Any other duty as assigned by the facility administrator
- Responsible for cleaning the clinic facility at all times
- Ensure that toiletries and supplies don’t run out of stock
- Assist our inpatients and outpatients when they need to take their bath and carry out other household tasks
- Cleans both the interior and exterior of the facility
- Handle any other duty as assigned by the facility manager
6. SWOT Analysis
Jason Collins® Methadone Clinic, Inc. is set to become one of the leading methadone clinics in New Mexico which is why we are willing to take our time to cross every ‘Ts’ and dot every ‘Is’ as it relates to our business. We want our methadone clinic to be the number one choice of all those hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers in Rancho and other cities in New Mexico.
We know that if we are going to achieve the goals that we have set for our business, then we must ensure that we build our business on a solid foundation. We must ensure that we follow due process in setting up the business.
Even though our Chief Medical Director (owner) has a robust experience in treating people who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers.
We still went ahead to hire the services of business consultants that are specialized in setting up new businesses to help our organization conduct detailed SWOT analysis and to also provide professional support in helping us structure our business to indeed become a leader in the mental health and substance abuse centers industry.
This is the summary of the SWOT analysis that was conducted for Jason Collins® Methadone Clinic, Inc.;
Our strength lies in the fact that we have a team of well qualified professionals manning various job positions in our organization.
As a matter of fact, they are some of the best hands in the whole of Rio Rancho – New Mexico. Our location, the Business model we will be operating on (inpatient and outpatient treatments), well equipped and secured clinic facility and our excellent customer service culture will definitely count as a strong strength for us.
Jason Collins® Methadone Clinic, Inc. is a new business which is own by an individual (family), and we may not have the financial muscle to sustain the kind of publicity we want to give our business and also to attract some of the highly experienced hands in the mental health and substance abuse centers industry in the United States of America.
- Opportunities:
Federal funding for Medicare and Medicaid has increased during the period as states have expanded Medicaid coverage to a greater number of low-income individuals. An increase in coverage enables more individuals struggling with substance use and mental illness to access industry services.
Currently, an estimated 41.9 percent of industry revenue is derived from Medicaid and Medicare reimbursement payments. in 2023, federal funding for Medicare and Medicaid is expected to increase, presenting a potential opportunity for the industry.
Individuals seeking treatment for mental health or substance use disorders have many options in regard to types of providers and treatment models.
As a result, industry operators experience external competition from numerous sources, including from short-term inpatient and outpatient service providers in the Mental Health and Substance Abuse Clinics industry. External competition is anticipated to remain high in 2019, posing a potential threat to operators in the Mental Health and Substance Abuse Centers industry.
7. MARKET ANALYSIS
- Market Trends
A notable trend shows that the revenue and wages for methadone clinics have largely been affected due to the recession and also a slight fund drop in 2012 from federal funding of Medicaid and Medicare as a result of a rise in premiums but the effect is wearing off as the industry has largely recovered.
Also, the economy which is constantly improving is expected to boost revenue for the methadone clinic business industry from 2015 to 2022. More companies entering into this industry are doing so due to the fact that there is an increasing focus on outpatient services, which are considered less costly than inpatient care, and which is also more desirable for insurance providers.
The demand for methadone clinics is largely driven by the availability of various factors such as new drugs and treatments, funding policies as well as insurance programs. Profitability for individual facilities depends on controlling costs as well as referrals.
Large scale methadone clinics usually have more advantage when purchasing as well as marketing to sources that would provide these referrals. However, small scale companies have more leverage in competition by providing superior service to patients, integration of treatments with follow-up procedures, and specialist treatment.
Lastly, most emergency physicians have treated methadone maintenance therapy (MMT) clients in the ED, and have dealt with withdrawal, missed appointments, and overdose.
No doubt the mental health and substance abuse centers industry will continue to grow and become more profitable because the aging baby-boomer generation in United States are expected to drive increasing demand for this specialized services and care.
8. Our Target Market
Anyone can walk into an MMT clinic and request treatment. Initial screening exams and interviews determine the applicant’s eligibility and the process includes an assessment of their readiness to accept treatment. Ongoing, if not daily interventions, are required to keep the patient in the system and off the opioid.
The addiction severity index collects basic information, and it can be used to track progress. Much of the information is supplied by the addict, and truthfulness on their part is paramount for success.
In view of the above, the fact that we are going to open our doors to a wide range of customers does not in any way stop us from abiding by the rules and regulations governing the mental health and substance abuse centers industry in the United States.
Our staff are well – trained to effectively service our customers and give them value for their monies. Our customers can be categorized into the following;
- Everyone who is hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers amongst others.
Our Competitive Advantage
To be highly competitive in the mental health and substance abuse centers industry means that you should be able to secure a conducive and secured clinic facility, deliver consistent quality service and should be able to record good testimonial of changed lives; of people who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers in and around Rio Rancho – New Mexico.
Jason Collins® Methadone Clinic, Inc. is coming into the market well prepared to favorably compete in the industry. Our clinic facility is well positioned (centrally positioned) and visible, we have good security and the right ambience for people who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers.
Our staff are well groomed in all aspect of methadone clinic and treatment services and all our employees are trained to provide customized customer service to all our inpatient and outpatient customers. Our services will be carried out by highly trained professional who know what it takes to give our highly esteemed inpatients and outpatients value for their money.
Lastly, all our employees will be well taken care of, and their welfare package will be among the best within our category (startups methadone clinic business and other related businesses in the United States) in the industry. It will enable them to be more than willing to build the business with us and help deliver our set goals and achieve all our business aims and objectives.
9. SALES AND MARKETING STRATEGY
- Sources of Income
Jason Collins® Methadone Clinic, Inc. will ensure that we do all we can to maximize the business by generating income from every legal means within the scope of our industry. We will generate income by offering the following services;
10. Sales Forecast
One thing is certain, there would always be patients who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers who would need the services of methadone clinic.
We are well positioned to take on the available market in Rio Rancho – New Mexico and we are quite optimistic that we will meet our set target of generating enough income / profits from the first six month of operations and grow our methadone clinic business and our inpatients and outpatients’ base.
We have been able to critically examine the methadone clinic services market and we have analyzed our chances in the industry and we have been able to come up with the following sales forecast. The sales projections are based on information gathered on the field and some assumptions that are peculiar to similar startups in Rio Rancho – New Mexico.
Below is the sales projection for Jason Collins® Methadone Clinic, Inc., it is based on the location of our clinic and of course the wide range of related services that we will be offering;
- First Fiscal Year (FY1): $75,000 (From Self – Pay Clients / Patients): $150,000 (From Health Insurance Companies)
- Second Fiscal Year (FY2): $150,000 (From Self – Pay Clients / Patients): $350,000 (From Health Insurance Companies)
- Third Fiscal Year (FY3): $200,000 (From Self – Pay Clients / Patients): $650,000 (From Health Insurance Companies)
N.B : This projection is done based on what is obtainable in the industry and with the assumption that there won’t be any major economic meltdown and natural disasters within the period stated above. Please note that the above projection might be lower and at the same time it might be higher.
- Marketing Strategy and Sales Strategy
The marketing and sales strategy of Jason Collins® Methadone Clinic, Inc. will be based on generating long-term personalized relationships with our inpatients and outpatients. In order to achieve that, we will ensure that we offer top notch all – round methadone clinic services at affordable prices compare to what is obtainable in New Mexico and other state in the US.
All our employees will be well trained and equipped to provide excellent and knowledgeable services as it relates to our business. We know that if we are consistent with offering high quality service delivery and excellent customer service, we will increase the number of our inpatients and outpatients by more than 25 percent for the first year and then more than 40 percent subsequently.
Before choosing a location for Jason Collins® Methadone Clinic, Inc., we conducted a thorough market survey and feasibility studies in order for us to be able to be able to penetrate the available market and become the preferred choice for patients who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers in Rio Rancho and other cities in New Mexico.
We have detailed information and data that we were able to utilize to structure our business to attract the numbers of customers we want to attract per time.
We hired experts who have good understanding of the mental health and substance abuse centers industry to help us develop marketing strategies that will help us achieve our business goal of winning a larger percentage of the available market in New Mexico.
In summary, Jason Collins® Methadone Clinic, Inc. will adopt the following sales and marketing approach to win customers over;
- Introduce our business by sending introductory letters to patients who are hoping to achieve sobriety from opioid addiction, including addiction to heroin and prescription painkillers and other stake holders in and around Rio Rancho – New Mexico
- Advertise our business in community – based newspapers, local TV and local radio stations
- List our business on yellow pages ads (local directories)
- Leverage on the internet to promote our business
- Engage in direct marketing
- Leverage on word of mouth marketing (referrals)
- Enter into business partnership with prisons, government agencies and NGOs that work with drug addicts, pornography addicts and other substance abusers.
- Attend drug and substance abuse related seminars/expos.
11. Publicity and Advertising Strategy
We are in the methadone clinic business to become one of the market leaders and also to maximize profits hence we are going to explore all available conventional and non – conventional means to promote Jason Collins® Methadone Clinic, Inc.
Jason Collins® Methadone Clinic, Inc. has a long – term plan of building methadone clinic facilities in key cities in the United States of America which is why we will deliberately build our brand to be well accepted in Rio Rancho – New Mexico before venturing out.
As a matter of fact, our publicity and advertising strategy is not solely for winning inpatients and outpatients (customers) over but to effectively communicate our brand to the general public. Here are the platforms we intend leveraging on to promote and advertise Jason Collins® Methadone Clinic, Inc.;
- Place adverts on both print (community – based newspapers and magazines) and electronic media platforms
- Sponsor relevant community programs that appeals to people who are addicted to drugs, alcohol and other substances
- Leverage on the internet and social media platforms like; Instagram, Facebook, twitter, YouTube, Google + et al to promote our brand
- Install our Bill Boards on strategic locations all around Rio Rancho – New Mexico
- Engage in roadshow from time to time in location with growing population of people prone to drug and substance abuse
- Distribute our fliers and handbills in target areas with high concentration of drug addicts and alcoholics
- Ensure that all our workers wear our branded shirts and our facility and all our vehicles are well branded with our company’s logo et al.
12. Our Pricing Strategy
In as much as methadone treatments are never free, they are an affordable option for those seeking care. The range of methadone treatment costs varies by clinic, and may be covered by private and public insurance, as well as Medicaid. Players in this industry offers methadone treatment that is covered by most insurance providers, and Medicaid.
Jason Collins® Methadone Clinic, Inc. will work towards ensuring that all our services are offered at highly competitive prices compare to what is obtainable in The United States of America. Be that as it may, we have put plans in place to offer discount services once in a while and also to reward our loyal inpatients and outpatients especially when they refer clients to us.
- Payment Options
The payment policy adopted by Jason Collins® Methadone Clinic, Inc. is all inclusive because we are quite aware that different customers prefer different payment options as it suits them but at the same time, we will ensure that we abide by the financial rules and regulation of the United States of America. Here are the payment options that Jason Collins® Methadone Clinic, Inc. will make available to her clients;
- Payment via bank transfer
- Payment with cash
- Payment via online bank transfer
- Payment via check
- Payment via Point of Sale Machines (POS Machine)
- Payment via bank draft
- Payment via mobile money
In view of the above, we have chosen banking platforms that will enable our client make payment for our treatment fee in our methadone clinic without any stress on their part. Our bank account numbers will be made available on our website and promotional materials to clients who may want to deposit cash or make online transfer for our services.
13. Startup Expenditure (Budget)
If you are looking towards starting a methadone clinic business, then you should be ready to go all out to ensure that you raise enough capital to cover some of the basic expenditure that you are going to incur. The truth is that starting this type of business does not come cheap.
You would need money to secure a standard clinic facility big enough to accommodate the number of inpatients you plan accommodating per time, you could need money to acquire medical supplies and you would need money to pay your workforce and pay bills for a while until the revenue you generate from the business becomes enough to pay them.
The items listed below are the basics that we would need when starting our methadone clinic business in the United States;
- The total fee for registering the business in the United States – $750.
- Legal expenses for obtaining licenses and permits – $1,500.
- Marketing promotion expenses for the grand opening of Jason Collins® Methadone Clinic, Inc. in the amount of $3,500 and as well as flyer printing (2,000 flyers at $0.04 per copy) for the total amount of – $3,580.
- The cost for hiring business consultant – $2,500.
- The cost for the purchase of insurance (general liability, workers’ compensation and property casualty) coverage at a total premium – $3,400.
- The cost for leasing a standard and secured facility in Rio Rancho – New Mexico for 2 years – $250,000
- The cost for facility remodeling – $50,000.
- Other start-up expenses including stationery ($500) and phone and utility deposits ($2,500).
- The total cost for computer software (Accounting Software, Payroll Software, CRM Software, Microsoft Office, QuickBooks Pro, drug interaction software, Physician Desk Reference software) – $7,000
- The total cost for Nurse and Drugs Supplies (Injections, Bandages, Scissors, et al) – $3,000
- Operational cost for the first 3 months (salaries of employees, payments of bills et al) – $100,000
- The cost for start-up inventory (stocking with a wide range of products such as toiletries, food stuffs and drugs et al) – $50,000
- Storage hardware (bins, rack, shelves,) – $3,720
- The cost for the purchase of furniture and gadgets (Beds, Computers, Printers, Telephone, TVs, tables and chairs et al): $4,000.
- The cost of Launching a Website: $700
- Miscellaneous: $10,000
We would need an estimate of seven hundred and fifty thousand dollars ($750,000) to successfully set up our methadone clinic in Rio Rancho – New Mexico. Please note that this amount includes the salaries of all the staff for the first month of operation.
Generating Funds/Startup Capital for Jason Collins® Methadone Clinic, Inc.
Jason Collins® Methadone Clinic, Inc. is a family business that is solely owned and financed by Dr. Jason Collins and his immediate family members.
They do not intend to welcome any external business partners which is why he has decided to restrict the sourcing of the start – up capital to 3 major sources. These are the areas Jason Collins® Methadone Clinic, Inc. intends to generate our start – up capital;
- Generate part of the start – up capital from personal savings
- Source for soft loans from family members and friends
- Apply for loan from my Bank
N.B: We have been able to generate about $200,000 (Personal savings $150,000 and soft loan from family members $50,000) and we are at the final stages of obtaining a loan facility of $550,000 from our bank. All the papers and document have been signed and submitted, the loan has been approved and any moment from now our account will be credited with the amount.
14. Sustainability and Expansion Strategy
The future of a business lies in the numbers of loyal customers that they have, the capacity and competence of the employees, their investment strategy and the business structure. If all of these factors are missing from a business (company), then it won’t be too long before the business close shop.
One of our major goals of starting Jason Collins® Methadone Clinic, Inc. is to build a business that will survive off its own cash flow without the need for injecting finance from external sources once the business is officially running.
We know that one of the ways of gaining approval and winning customers over is to offer treatments and services in our methadone clinic a little bit cheaper than what is obtainable in the market and we are well prepared to survive on lower profit margin for a while.
Jason Collins® Methadone Clinic, Inc. will make sure that the right foundation, structures and processes are put in place to ensure that our staff welfare are well taken of. Our company’s corporate culture is designed to drive our business to greater heights and training and retraining of our workforce is at the top burner.
As a matter of fact, profit-sharing arrangement will be made available to all our management staff and it will be based on their performance for a period of three years or more. We know that if that is put in place, we will be able to successfully hire and retain the best hands we can get in the industry; they will be more committed to help us build the business of our dreams.
Check List/Milestone
- Business Name Availability Check: Completed
- Business Registration: Completed
- Opening of Corporate Bank Accounts: Completed
- Securing Point of Sales (POS) Machines: Completed
- Opening Mobile Money Accounts: Completed
- Opening Online Payment Platforms: Completed
- Application and Obtaining Tax Payer’s ID: In Progress
- Application for business license and permit: Completed
- Purchase of Insurance for the Business: Completed
- Leasing of facility and remodeling the clinic facility: In Progress
- Conducting Feasibility Studies: Completed
- Generating capital from family members: Completed
- Applications for Loan from the bank: In Progress
- Writing of Business Plan: Completed
- Drafting of Employee’s Handbook: Completed
- Drafting of Contract Documents and other relevant Legal Documents: In Progress
- Design of The Company’s Logo: Completed
- Graphic Designs and Printing of Packaging Marketing / Promotional Materials: In Progress
- Recruitment of employees: In Progress
- Purchase of medical equipment and vans et al: In Progress
- Purchase of the needed furniture, racks, shelves, computers, electronic appliances, office appliances and CCTV: In progress
- Creating Official Website for the Company: In Progress
- Creating Awareness for the business both online and around the community: In Progress
- Health and Safety and Fire Safety Arrangement (License): Secured
- Opening party / launching party planning: In Progress
- Establishing business relationship with players in key industries, NGOs, government and third – party services providers: In Progress
Overview of Opioid Treatment Program Regulations by State
Restrictive rules put evidence-based medication treatment out of reach for many.
- Overview of Opioid Treatment Program Regulations by State (PDF)
Navigate to:
- Table of Contents

Opioid treatment programs (OTPs) are the only health care facilities that can offer patients all three forms of FDA-approved medication for opioid use disorder (OUD): methadone, buprenorphine, and injectable extended-release naltrexone. 1 But Pew found that nearly all states have rules governing OTPs that are not based in evidence and in turn limit access to care or worsen patient experience. 2
These rules governing the establishment, operation, and provision of care at OTPs exist at both the federal and state levels: The federal government establishes baseline requirements for OTPs, and states layer additional requirements on top of them. 3 Although debate over the future of federal methadone regulation is ongoing, state policymakers have the opportunity to act now to improve access to this medication and the quality of OTP services, as well as remove rules that go beyond federal restrictions and limit access to care. 4
This chartbook examines OTP regulations across all 50 states and the District of Columbia as of June 2021 in two areas:
Access to care: Regulations that affect the ease with which patients access care at OTPs, such as dictating whether one is located close to where they live or work, whether services are available at convenient times, or whether patients must obtain a government ID to start treatment.
Patient experience: Rules that affect how patients receive care, such as whether they receive medication to take at home or if they have to go to the clinic every day. State regulations can help or hinder access to high-quality, evidence-based care that is aligned with federal rules and tailored to meet patients’ needs.
Methadone is offered only in OTPs, which is one reason they are critical to reducing overdose deaths and providing lifesaving addiction treatment. State policymakers should review these rules and, where needed, revise them so that residents with OUD can access high-quality, lifesaving treatment.
Access to care
OTPs are not available in many communities. As of 2018, 80% of counties in the U.S., representing nearly a quarter of the population, had no OTPs. 5 Even when a facility is nearby, patients may have challenges accessing care if services aren’t available at convenient times or patients must show a government ID to receive methadone.
How states choose to regulate OTPs plays a role in how great these access challenges are.
Restrictions on new OTPs
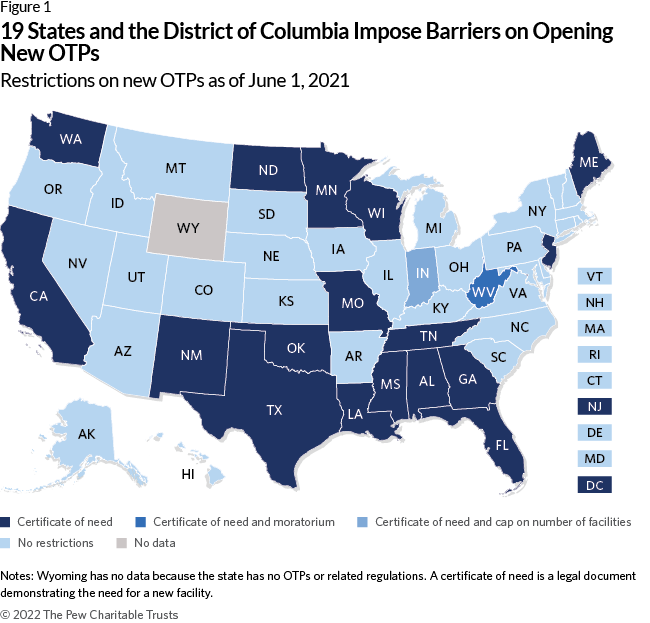
Nineteen states and the District of Columbia restrict providers from opening new OTPs in some way:
All 20 require a certificate of need, a legal document demonstrating that there is a need for a new facility. And Indiana limits the number of new facilities that can open.
West Virginia is the most restrictive state, with a legal moratorium disallowing new OTPs.
Medication units
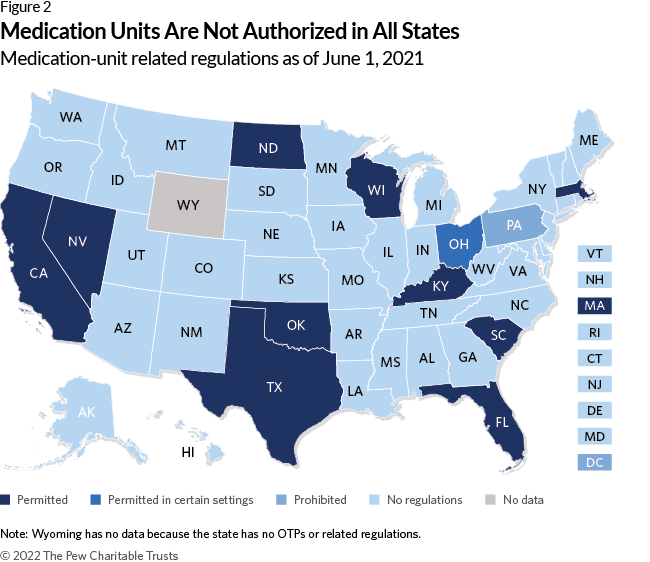
Conversely, allowing OTPs to open medication units—locations that may offer dosing and urine screens and are affiliated with an existing OTP—can make treatment more convenient for patients who receive methadone by expanding the locations where they can receive care. 6
Eleven states explicitly permit medication units, while one— Pennsylvania—prohibits them. Ohio specifically allows medication units to operate in homeless shelters, jails, prisons, local boards of public health, community health centers, residential treatment providers, small counties, and counties in Appalachia. 7
Pharmacy-related barriers
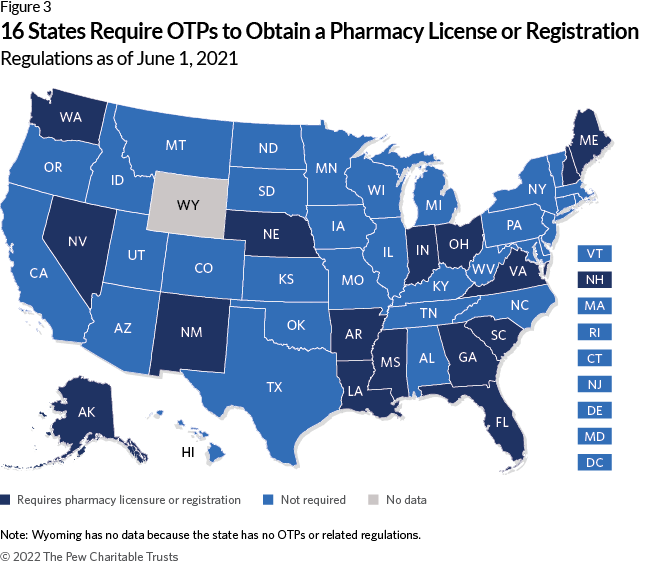
Requiring pharmacy licensure or registration.
Another barrier to establishing new OTPs mandates that they be licensed or registered as pharmacies.
This is not required by federal law. 8 Sixteen states have these rules.
Applying general pharmacy regulations to OTPs
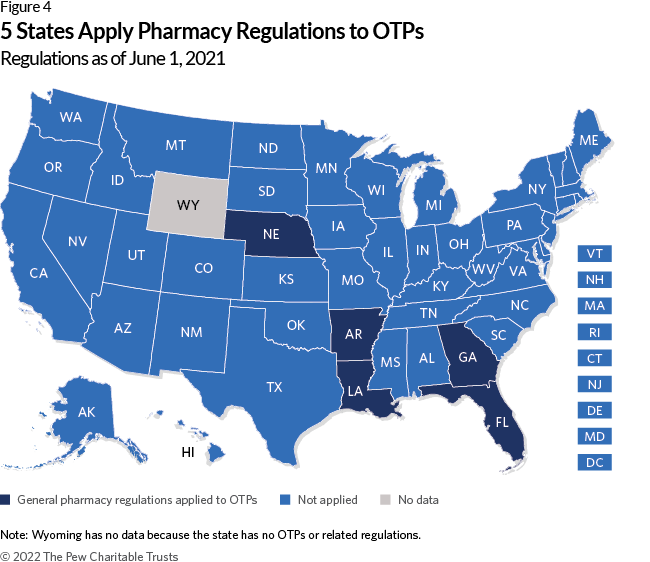
States that require OTPs to follow their general pharmacy regulations— which apply to a neighborhood drugstore that fills prescriptions for many medications that are used for multiple conditions—make establishing new OTPs even more challenging.
Five states apply general pharmacy regulations to OTPs.
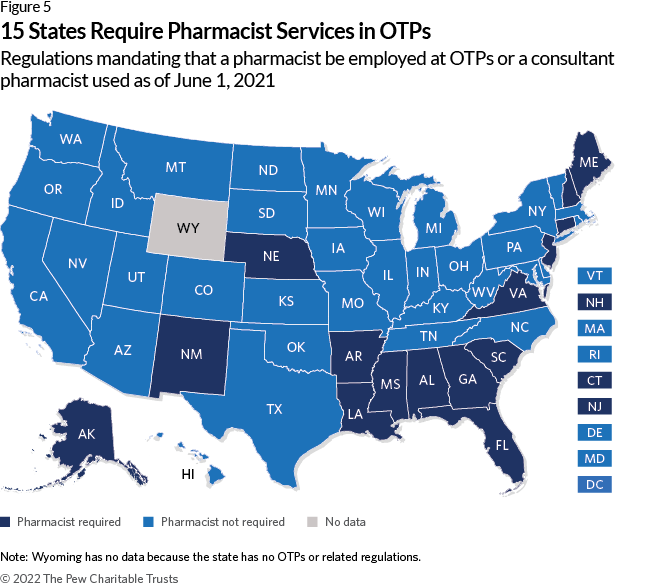
Requiring pharmacist services
Federal law allows methadone administration by a variety of licensed health care professionals including registered nurses, licensed practical nurses, or other health care professionals who are otherwise authorized to dispense opioids. 9
However, 15 states require OTPs to hire a pharmacist or a consultant pharmacist, who provides guidance on the appropriateness and safety of medication use. 10
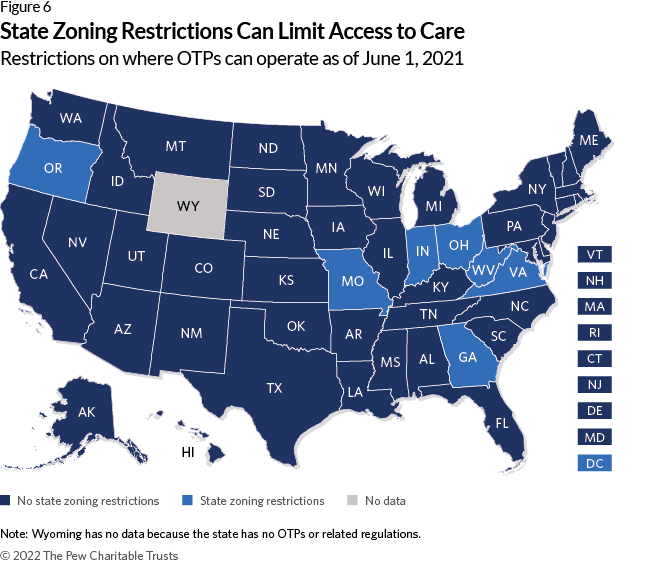
State zoning restrictions
Restrictions on where an OTP can operate, beyond those that apply to other medical facilities, is not considered to be best practice. 11
Seven states and the District of Columbia have these rules. However, in the District, the regulation supports access to care because OTPs are required to be located near public transportation.
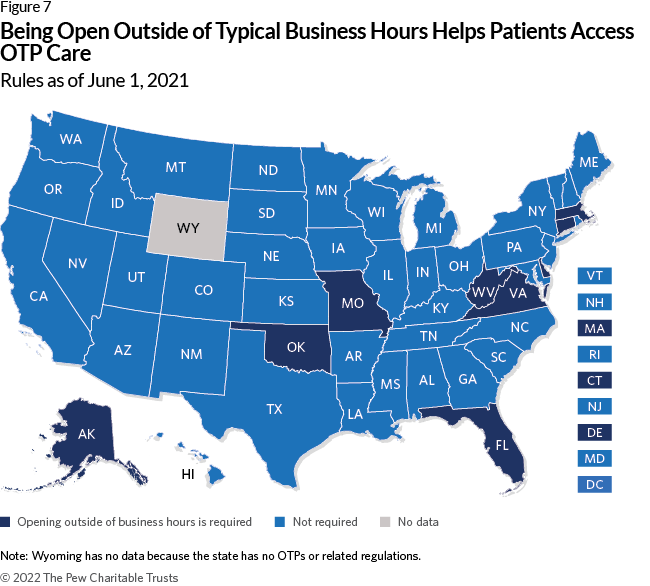
Hours of operation
Requiring OTPs to be open outside of regular business hours (e.g., outside of 8 a.m.-5 p.m.) provides flexibility for clients who may find it difficult to go to the clinic each day due to other responsibilities such as work or family obligations. 12
Nine states require OTPs to be open outside of business hours.
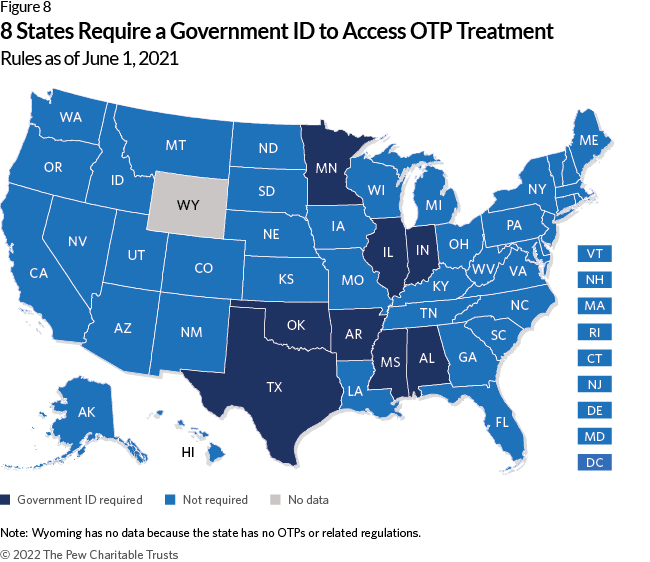
Government ID
Some people—including undocumented immigrants, people who have been incarcerated, people experiencing homelessness, and many other populations— face challenges in obtaining an ID. 13 Requiring a client to show government ID to be admitted to an OTP can be a barrier to care.
Eight states have this requirement.
Conversely, California allows OTPs to provide patient identification cards that include the individual’s photo, a unique identifier, and a physical description. 14 This allows the OTP to verify the patient’s identity before dispensing methadone without requiring a government ID.
Patient experience
Federal rules already dictate the frequency of urine drug screens and whether patients can receive take-home methadone—a supply of medication for opioid use disorder that allows patients to avoid having to go to the clinic each day—as well as other aspects of OTP care.
When states add additional rules, they further constrain providers from offering individualized, high-quality care that meets their patients’ needs.
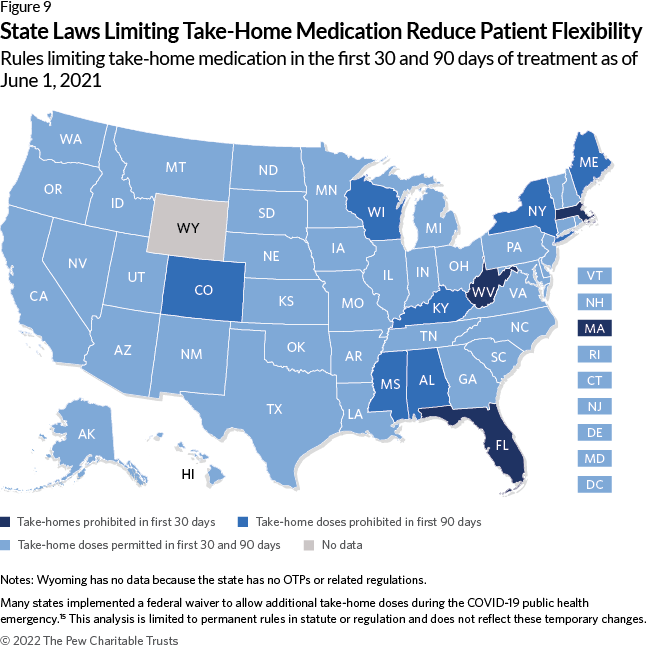
Eligibility for take-home doses
Before the COVID-19 public health emergency, federal rules allowed a single take-home dose per week in the first 90 days of treatment if patients met specific stability criteria. 16 This requirement has not been permanently changed, and only temporary flexibilities have been granted as of April 2022. 17
Ten states go beyond federal rules by prohibiting take-home doses in the first 30 days of treatment. Of these, seven states prohibit this practice during the full first 90 days of care.

Additional stability criteria
Federal rules require that patients meet eight stability criteria to receive take-home doses:
- Absence of recent abuse of drugs (opioid or non-narcotic), including alcohol.
- Regularity of clinic attendance.
- Absence of serious behavioral problems at the clinic.
- Absence of known recent criminal activity, e.g., drug dealing.
- Stability of the patient’s home environment and social relationships.
- Length of time in comprehensive maintenance treatment.
- Assurance that take-home medication can be safely stored within the patient’s home.
- Whether the rehabilitative benefit the patient derived from decreasing the frequency of clinic attendance outweighs the potential risks of diversion . 18
Ten states impose additional stability criteria. For example, Missouri also requires that patients “demonstrate a level of stability as evidenced by … employment, actively seeking employment, or attending school if not retired, disabled, functioning as a homemaker, or otherwise economically stable.” 19
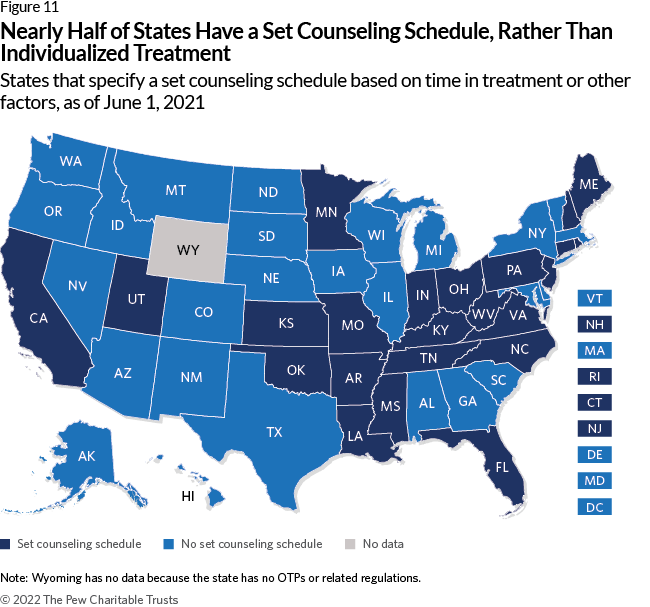
Inflexible counseling requirements
Requiring clients to participate in a set counseling schedule (e.g., a minimum number or length of sessions) to stay in treatment or receive take-home medication is not in line with federal regulations, and strict counseling requirements can reduce retention in treatment. 20
Twenty-three states impose a set counseling schedule. These rules can be tied to eligibility for take-home medication. In Oklahoma, for example, patients move through five phases of treatment based on time in treatment and compliance with program rules, including participation in a set number of individual and group counseling sessions per phase. Each phase provides more take-home doses. 21
These rules are not aligned with evidence, which shows that medication for opioid use disorder can be effective without counseling. 22

Forcing people to leave treatment for violating program rules
It’s common for people who use opioids to also use multiple substances as well as return to opioid use, even among people on medications for opioid use disorder (MOUD). 23 Although federal guidelines and recommendations list neither as a reason to end medication treatment and research supports that continuing MOUD is safer than suddenly stopping treatment, some programs “administratively discharge”—or terminate—clients because of continued drug use. 24
Only Massachusetts and South Dakota prohibit administrative discharge for not being abstinent.
All states allow administrative discharge for missed methadone doses, although federal guidelines recommend reassessing patients who miss more than four methadone doses rather than terminating their treatment. 25
All states also allow administrative discharge for nonparticipation in counseling or other ancillary services, even though the American Society of Addiction Medicine says the decision to decline these services should not affect a patient’s ability to obtain MOUD. 26
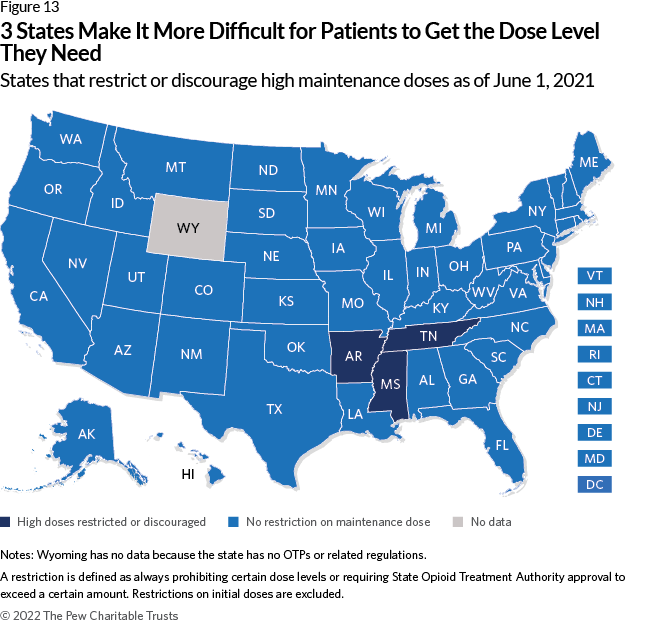
Restricting medication dosage
Doses that are too low may not effectively reduce drug cravings or use. 27 Restricting or discouraging higher doses of medication may cause patients to discontinue treatment. This restriction is also not aligned with federal guidelines or evidence, as higher doses can lead to greater reductions in drug use among patients with OUD. 28
Three states have these rules.
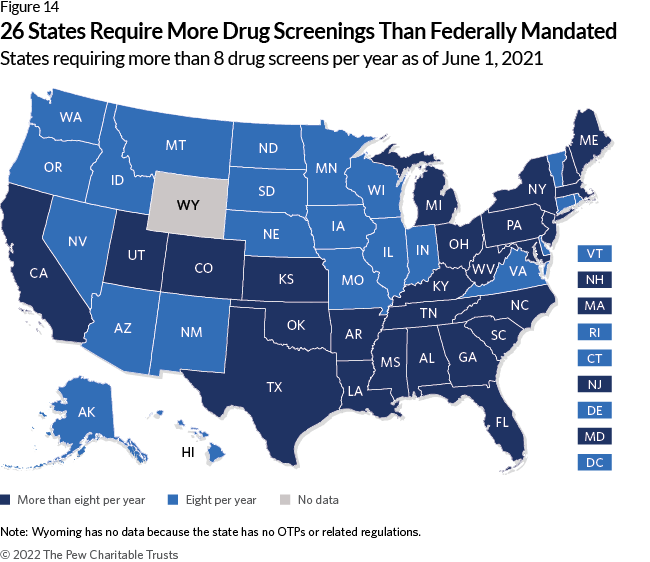
Urine drug screenings
Requiring additional tests.
Federal rules require eight drug tests per year. 29 Requiring additional tests places a burden on patients and, according to preliminary research, may not be as necessary for patient safety as once thought, and may also raise the cost of treatment. 30
Twenty-six states require more than eight annual drug screenings.
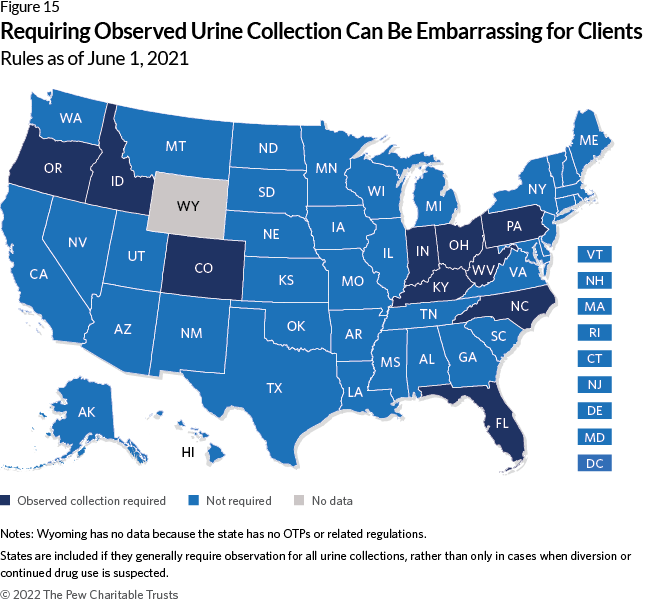
Observing urine specimen collection
Ten states have rules requiring OTPs to observe patients during urine sample collection, which can be embarrassing and degrading for clients. 31 According to one, “I don’t like somebody looking at me, or behind me … it’s not a very pleasant experience for anybody. Actually, I think it’s undignified, and I feel it’s wrong.” 32

Establishing a treatment goal not based in evidence
Evidence supports that long-term treatment can be more beneficial for patients in terms of overdose risk, employment, health, and criminal justice involvement; according to the American Society of Addiction Medicine, “There is no recommended time limit for pharmacological treatment with methadone.” 33
But eight states have rules that establish discontinuation as the goal of treatment. These regulations may encourage providers and patients to stop treatment when doing so is not necessary and can increase overdose death. 34
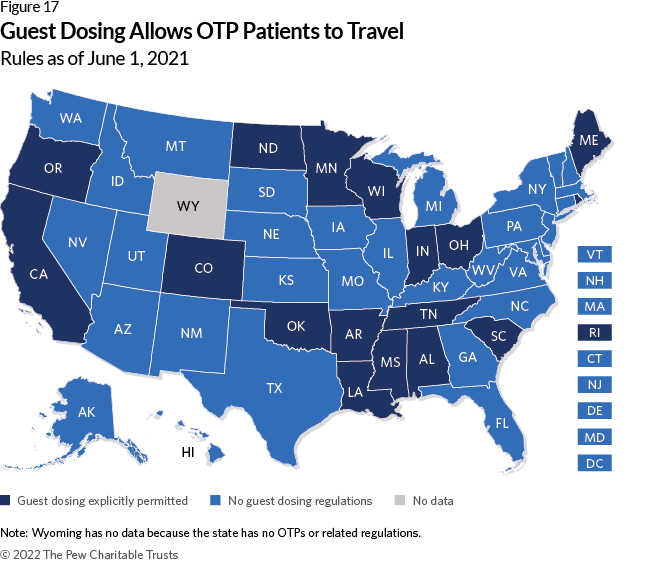
Allowing patients flexibility while traveling
Although other regulations can worsen patient experience, states can also improve it through regulations.
Explicitly allowing guest dosing— that is, temporarily getting methadone from an OTP other than the one at which someone is a patient—is one way to help. This provides flexibility for patients who are traveling. 35
Seventeen states have rules that explicitly allow this practice, though it may still be permitted in states without these regulations.
Data shows that many states make it harder for OTP patients to access and remain in treatment in a variety of ways.
As overdose deaths continue to climb, state policymakers should review these rules and make changes so that more people get the lifesaving treatment provided in these settings.
Methodology
Identifying regulatory language.
Pew reviewed both statutes and administrative codes for the District of Columbia and all states, except for Wyoming, using Lexis. Wyoming was excluded because the state does not have any OTPs or related regulations.
Initial citations were drawn from Jackson et al. (2020) and the Prescription Drug Abuse Policy System “Requirements for Licensure and Operations of Medications for Opioid Use Disorder Treatment.” 36 In addition to these sources, Pew reviewed the section of statutes providing rule-making authority to the agency that promulgated regulations in the administrative code. If either regulations or statutes referred to Board of Pharmacy oversight, Pew also examined the relevant sections of administrative code produced by that body.
Data represents state rules codified in statute and administrative code as of June 2021. It does not reflect any temporary changes such as executive orders or policy statements states may have issued due to the COVID-19 pandemic. 37
Pew developed an initial list of codes based on a review of the OTP federal guidelines and literature on best practices. Using NVivo, the research team that has years of OUD research and policy expertise initially coded five states. The regulations for each state were independently coded by two members of the research team. Pew then held a coding meeting to discuss our findings and refine the codebook, and then recoded these states. The research team then conducted a test of inter-rater reliability, which ensures consistency in coding among research team members, resolved coding discrepancies, and refined the codebook further. Pew then coded five additional states, held another coding meeting, and finalized the codebook. (See Appendix)
Quality control
Pew conducted two quality control steps—comparing our findings with existing research and verifying results with state officials.
Comparison with existing research
Pew compared the findings with previously conducted reviews of OTP regulations. 38 In most cases, disagreement between Pew’s findings and these publications were due to differences in definition or because regulations had been updated since those reviews were conducted. If we identified an error based on these comparisons, we updated our data.
Verification with state opioid treatment authorities (SOTAs)
Between June and August 2021, Pew sent the results of each jurisdiction’s regulatory review to their state opioid treatment authority, or SOTA, the official charged with overseeing OTPs. These officials were identified by a list maintained by the Substance Abuse and Mental Health Services Administration. 39 For Wyoming, Pew contacted the deputy administrator of the Behavioral Health Division because the state does not have a SOTA.
Each SOTA was asked to verify whether Pew’s interpretation of their state’s OTP rules was correct, and if it was not, to provide updated information.
After sending multiple reminders to each official, Pew received responses from all but 12 states (Delaware, Kansas, Mississippi, Missouri, New Hampshire, New York, Rhode Island, Tennessee, Utah, Vermont, Washington, and Wisconsin). If the SOTA disagreed with the research team’s findings, Pew either updated the research or explained the decision not to. In those cases where we did not update our findings, those discrepancies were either due to differences in definitions or because updated regulatory language was not in effect until after June 1, 2021, our cutoff date.
- The Pew Charitable Trusts, “Medications for Opioid Use Disorder Improve Patient Outcomes” (2020), https://www.pewtrusts.org/en/research-and-analysis/factsheets/2020/12/medications-for-opioid-use-disorder-improve-patient-outcomes .
- The Pew Charitable Trusts, “Improved Opioid Treatment Programs Would Expand Access to Quality Care” (2022), https://www.pewtrusts.org/-/media/assets/2022/03/improve-opioid-treatment-programs-to-expand-access.pdf .
- American Society of Addiction Medicine, “Regulation of the Treatment of Opioid Use Disorder With Methadone” (2021), https://www.asam.org/advocacy/public-policystatements/details/public-policy-statements/2021/11/16/the-regulation-of-the-treatment-of-opioid-use-disorder-with-methadone .
- M. Hawryluk, “Calls to Overhaul Methadone Distribution Intensify, but Clinics Resist,” KHN, March 3, 2022, https://khn.org/news/article/opioid-methadone-treatmentoverhaul-clinics-resist-addiction/ .
- J.H. Duff and J.A. Carter, “Location of Medication-Assisted Treatment for Opioid Addiction: In Brief” (Congressional Research Service, 2019), https://www.everycrsreport.com/files/20190624_R45782_ed39091fadf888655ebd69729c3180c3f7e550f6.pdf .
- Substance Abuse and Mental Health Services Administration, “OTP Services Through Medication Units” (2022), https://www.samhsa.gov/medication-assisted-treatment/become-accredited-opioid-treatment-program care; A. McBournie et al., “Methadone Barriers Persist, Despite Decades of Evidence,” Health Affairs Blog , Health Affairs, Sept. 23, 2019, https://www.healthaffairs.org/do/10.1377/hblog20190920.981503/full/#_ftnref1 .
- Ohio Administrative Code, Medication Units, 5122-40-15 (2019), https://codes.ohio.gov/ohio-administrative-code/rule-5122-40-15 .
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards, https://www.ecfr.gov/cgi-bin/retrieveECFR?gp=3&SID=7282616ac574225f795d5849935efc45&ty=HTML&h=L&n=pt42.1.8&r=PART .
- University of Florida Health, “What Are the Benefits of Becoming a Consultant Pharmacist?” accessed March 21, 2022, https://cpe.pharmacy.ufl.edu/consultantpharmacist-2/what-are-the-benefits-of-becoming-a-consultant-pharmacist/ .
- J.R. Jackson et al., “Characterizing Variability in State-Level Regulations Governing Opioid Treatment Programs,” Journal of Substance Abuse Treatment 115 (2020), https://doi.org/10.1016/j.jsat.2020.108008 .
- K. Cioe et al., “A Systematic Review of Patients’ and Providers’ Perspectives of Medications for Treatment of Opioid Use Disorder,” Journal of Substance Abuse Treatment 119 (2020), https://pubmed.ncbi.nlm.nih.gov/33138929 ; H.S. Reisinger et al., “Premature Discharge From Methadone Treatment: Patient Perspectives,” Journal of Psychoactive Drugs 41, no. 3 (2009): 285-96, https://pubmed.ncbi.nlm.nih.gov/19999682 .
- A.M.W. LeBrón et al., “Restrictive ID Policies: Implications for Health Equity,” Journal of Immigrant and Minority Health 20, no. 2 (2018): 255-60, https://doi.org/10.1007/s10903-017-0579-3 .
- California Code of Regulations, Patient Identification System, 9 CSR 10240 (2021), https://www.law.cornell.edu/regulations/california/Cal-Code-Regs-Tit-9-SS-10240 .
- V. Baaklini et al., “Most States Eased Access to Opioid Use Disorder Treatment During the Pandemic” (2022), https://www.pewtrusts.org/en/research-and-analysis/articles/2022/06/01/most-states-eased-access-to-opioid-use-disorder-treatment-during-the-pandemic .
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards; Substance Abuse and Mental Health Services Administration, “Federal Guidelines for Opioid Treatment Programs” (2015), https://store.samhsa.gov/product/Federal-Guidelines-for-Opioid-Treatment-Programs/PEP15-FEDGUIDEOTP .
- Substance Abuse and Mental Health Services Administration, “Methadone Take-Home Flexibilities Extension Guidance,” last modified March 3, 2022, https://www.samhsa.gov/medication-assisted-treatment/statutes-regulations-guidelines/methadone-guidance .
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards.
- Missouri Code of Regulations, Opioid Treatment Program, 9 CSR 30-3.132 (2021), https://www.law.cornell.edu/regulations/missouri/9-CSR-30-3-132 .
- 42 C.F.R. § 8.12 Federal Opioid Treatment Standards; M. Hochheimer and G.J. Unick, “Systematic Review and Meta-Analysis of Retention in Treatment Using Medications for Opioid Use Disorder by Medication, Race/Ethnicity, and Gender in the United States,” Addictive Behaviors 124 (2022), https://www.sciencedirect.com/science/article/pii/S0306460321002987 .
- Oklahoma Code of Regulations, Service Phases - Phase VI, 450:70-6-17.8 et seq(2021), https://www.law.cornell.edu/regulations/oklahoma/Okla-Admin-CodeSS-450-70-6-17-8 (a sixth phase is also set out in regulations, but new patients have not been eligible for this phase since July 1, 2007).
- National Academies of Sciences, Engineering, and Medicine, Medications for Opioid Use Disorder Save Lives (Washington: National Academies Press, 2019).
- The Pew Charitable Trusts, “Opioid Overdose Crisis Compounded by Polysubstance Use” (2020), https://www.pewtrusts.org/en/research-and-analysis/factsheets/2020/10/opioid-overdose-crisis-compounded-by-polysubstance-use ; A.C. Stone et al., “Methadone Maintenance Treatment Among Patients Exposed to Illicit Fentanyl in Rhode Island: Safety, Dose, Retention, and Relapse at 6 Months,” Drug and Alcohol Dependence 192 (2018): 94-97, https://www.sciencedirect.com/science/article/pii/S0376871618304721 .
- Substance Abuse and Mental Health Services Administration, “Federal Guidelines for Opioid Treatment Programs”; Substance Abuse and Mental Health Services Administration, “Medications for Opioid Use Disorder: Treatment Improvement Protocol 63” (2021), https://store.samhsa.gov/sites/default/files/SAMHSA_Digital_ Download/PEP21-02-01-002.pdf; National Academies of Sciences, Medications for Opioid Use Disorder Save Lives .
- Substance Abuse and Mental Health Services Administration, “Medications for Opioid Use Disorder: Treatment Improvement Protocol 63.”
- American Society of Addiction Medicine, “National Practice Guideline for the Treatment of Opioid Use Disorder” (2020), https://sitefinitystorage.blob.core.windows.net/sitefinity-production-blobs/docs/default-source/guidelines/npg-jam-supplement.pdf?sfvrsn=a00a52c2_2 .
- F. Faggiano et al., “Methadone Maintenance at Different Dosages for Opioid Dependence,” Cochrane Database of Systematic Reviews , no. 3 (2003), https://doi.org//10.1002/14651858.CD002208 .
- Substance Abuse and Mental Health Services Administration, “Federal Guidelines for Opioid Treatment Programs”; J.A. Trafton, J. Minkel, and K. Humphreys, “Determining Effective Methadone Doses for Individual Opioid-Dependent Patients,” PLOS Medicine 3, no. 3, (2006): e80, https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.0030080 .
- Urban Survivors Union, “The Methadone Manifesto,” ( https://sway.office.com/UjvQx4ZNnXAYxhe7?ref=Link&mc_cid=9754583648&mc_eid=51fa67f051 ; G. Joseph et al., “Reimagining Patient-Centered Care in Opioid Treatment Programs: Lessons From the Bronx During COVID-19,” Journal of Substance Abuse Treatment 122 (2021), https://pubmed.ncbi.nlm.nih.gov/33353790 .
- C. Strike and C. Rufo, “Embarrassing, Degrading, or Beneficial: Patient and Staff Perspectives on Urine Drug Testing in Methadone Maintenance Treatment,” Journal of Substance Use 15, no. 5 (2010): 303-12, https://doi.org/10.3109/14659890903431603 .
- National Academies of Sciences, Medications for Opioid Use Disorder Save Lives ; American Society of Addiction Medicine, “The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder - 2020 Focused Update” (2020), https://www.asam.org/quality-care/clinical-guidelines/national-practice-guideline .
- N. Krawczyk et al., “Opioid Agonist Treatment Is Highly Protective Against Overdose Death Among a U.S. Statewide Population of Justice-Involved Adults,” The American Journal of Drug and Alcohol Abuse 47, no. 1 (2021): 117-26, https://doi.org/10.1080/00952990.2020.1828440 .
- American Association for the Treatment of Opioid Dependence, “AATOD Guidelines for Guest Medication,” http://www.aatod.org/advocacy/policy-statements/aatodguidelines-for-guest-medication/ .
- Jackson et al., “Characterizing Variability”; Prescription Drug Abuse Policy System, Requirements for Licensure and Operations of Medications for Opioid Use Disorder Treatment, through Aug. 1, 2020, https://pdaps.org/datasets/medication-assisted-treatment-licensure-and-operations-1580241579 .
- American Society of Addiction Medicine, “COVID-19 - National and State Health Guidance,” https://www.asam.org/quality-care/clinical-guidelines/covid/national-andstate-guidance .
- Jackson et al., “Characterizing Variability”; Prescription Drug Abuse Policy System, Requirements for Licensure and Operations of Medications for Opioid Use Disorder Treatment.
- Substance Abuse and Mental Health Services Administration, “State Opioid Treatment Authorities,” https://www.samhsa.gov/medication-assisted-treatment/sota .

How State Legislatures Can Pass Effective Policies on SUD
Like many parts of the country, Kentucky has experienced a devastating opioid crisis, with the second highest overdose death rate in the U.S. according to the Centers for Disease Control and Prevention.

Measure More Than Deaths to Improve Addiction Treatment
During the first 12 months of the COVID-19 pandemic, more than 70,000 people died in the U.S. from an opioid overdose.
Don’t miss our latest facts, findings, and survey results in The Rundown
ADDITIONAL RESOURCES

MORE FROM PEW

Opioid Treatment Programs: SAMHSA Makes Permanent Regulatory Flexibilities

On February 1, 2024, the Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services, announced a final rule updating the regulations regarding Opioid Treatment Programs (OTPs) as part of the Biden Administration’s Overdose Prevention Strategy. These announced changes are the first update to the OTP regulations in over 20 years and significantly increase access to medications like methadone and buprenorphine that treat opioid use disorder by, among other things, making permanent prescribing of “take-home” doses and enabling use of telemedicine to extend OTPs to a patient’s home.
What are OTPs?
OTPs provide medication assisted treatment (MAT) for people diagnosed with opioid use disorder (OUD). MAT utilizes medications (typically methadone or buprenorphine) with psychosocial counseling and other behavioral health services to treat patients. OTPs are sometimes called methadone clinics because these clinics are the only way people can access methadone treatment for opioid use disorder. OTPs may exist in a variety of settings including intensive outpatient programs, residential programs, and hospitals, but all OTPs require a specific license certification by SAMHSA, and accreditation by an independent, SAMHSA-approved accrediting body. The OTP model has been criticized as too burdensome in restricting a patient’s ability to easily access life-saving medication and treatments for OUD. The prior requirement that methadone only be prescribed at these clinics and the prior restriction on unsupervised or take-home doses of medications used to treat OUD have historically required patients to make daily visits to an OTP, even in the outpatient setting.
What did the Final Rule change?
The final rule updates OTP certificate and accreditation standards, treatment standards related to medications dispensed by an OTP and removed language regarding the DATA Waiver. The DATA Waiver requirement was removed in January 2023. SAMHSA also released a table summarizing key changes along with the rationale for these changes.
Flexibility of Methadone Medication Take-Home Doses in OTPs
In March 2020, due to the COVID-19 Pandemic, SAMHSA issued exemptions allowing OTPs to dispense up to 28 days of “take-home methadone doses for stable patients being treated for OUD and up to 14 doses of “take-home” methadone for “less stable” patients. Originally meant to reduce the risk of spreading COVID-19, OTPs and patients widely supported these changes. These flexibilities were scheduled to sunset one year past the end of the COVID-19 Public Health Emergency (PHE) (May 11, 2024) or until a final rule was published.
This final rule created a permanent option allowing take-home medication including methadone, buprenorphine, buprenorphine combination productions, and Naltrexone. First, the rule allows patients to be able to access take-home medication doses for days when the clinic is closed. Beyond those doses, the OTP practitioner may use their discretion to dispense medications to patients for OUD subject to certain maximums. Within the first 14 days of treatment, the take-home supply is limited to maximum supply of seven days’ worth of take-home medication. Between 15-30 days of treatment, the take-home supply maximum is increased to 14 days. Finally, after 31 days, the patient may have a take-home supply up to 28 days.
Flexibility to Prescribe Medication for OUD via Telehealth without an Initial In-person Physical Evaluation
In April 2020, SAMHSA implemented regulatory flexibilities to address the impact of the COVID-19 pandemic including exempting OTPs from the requirement to perform an in-person physical evaluation for patients being treated with buprenorphine in an OTP. Notably, this flexibility did not apply to methadone. On May 9, 2023, SAMHSA extended this telehealth flexibility until one year past the end of the COVID-19 PHE, or until such time that SAMHSA published a final rule.
This final rule allows an OTP practitioner to initiate treatment of methadone or buprenorphine via telehealth without an initial in-person exam. The final rule states that if certain practitioners, including the OTP physician, primary care physician, or other authorized health care professional under the supervision of program physician determines that an evaluation of the patient can be accomplished via audio visual technology, then a licensed OTP practitioner may prescribe and dispense methadone or buprenorphine to the patient. Importantly, in the rule commentary, SAMHSA notes it is not extending the use of audio-only telehealth technology to methadone because methadone holds a higher risk profile for sedation. If audio-visual technology is not available, an audio-only device may be used to prescribe methadone but only when patient is in the presence of a licensed practitioner who is registered to prescribe and dispense controlled medications. These additional requirements significantly limit the usefulness of audio-only technology for the prescription of methadone.
SAMHSA notes that this final rule does not authorize the prescription of methadone via telehealth outside the OTP context Methadone must still be prescribed and dispensed by appropriately licensed OTP practitioners. Additionally, any medication must still be dispensed to the patient under existing OTP procedures.
Admission Criteria Changes
Additionally, the final rule removed stringent admission criteria that prevented patients from initially accessing treatment. First, the final rule removed the requirement that patients have a full year history of OUD before being able to access treatment at an OTP. Second, this final rule removes the requirement that patients under the age of 18 have two unsuccessful attempts at treatment before entering treatment at an OTP.
Scope of Practice Expansion
On the federal level, the definition of practitioner was modified to include any “health care professional who is appropriately licensed by the state to prescribe and/or dispense medications for opioid use disorder.” This means, subject to state laws, many more types of non-physician practitioners such as nurse practitioners or physician assistant may prescribe or order medication. However, some states may not allow non-physician practitioners such as certified nurse-midwives, nurse practitioner, physician assistants, or pharmacists to prescribe these medications.
Impact of the Final Rule
These increased flexibilities will vastly improve patient’s access to life-saving OTP services. Specifically, the changes regarding methadone prescribing are a crucial step forward in allowing patients access to this important medication. While these changes only apply to the OTP regulatory scheme, the introduction of take-home medications, the ability to prescribe medication through telehealth, changes to admission criteria, and expanding the scope of practitioners will allow OTPs to access more patients in a field that desperately needs more providers.
Foley is here to help you address the short- and long-term impacts in the wake of regulatory changes. We have the resources to help you navigate these and other important legal considerations related to business operations and industry-specific issues. Please reach out to the authors, your Foley relationship partner, or to our Health Care Practice Group with any questions.

Alexandra B. Maulden

Kyle Y. Faget
Related insights, massachusetts health care act dies at the end of legislative session but previews sweeping changes for the health care industry, fda: the effects of loper on the regulatory agenda, substance use disorder treatment services: 2025 physician fee schedule proposed rule would expand access and medicare coverage.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock A locked padlock ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
HHS Announces Funding for Substance Use Treatment and Prevention Programs
Grants to Focus on Increasing Access to Medication-Assisted Treatment for People Battling Opioid Use Disorder
Today, the Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), is announcing two grant programs totaling $25.6 million that will expand access to medication-assisted treatment for opioid use disorder and prevent the misuse of prescription drugs. By reducing barriers to accessing the most effective, evidenced-based treatments, this funding reflects the priorities of HHS' Overdose Prevention Strategy , as well as its new initiative to strengthen the nation's mental health and crisis care systems.
"Every five minutes someone in our nation dies from an overdose," said Secretary Becerra. "This is unacceptable. At HHS, we are committed to addressing the overdose crisis, and one of the ways we're doing this is by expanding access to medication-assisted treatment and other effective, evidenced-based prevention and intervention strategies. We're also traveling the country to listen and learn about new and innovative ways HHS can support local communities in addressing mental health and substance use. Together, through our Overdose Prevention Strategy and National Tour to Strengthen Mental Health, we can change the way we address overdoses and save lives."
Last week, following President Joe Biden's State of the Union address, HHS kicked off a National Tour to Strengthen Mental Health in an effort to hear directly from Americans across the country about the challenges they're facing, and engage with local leaders to strengthen the mental health and crisis care systems in our communities. This funding announcement is part of this new initiative, which is focused on three aspects of the crisis Americans are facing: mental health, , suicide, and substance use.
"This funding will enhance efforts underway throughout our nation to get help to Americans who need it," said Miriam Delphin-Rittmon, Ph.D., HHS Assistant Secretary for Mental Health and Substance Use and the leader of SAMHSA. "Expanding access to evidence-based treatments and supports for individuals struggling with opioid use disorder has never been more critical. Strengthening the nation's prescribing guidelines to prevent misuse is equally critical."
The two grant programs are:
- The Strategic Prevention Framework for Prescription Drugs ( SPF Rx ) grant program provides funds for state agencies, territories, and tribal entities that have completed a Strategic Prevention Framework State Incentive Grant plan or a similar state plan to target prescription drug misuse. The grant program will raise awareness about the dangers of sharing medications, fake or counterfeit pills sold online, and over prescribing. The grant will fund a total of $3 million over five years for up to six grantees.
- The Medication-Assisted Treatment – Prescription Drug and Opioid Addiction ( MAT-PDOA ) grant program provides resources to help expand and enhance access to Medications for Opioid Use Disorder (MOUD). It will help increase the number of individuals with Opioid Use Disorder (OUD) receiving MOUD and decrease illicit opioid use and prescription opioid misuse. The grant will fund a total of $22.6 million over 5 years for up to 30 grantees. No less than $11 million will be awarded to Native American tribes, tribal organizations, or consortia.
Anyone seeking treatment options for substance misuse should call SAMHSA's National Helpline at 800-662-HELP (4357) or visit findtreatment.gov . Reporters with questions should email [email protected] .
More information on the National Tour to Strengthen Mental Health is available at https://HHS.gov/HHSTour .
Sign Up for Email Updates
Receive the latest updates from the Secretary, Blogs, and News Releases
Subscribe to RSS
Receive latest updates

Related News Releases
Biden-harris administration awards $45.1 million to expand mental health and substance use services across the lifespan, kids online health and safety task force announces recommendations and best practices for safe internet use, biden-harris administration launching initiative to build multi-state social worker licensure compact to increase access to mental health and substance use disorder treatment and address workforce shortages, related blog posts.

The HHS Office for Civil Rights Celebrates National Recovery Month
Media inquiries.
For general media inquiries, please contact [email protected] .
Disclaimer Policy: Links with this icon ( ) mean that you are leaving the HHS website.
- The Department of Health and Human Services (HHS) cannot guarantee the accuracy of a non-federal website.
- Linking to a non-federal website does not mean that HHS or its employees endorse the sponsors, information, or products presented on the website. HHS links outside of itself to provide you with further information.
- You will be bound by the destination website's privacy policy and/or terms of service when you follow the link.
- HHS is not responsible for Section 508 compliance (accessibility) on private websites.
For more information on HHS's web notification policies, see Website Disclaimers .
- Skip to main content
- Keyboard shortcuts for audio player
- Your Health
- Treatments & Tests
- Health Inc.
Public Health
With opioid deaths soaring, biden administration will widen access to methadone.

A liquid dose of methadone at the clinic in Rossville, Ga. The medication is only available at designated opioid treatment centers and that won't change. But more clinicians will be able to prescribe it. Kevin D. Liles/AP hide caption
A liquid dose of methadone at the clinic in Rossville, Ga. The medication is only available at designated opioid treatment centers and that won't change. But more clinicians will be able to prescribe it.
As drug deaths surged above 112,000 a year in the U.S., driven by the spread of the synthetic opioid fentanyl, addiction experts have pointed to a troubling paradox. Proven medications, including methadone, have been shown to save lives, cutting the risk of relapses and fatal overdoses by nearly 60% . Yet they are rarely prescribed.
Despite the growing risk of death, only one-in-five people experiencing opioid addiction gain access to medications. Clinicians and treatment advocates say that's due in part to the fact that methadone is heavily regulated.
Now for the first time in more than 20 years, the Biden administration is publishing new federal rules for methadone treatment aimed at widening access for more patients.
"The easier we make it for people to access the treatments they need, the more lives we can save," said HHS Deputy Secretary Andrea Palm, in a statement .
"With these announcements, we are dramatically expanding access to life-saving medications."
Under the revised rules , methadone will still only be available through a limited number of roughly 2,000 federally-approved opioid treatment programs (OTPs) nationwide.
But patients accessing those clinics will now be able to receive more take-home doses of the medication; they'll be able to receive care more frequently after a telehealth consultation; and nurse practitioners and physicians assistants working at OTPs will be able to order the medication.
The new rule also eliminates a long-standing restriction that required patients to experience opioid addiction for at least a year before receiving methadone. The new actions will take affect within six months, the government says.
In a statement, White House drug czar Dr. Rahul Gupta said the new rules "can mean the difference between life or death" for people addicted to fentanyl and other opioids.
The changes, which take effect this summer, drew praise from addiction policy experts, but some critics said they don't go far enough.
In a statement to NPR, the head of the American Society of Addiction Medicine said it should be easier for qualified doctors not employed by OTPs to dispense opioid treatment medications, including methadone.
"Now it is time for Congress to act," said Dr. Brian Hurley . "[A]llow addiction specialist physicians to prescribe methadone...that can be dispensed from a local pharmacy."
Sen. Edward Markey, a Democrat from Massachusetts, also supported the Biden administration reforms, but criticized the regulatory bottleneck requiring opioid treatment programs to distribute methadone.
"Ultimately, tethering methadone exclusively to opioid treatment programs is less about access, or health and safety, but about control, and for many investors in those programs, it is about profit," Markey said in a statement.
"The longer we leave this antiquated system in place, the more lives we lose."
The American Medical Association also supported the new rules, in part because they will liberalize access to buprenorphine, another proven opioid treatment medication.
"Prescribing buprenorphine through telehealth visits provides the opportunity to reach remote and underserved communities and patients who may be unable to travel daily to in-person appointments," said the AMA's Dr. Bobby Mukkamala in a statement.
These new rules are part of a wider strategy by the Biden administration over the last two years aimed at curbing unprecedented overdose death rates .
- opioid addiciton
- biden administration
- opioid overdose

An official website of the Department of Health & Human Services

- Search All AHRQ Sites
- Email Updates
Business Plan for Medication-Assisted Treatment
Presents a business plan for health centers and practices who treat opioid use disorder (OUD). Source Providers Clinical Support System and National Association of Community Health Centers Link https://pcssnow.org/courses/business-plan-for-medications-for-addiction-treatme… Year 2017 Format Other Terms of Use Copyrighted, freely available Topic Payment & Reimbursement Audience Medical Providers Other Team Members Use Implementation of Substance Use Treatment in Ambulatory Care Special Collection MAT Tools and Resources
What is a methadone clinic / are they free?
Medically reviewed by Carmen Pope, BPharm . Last updated on June 6, 2024.
Official answer
- A methadone clinic is a SAMHSA-certified opioid treatment program.
- There are more than 1,250 SAMHSA-certified opioid treatment programs across the U.S.
- Methadone clinics provide comprehensive rehabilitation services to assist people on the road to recovery from opioid addiction.
- Methadone clinics are the only place in the United States authorized to prescribe methadone for opioid addiction.
- Methadone clinics are not free; however, public methadone clinics are usually more affordable.
More than 2 million people in the U.S. abuse opioids and more than 90 Americans die of an opioid overdose every day.
Methadone is a long-acting synthetic opioid that may be used to treat opioid addiction and chronic pain. It helps reduce withdrawal symptoms for people who have become addicted to narcotics, such as heroin, and satisfies cravings without producing a high. It was discovered in Germany in 1937 and by the 1960s it was being used to treat heroin dependency in the U.S.
Methadone is classified as a Schedule II controlled drug and according to US law, it can only be obtained through a SAMHSA (Substance Abuse and Mental Health Services Administration)-certified opioid treatment program that is registered with the Drug Enforcement Administration (DEA). These programs may also be called methadone clinics.
Methadone clinics are medical facilities where staff members are trained specifically in the prescribing and administration of methadone. They also provide comprehensive care including counseling services and help people with rehabilitation and getting on the road to recovery. However, methadone may not be the appropriate choice for everybody and other types of addiction recovery treatments, such as Suboxone, are available that can be prescribed more freely.
There are more than 1,250 opioid treatment programs across the United States that provide services to approximately 350,000 people. More than half of those require maintenance and detoxification treatment.
- Daily dispensing of methadone is often undertaken, at least initially.
- For some people, off-site dispensing can be arranged.
- Some methadone clinics see thousands of people a day.
Methadone clinics provide a range of services, such as:
- Helping people to reduce or eliminate drug use or prevent it from happening in the first place
- Advice and preventative measures to reduce the spread of infectious diseases, such as hepatitis and HIV
- Improving the well being and quality of life of people in treatment and preventing criminal activity.
Related questions
- Which drugs cause opioid-induced constipation?
- How long does opioid withdrawal last?
- How can I get emergency methadone?
Are methadone clinics free?
There is usually a cost associated with methadone clinics.
There are two types of methadone clinics – public and private.
Although public clinics are not free, they are more affordable than private clinics; however, they usually have long waiting lists and can be overcrowded.
Private clinics cost more, but they usually have no wait lists and provide a clean and welcoming atmosphere. Some may cater to specific demographics, genders, or religion.
Most offer payment plans and other payment options for those without health insurance coverage or state or federal coverage through programs such as Medicaid.
- Methadone Drugs.com https://www.drugs.com/ppa/methadone.html
- Villa, L. Methadone and Suboxone: What’s the Difference Anyway? DrugAbuse.com https://drugabuse.com/suboxone-vs-methadone/
- Frequently Asked Questions About Methadone CRC Health
Suboxone vs methadone: What’s the difference?
Suboxone (buprenorphine and naloxone) and methadone are different medicines but are both used to help people fight opioid addiction (also called opioid use disorder, or OUD). Your first treatment after a medically-supervised opioid withdrawal (detox) is often started with either buprenorphine and naloxone or methadone. Continue reading

How to sleep while taking Cymbalta?
Not being able to sleep (also called insomnia) is one of the most common side effects reported by people taking Cymbalta. In some people, this side effect improves after a couple of weeks of taking Cymbalta, but difficulty falling asleep or staying asleep can persist in others. Here are some ways you can improve sleep while taking Cymbalta:
- Take your dose of Cymbalta in the morning. Cymbalta may be given once a day or twice a day but for those people experiencing insomnia, it should be taken just once a day in the morning
- Swallow Cymbalta capsules whole; do not crush, chew, or open up the capsules and sprinkle them on food because this may cause Cymbalta to be absorbed more quickly than intended, increasing the risk of side effects such as insomnia...
Can you take tramadol with acetaminophen, ibuprofen, or aspirin?
Yes, it is safe for most people to take tramadol with acetaminophen, ibuprofen, or aspirin if they are old enough (aspirin is not recommended for children less than 16 years and tramadol should not be taken by children under the age of 12). Continue reading
Related medical questions
- How long does methadone withdrawal last?
- Does methadone show up on a drug test?
- Is methadone an opiate blocker?
- How do Celebrex and ibuprofen compare?
- Oxycodone vs Hydrocodone - How do they compare?
- 8 Cymbalta Side Effects: Should I be Concerned?
- Can you take 800mg ibuprofen with 50mg tramadol?
- Acetaminophen vs paracetamol: What do you need to know?
- How long does oxycodone stay in your system?
- Norco vs Vicodin - How do they compare?
- What do Cymbalta brain zaps feel like?
- How long does oxycodone take to work?
- Oxycodone vs OxyContin - What's the difference?
- Vicodin vs Percocet: What's the difference?
- What are the different brands of buprenorphine?
- What are the withdrawal symptoms of oxycodone?
- Oxymorphone vs Hydromorphone - How do they compare?
- What does a pain management doctor do?
- Is Buprenex safe for humans?
- Is Buprenex the same as buprenorphine?
- Is Xtampza ER a controlled substance?
- How is RoxyBond formulated to be abuse deterrent?
- Is MorphaBond ER a controlled substance?
Drug information
- Methadone Information for Consumers
- Methadone prescribing info & package insert (for Health Professionals)
- Side Effects of Methadone (detailed)
Related support groups
- Methadone (78 questions, 2,939 members)
- Chronic Pain (287 questions, 3,325 members)
- Opiate Dependence (150 questions, 2,357 members)
- Opiate Withdrawal (59 questions, 2,346 members)
- Drug Dependence (47 questions, 539 members)
Medical Disclaimer

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.

In Crisis? Call or Text 988
Your browser is not supported
Switch to Chrome, Edge, Firefox or Safari
Page title SAMHSA Announces Funding Opportunities for Grants Addressing Substance Misuse, Substance Use Disorder Treatment on Multiple Fronts
The U.S. Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), is announcing Notices of Funding Opportunities (NOFOs) for five grant programs aimed at preventing substance misuse and treating substance use disorder (SUD) throughout the nation. The grant opportunities total about $73.4 million and align with the Biden-Harris Administration’s efforts to address the nation’s addiction and overdose crises.
Preliminary data from the U.S. Centers for Disease Control and Prevention show that 102,429 people died of a drug overdose in the 12-month period ending in July 2022. There has been a steady slowing of the rate of increase in overdose deaths for the tenth month in a row, and a decrease in 12-month rolling totals for the fifth month in a row.
According to SAMHSA’s National Survey on Drug Use and Health (NSDUH), in 2021, 46.3 million people 12 or older (or 16.5 percent of the population) met the applicable Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria for having a substance use disorder (SUD) in the past year, including 29.5 million people who were classified as having an alcohol use disorder and 24 million people who were classified as having a drug use disorder. Additionally, 9.2 million people 12 or older misused opioids in the past year. The percentage of people who were classified as having a past-year SUD, including alcohol use and/or drug use disorder, was higher among young adults ages 18 to 25, compared with adults 26 or older. In 2021, 94 percent of people 12 or older with a substance use disorder did not receive any treatment. Nearly all people with an SUD who did not get treatment at a specialty facility did not think they needed treatment.
“SAMHSA’s grant funding helps break the cycles of substance misuse that contribute to America’s addiction and overdose crises,” said Miriam E. Delphin-Rittmon, Ph.D., the HHS Assistant Secretary for Mental Health and Substance Use and the leader of SAMHSA. “These grant programs present opportunities on a range of dimensions to increase access to services and supports for families and individuals in the areas of substance use prevention and treatment.”
The five grant programs are:
- Grants to Expand Substance Use Disorder Treatment Capacity in Adult and Family Treatment Drug Courts (SAMHSA Treatment Drug Courts) – $32.4 million – This expands SUD treatment and recovery support services in existing drug courts. The program recognizes the need for treatment instead of incarceration for certain individuals who have SUDs.
- Adult Reentry Program – $13 million – This program expands SUD treatment and related recovery and reentry services to adults in the criminal justice system who have an SUD and/or co-occurring substance use and mental disorders, who are returning to their families and communities after being incarcerated in state and local facilities including prisons, jails or detention centers.
- Medication-Assisted Treatment – Prescription Drug and Opioid Addiction Grant Program (MAT-PDOA) – $18.2 million – This program provides resources to help expand or enhance access to medications for opioid use disorder (MOUD). This program will help to increase the number of people who receive MOUD for their opioid use disorders and decrease illicit opioid use and prescription opioid misuse.
- Emergency Department Alternatives to Opioids Program (ED-ALT) – $6.8 million – This program develops and implements alternatives to opioids for pain management in hospitals and emergency department settings.
- Sober Truth on Preventing Underage Drinking Act (STOP Act) Grants – $3 million – This program works to prevent and reduce alcohol use among youth and young adults ages 12-20 in communities throughout the United States. The program addresses norms regarding alcohol use by youth, reduces opportunities for underage drinking, creates changes in underage drinking enforcement efforts, addresses penalties for underage use, and reduces negative consequences associated with underage drinking (e.g., motor vehicle crashes, sexual assaults).
Anyone in the United States seeking treatment for substance use issues should call SAMHSA’s National Helpline at 800-662-HELP (4357) or visit findtreatment.gov .
If you or someone you know is struggling or in crisis, help is available. Call or text 988 or chat 988lifeline.org .
Reporters with questions should send inquiries to [email protected] .
The Substance Abuse and Mental Health Services Administration (SAMHSA) is the agency within the U.S. Department of Health and Human Services (HHS) that leads public health efforts to advance the behavioral health of the nation. SAMHSA’s mission is to lead public health and service delivery efforts that promote mental health, prevent substance misuse, and provide treatments and supports to foster recovery while ensuring equitable access and better outcomes.
Last Updated: 01/13/2023
- Open access
- Published: 14 August 2021
“It’s like ‘liquid handcuffs”: The effects of take-home dosing policies on Methadone Maintenance Treatment (MMT) patients’ lives
- David Frank ORCID: orcid.org/0000-0003-3304-3237 1 , 2 ,
- Pedro Mateu-Gelabert 3 ,
- David C. Perlman 4 ,
- Suzan M. Walters 2 , 5 ,
- Laura Curran 1 &
- Honoria Guarino 3
Harm Reduction Journal volume 18 , Article number: 88 ( 2021 ) Cite this article
81k Accesses
78 Citations
126 Altmetric
Metrics details
Methadone Maintenance Treatment (MMT) is widely recognized as one of the most effective ways of reducing risk of overdose, arrest, and transmission of blood-borne viruses like HIV and HCV among people that use opioids. Yet, MMT’s use of restrictive take-home dose policies that force most patients to attend their clinic on a daily, or near-daily, basis may be unpopular with many patients and lead to low rates of treatment uptake and retention. In response, this article examines how clinics’ take-home dosing policies have affected patients’ experiences of treatment and lives in general.
This article is based on semi-structured, qualitative interviews with a variety of stakeholders in MMT. Interviews explored: reasons for engaging with, or not engaging with MMT; how MMT is conceptualized by patients and treatment providers (e.g., as harm reduction or route to abstinence and/or recovery); experiences with MMT; perception of barriers to MMT (e.g., organizational/regulatory, social) and how MMT might be improved to support peoples’ substance use treatment needs and goals.
Nearly all of the patients with past or present MMT use were highly critical of the limited access to take-home doses and consequent need for daily or near daily clinic attendance. Participants described how the use of restrictive take-home dose policies negatively impacted their ability to meet day-to-day responsibilities and also cited the need for daily attendance as a reason for quitting or avoiding OAT. Responses also demonstrate how such policies contribute to an environment of cruelty and stigma within many clinics that exposes this already-stigmatized population to additional trauma.
Conclusions
Take-home dose policies in MMT are not working for a substantial number of patients and are reasonably seen by participants as degrading and dehumanizing. Revision of MMT regulations and policies regarding take home doses are essential to improve patient satisfaction and the quality and effectiveness of MMT as a key evidence-based treatment and harm reduction strategy.
Introduction
Methadone Maintenance Treatment (MMT) is widely recognized as one of the most effective ways of reducing risk of overdose, arrest, and transmission of blood-borne viruses like HIV and HCV among people that use opioids [ 1 , 2 , 3 , 4 ]. Yet it is unpopular among many people who use illegal opioids [ 5 , 6 ] and its effectiveness has been hindered by consistently low rates of uptake and retention [ 7 ] that prevent it from meeting its potential as a harm reduction and public health intervention [ 8 , 9 ].
Research suggests that clinic policies that provide limited access to take-home doses, and the corresponding need for patients to attend their clinic on a daily or near-daily basis, is a primary driver of patient dissatisfaction [ 10 , 11 ]. Drug user rights groups, such as the Urban Survivors Union, have also argued that the lack of access to take-home doses is unethical and cruel, and that it is only because of the powerful stigma against people who use opioids that such policies are considered acceptable [ 5 ]. Moreover, there is a strong feeling among members of such organizations, that people who are not on MMT themselves, or directly connected with someone who is, simply do not understand how disruptive and counter-productive such policies are to the lives of patients [ 5 ]. Yet, there are very little data describing the effects of take-home policies on patients’ lives, including their experiences with treatment.
Thus, it is particularly important to investigate this issue in a way that centers the voices and experiences of people who use drugs (PWUD) and people on MMT especially in light of the long history of ignoring the views of PWUD in the design of substance use treatment programs and policies [ 5 , 12 , 13 ].
To address this gap, this study used semi-structured qualitative interviews with PWUD, most of whom were either currently or previously in MMT, and with treatment providers, to examine how clinics’ take-home policies have affected patients’ experiences of treatment and lives in general. Findings suggest that the current approach that requires frequent visits to MMT clinics is impractical and counter-productive, and, as such, serves as a barrier to treatment uptake and retention. In conclusion we suggest some potential policy changes for addressing the problem.
Regulations
Federal regulations mandate that when patients begin MMT they must go to their clinic every day (or six days per week if the clinic is closed on Sundays) to ingest their daily methadone dosage under direct observation by clinic staff [ 14 ]. As patients accumulate time at the clinic and test negative for illicit opioids on screens given at least once a month they are provided “take-home doses” of methadone to be used on days when clinic attendance is not required. Although federal regulations stipulate how often and under what circumstances take-home doses can be provided, individual clinics can adopt stricter policies if they choose [ 14 ]. For example, while patients can typically earn a maximum of 14 days’ worth of take-home doses (except for the few clinics that offer “medical maintenance” which provide a maximum of 28 take-home doses), many clinics choose to offer a maximum of only one week’s supply or less and require long periods of attendance and negative drug tests results to qualify [ 11 ].
Similarly, while the Substance Abuse and Mental Health Services Administration (SAMHSA) provides treatment providers with recommendations on how to determine patient eligibility for take-home doses, clinics have wide latitude to determine which patients meet that standard. For example, some clinics will not provide any take-home doses to patients who use cannabis or drink alcohol [ 15 ]. Thus, there is substantial diversity among individual clinics in regard to how many take-home doses are allowed and under what circumstances they are provided [ 11 , 16 ].
Although there are no national data on how many patients receive take-home doses, studies have found that most patients receive very few [ 11 , 17 ]. According to a recent study on take-home dose provision, while the percent of participants receiving any take-home doses (pre-Covid-19) ranged from 56 to 82%, the majority of that group (59.8%) were only receiving 1–2 days, meaning they were required to attend their clinic for the remaining 5–6 days [ 11 ].
Studies have shown that the absence of take-home doses can be a barrier to initiating treatment and that patients are more likely to discontinue MMT when take-home doses are removed [ 18 , 19 ]. There is also no evidence that requiring daily or near-daily attendance improves patient outcomes [ 20 ].
The effects of Covid-19 on take-home doses
The emergence of the Covid-19 pandemic and associated social distancing mandates placed a newfound focus on the provision of take-home doses because of the often-crowded physical spaces at most MMT clinics. In response, SAMHSA instituted amended guidelines allowing clinics to provide a greater number of take-home doses to a greater number of patients, thereby reducing the need for daily attendance [ 21 ]. The new policy granted clinics blanket authority to provide all “stable” patients with up to 28 days of take-home medication. Patients seen as less stable, but still capable of safeguarding and handling their doses, were eligible for up to 14 days of take-home doses [ 21 ].
Recent research indicates that the increased access to take-homes was highly beneficial to most patients and that there was little evidence of diversion [ 11 , 22 ]. However, the new policies were adopted inconsistently and, in some cases, existing policies were not modified at all [ 23 ]. Nevertheless, drug user advocates see the expanded access as an opportunity for change, and have pushed to make the new standards permanent [ 24 , 25 ].
Participant recruitment and interviews
This article is based on semi-structured, qualitative interviews with members of the following groups: a) people currently on MMT ( n = 13); b) people formerly on MMT ( n = 4); c) people that use illegal opioids who have never been in Opioid Agonist Treatment (OAT) ( n = 4); d) MMT treatment providers ( n = 5); e) buprenorphine treatment providers ( n = 5); and f) people who work in government agencies that regulate MAT ( n = 5).
Participants were recruited using a combination of purposive and snowball sampling, between June and October, of 2020 in New York City [ 26 , 27 ]. Recruitment was conducted using a variety of strategies including: an advertisement placed on craigslist; flyers at clinics or harm reduction organizations; and through word-of-mouth.
The study sample was diverse in terms in age, race, socio-economic status and gender. However, since participants were sampled from the New York City area, participants experience of treatment was primarily in an urban setting. As such, most had access to MMT providers, available public transportation, and comparatively short commuting distances to clinics.
Interviews lasted between 60 and 90 min and were conducted by video. Interviews were audio recorded (and video recorded if the participant consented to this) and transcribed later. Interviews explored the following domains: participants’ substance use history; reasons for engaging with, or not engaging with, and retention within MMT; how MMT is conceptualized by patients and treatment providers (e.g., as harm reduction or as a route to abstinence and/or recovery); how MMT is practiced; experiences with MMT; perception of barriers to MMT (e.g., organizational/regulatory, social) and how MMT might be improved to better support individuals’ various substance use treatment needs and goals.
All participants’ names included in this article are pseudonyms and all participants provided informed consent to participate in this study.
Data analysis
Data was coded and analyzed by Dr. Frank using AtlasTi, version 8. Analysis was guided by a thematic approach that aimed to organize data into meaningful categories based on the aims of the study and existing literature and informed by the first author’s lived experience using illegal opioids and in MMT [ 28 ].
Dr. Frank has been on MMT for approximately 17 years and received services at two clinics: one in Chicago, IL and one in The Bronx, NY. Moreover, as he has done in previous studies, Frank regularly disclosed his status as someone with lived experience of opioid use who was currently on MMT to study participants [ 9 , 15 ]. Although he has discussed many of the methodological issues associated with this choice in other articles (see for example [ 29 ], in short, the authors believe that by disclosing Frank’s shared history, he was able to develop a level of comfort and trust with study participants that facilitated more robust and honest conversations and a richness of data that would not have been possible otherwise. There is an extensive literature describing the mistrust that PWUD often feel towards public health and substance researchers that similarly recognizes the importance of research conducted by and involving community insiders [ 30 , 31 , 32 ].
Theoretical approach
Consistent with Dr. Frank’s lived experience with opioid use and MMT, the authors used a situated theoretical approach to data collection and analysis. Situated approaches are those that acknowledge the positionality and power relationships existing between researcher, subject, and participant [ 33 , 34 , 35 ]. They are often used when studying groups that are structurally and/or ideologically marginalized, and generally place a greater emphasis on transparency and reflexivity than on neutrality and objectivity. Situated approaches are also more comfortable with the political and activist concerns of research than other methodological approaches that focus primarily on uncovering objective knowledge. In situated approaches, challenging power is seen as a valuable part of the process [ 33 , 36 ].
Patients’ experience of restricted access to take-home doses
Nearly all of the patients with past or present MMT use were highly critical of the limited access to take-home doses and consequent need for daily or near daily clinic attendance. It was by far the most commonly reported complaint from patients and former-patients. Participants often compared the restrictions to jail and/or used the pejorative that MMT was like “liquid handcuffs”. Participants’ responses also demonstrated significant anger, resentment, and a sense that their experiences were not understood by the “outside world”. For example, patients said:
I hate it [MMT] because it’s like liquid handcuffs. Say you want to go somewhere for a few days, you need take-homes and if they won’t give them to you, there’s nothing you can do. The outside world, or people that are not on MMT don’t really understand what that’s like…. Take-homes are the biggest thing [problem], everyone has trouble with them, whether it’s losing their job, or they can’t go out of town, or they’re just late, or sick. And then especially, with hurricane Sandy. Whenever there’s going to be a storm in the forecast, I specifically hide some of my pills so that I’ll have something, just in case. Samantha, female, previously on MMT
I need, I want to get off it [MMT]. It’s like being in jail. Because you have to go every goddam day. Lisa, female, currently on MMT
The only time – yeah, the only time you got a take home was something like Christmas Day and New Year’s Day. And, yeah, and other than that, you went and there was only one program and you could be three hours away on the other side of the island and it didn’t matter. Genene, female, currently on MMT
Having to be at the clinic everyday made it particularly difficult for patients to maintain steady employment, attend school, or manage their daily lives. Since most clinics have limited hours of operation, often early in the morning, it regularly impacted their ability to get to work or attend to other daily responsibilities on time. Moreover, since many participants hid their participation in MMT from employers, they often had to lie on occasions when they were late to work due to clinic attendance. That clinic policies had such a negative impact on participants’ ability to work led to strong feelings of injustice among patients and a sense that they were not being treated in a fair or decent way. For example, participants described this issue in the following ways:
So basically, the idea is to get back to living your regular life, you know? But, in a way, it kind of deters you from doing so sometimes, you know? And you know, and especially at first, I had to go even on Saturdays. I mean, how the hell would I do a regular job like that, you know? How could I get a nine to five, right? You know, I don't know that I could definitely be on time. I've seen it happen. Like, my brother for instance, I've been lucky, kinda, so far, that I've been able to try to make it work, you know? Dean, male, currently on MMT
Because when they tell you – not only that you have to go there every day, they take control of your life. You can't go on vacation, you gotta tell them when you're going, and you gotta ask permission . You know, and then you gotta explain to people why you're always late. I need to – they don't look at you good when you tell them you're on methadone program, but I have to go every day. Nina, female, previously on MMT
Like say, I have to be at work at 7 o'clock. [The] place opens at 6:30, and then by the time I get out of there, it's already 7 o'clock and I'm supposed to be at work at seven, you know. John, male currently on MMT
Thus, patients characterized the need for daily or near-daily clinic attendance as antithetical to their efforts to adopt a more stable, and in particular employed, life and to their ability to effectively manage their day-to-day responsibilities. It also adversely impacted their quality of life not only through the daily labor of clinic commutes but also through the stress and anxiety that such policies created in their lives.
Impact of MMT’s organizational structure on patients’ ability to plan for life activities
Difficulties with daily attendance were exacerbated by the often inconsistent and hard-to-plan-for organizational structure of most clinics. Patients reported that long lines, a lack of communication, and on-the-spot changes in patient requirements, meant that people could not effectively anticipate how long each visit might last. For example, patients were often informed of mandatory meetings with their counselor upon arriving at the clinic. They were rarely given information on the length of time they would have to wait or on how long their appointment was expected to last. They were also unable to postpone or re-schedule such appointments since most clinics prevented patients from dosing in such circumstances. Moreover, patients knew that leaving would likely result in disciplinary actions and would almost certainly mean the loss of any currently held take-home doses. For example, Dean, who is currently on MMT described the effects of such practices in the following way:
I've had numerous times, like, when I was going, three times a week or whatever, [and] I would have a counselor session, so now, not only am I standing on the line, and you know, getting medicated, which is gonna take 15 to 20 minutes, now I gotta stop and see the counselor, and they could be with somebody else. I mean, I've had instances when I went in and out, but I've also had instances when I go – walk in there thinking I'm gonna be out in 15 minutes, and I've been in there for freaking an hour and a half, you know? I mean, that's a big chunk of your day. How am I supposed to – you know, how am I supposed to hold down a normal job, and you know, deal with that when it's not even scheduled? You know what I'm saying? Dean, male, currently on MMT
Patients were also randomly required to make additional clinic visits, known as “callbacks” in order to prove that they had to correct amount of medication and thus, were not selling it or using it too fast. As Kathy, a 65-year-old woman on MMT described:
What they did was the call backs were five days a week you had to call a phone number at 6:00 PM. And if it was your number, the next morning you had to go there with your bottles. And it was like, you know, I was an executive for Fortune 5 Company. I work for [a well-known company] and I might find out the night before I had to be in the New York office for board meeting. And I was like, “How can I live like this?” Kathy, female, currently on MMT
Similarly, participants reported that clinics were often unwilling to provide take-home doses for life events, such as weddings, funerals, or medical emergencies. Moreover, since clinics often employed a complex and time-consuming committee structure to make such decisions, patients were unable to plan for such occurrences and many described having missed out on important family gatherings and events. For example, when asked if their clinic would provide take-home doses for an emergency, Todd said:
I don’t think so [that my clinic would give me take-homes for a family emergency], no. Because the thing is, it would have to – my counsellor would have to have a sit down with the committee, they would have to talk about it, so if it's an emergency situation, and I have to go, that timeframe is not – you know, I don’t have time for that. So, if I call them now, and I'm like, "I got a flight to Florida, I got to go in, like, a half hour," you know, I'm not going to get the take-home doses.” If something were to happen where, like, you know, my father is getting up there in age, so if, God forbid, something was to happen, and I had to [go see him], my only option is to figure out how, you know. I'm not going to get sick when I go to Florida, you know what I mean? And I think it's going to be – I don’t think I'm going to have any luck talking to them [the clinic], so the only option I'm left with is, you know, figuring out on my own devices [obtaining opioids illegally], you know what I mean? Todd, male, currently on MMT
These difficulties are often exacerbated by the expense, complexity, and limited availability of clinics that provide guest dosing to out-of-town patients as well as by the need for many patients to keep their participation in MMT a secret from family members.
As participants’ responses demonstrate, patients experience significant frustration over polices which they saw either as completely incomprehensible or as an expression of stigma and dislike of PWUD. Many expressed the view that the take-home structure made improving one’s situation while on MMT a nearly impossible task.
Moreover, as Todd described, such practices put patients in the position of having to choose between missing out on important life events, trying to attend them while in withdrawal, or obtaining opioids on the illicit market, and thus risking a future failed clinic drug screen which would then result in the removal of any take-home doses that patient was currently receiving (as well as the other risks associated with buying and using illegal opioids).
In some cases, clinicians’ treatment of patients was even cruel and dehumanizing. For example, Nina, who is no longer on MMT, described a harrowing and degrading experience in which she was made to wait in line after her water broke during pregnancy.
The last clinic, I was at, I was pregnant, and I had my water break in line, and it was a long line. I asked them to put me to the front, and they made me wait in line. I told them my water broke and they made me stay in line. Instead of medicating me, they made me stay in line with everybody. Nina, female, previously on MMT
Lack of take-home doses creates a deterrent to participation in MMT
People who had quit MMT, or who have never been on it, often described the need for daily attendance as their primary reason for avoiding or quitting treatment. They pointed out that in combination with long commuting times to the clinic, that everyday attendance is unrealistic as a workable, long-term solution. For example, one participant who said that he “would have jumped on treatment in a second” described why he chose not to in the following way:
You have to go to go there every single day and get doses, which is a complete, that’s a nightmare. That’s going to probably be the number one reason people don’t want to get on Methadone. You got to go, you have to go stand there in the morning, wait to get dosed and it just sounds like a real pain. I’d much rather see a doctor once a month, get a prescription and deal with it like that… I lived in Pennsylvania, and at the worst time, I would have jumped, I would have jumped on treatment in a second. But the closest clinic was in Lancaster and that meant that I would have to drive up there every day, which it was a little over two hours each way so, I would have to do that every day. Edward, male, never been on MMT
Others, echoing Todd’s comment that restrictive take-home policies encourage patients to continue using illegal opioids, pointed out that restrictions on MMT made it so onerous that it was easier to simply obtain opioids illegally. For example, Nina, a 63-year-old woman who had previously been on MMT explained:
That was one of the things that drove me away, that I would rather be on heroin than be on methadone. Cuz I wanted to be free to do what I want to do when I want to do it, and I – and could take them with me, and go where I want… [When I was on MMT] I was like a double slave. Like, you're a slave to the heroin already. And you're on methadone, you're a slave to the methadone and the clinic. Nina, female, previously on MMT
A financial incentive for not providing take-home doses
Patients, treatment providers and individuals from government agencies that regulate MMT all described a variety of ways that clinics were financially disincentivized from providing patients with take-home doses. For example, patients described how insurance, and the different ways that companies reimbursed clinics, affected how often they were required to come in. Patients also regularly described clinics as “businesses” and saw treatment decisions as being motivated primarily by financial rather than healthcare-related concerns. They reported the following:
This was kinda shitty. I remember I earned up to two weeks [of take-home doses], and I was self-paying, you know? And then what happened was I started working a nine to five again, and I qualified for – not Medicaid, but the, like, family health plus or something like that. So, because they [Dean’s new insurance company] paid less [than he previously paid as an out-pocket customer], they [the clinic] wanted me to now come once a week. Even though I was still just as abstinent, they wouldn't get paid as much since I wasn't self-paying anymore. So, they wanted to bill every week. And my counselor basically told me the truth. She's like, "Look, they're not gonna ok this." And I thought that was kinda fucked up, you know? You know, it's like, "Really?" You know? It's like – you know, cuz – I mean I understand that [it’s a] business, absolutely, but you know. Dean, male, currently on MMT I go once every two weeks now that's only, because of the COVID and, because of the fact that I'm on Medicaid. Medicaid—if I was on some other type of insurance, I would only have to go once a month regardless of the COVID but, because Medicaid will not pay for you to come—they won't pay the clinic the money unless you show up. Allison, female, currently on MMT But it also is a business, and so, sometimes, when you go to a counsellor, or you go to somebody from the program, I feel you kind of get a little sided – not honest – because they don’t want you to get off, they want you to keep coming, you know what I mean? It's a business before anything else. Todd, male, currently on MMT
Treatment providers and respondents who work in government organizations that administer MMT also described a structure of financial incentives linked to clinic attendance. While indicating that the logistics of clinic billing are complex and subject to differences in state and local regulations and between individual clinic policies and practices, they nevertheless described a reimbursement structure that disincentivized the provision of take-home doses. For example, they reported the following:
I'm wondering if you've looked into this – that the amount of times, the number of times people go is tied into the reimbursement that clinics get, and that alone is a big deal. I really can’t claim to understand, it is the whole billing process. [But] I think the way that programs are able to bill generally is badly set up for people who are stable and receiving 28 days delivery, but it’s something to do with paying for, you can get the money for the medication and then you get money for the counseling or the other kind of support services, that clinics have been reluctant to either increase people’s take-home doses because of a financial barrier. Dale, female, government employee I would say that they are not supported properly with the proper financial reimbursement that supports a proper successful model… So, it's not necessarily that they're incentivized to bring people in every day. It's that they're not reimbursed with a structure that allows them, that supports them financially, to give out 28 days to successful patients. So just to give you a quick idea, you get paid -- let's say it's $20 every time someone comes just for the medicine, for a medication visit, but the first visit of the week is $40, let's say. So, if you came once for 28 days and that's all you got, you would get $40 for that visit. Sofia, female, treatment provider and advocate It seems to us even in the way that OASAS [Office of Addiction Services and Supports] and other folks were describing it was the system basically is not set up well for people who are stable, because the reimbursement is less. And so, there is less incentive for any of these clinics, which are all money-making entities, to extend peoples’ take-home doses. Christine, female, government employee
Thus, despite the many variables that likely play a role in this issue, participants were confident that clinics’ take-home dose policies were directly related to an institutional reimbursement structure that incentivizes clinic attendance to generate MMT program revenue and thus disincentivizes the provision of take-home doses.
Providers’ views on take-home doses
Many treatment providers, particularly those who worked primarily with buprenorphine, agreed with patients that the current approach is impractical and poorly suited to addressing patients’ needs. For example, they stated that:
[You shouldn’t] have to go every day for however indefinite number of years to a place that's 90 miles away from your house, and you've got to ride public transportation or whatever it is. Yeah, no. Our closest methadone clinic from my office is about a half hour. From the central place for most of my patients based on where they live in the zip code. It's a two-and-a-half-hour round trip to go to a methadone clinic so you can't work, you can't have a job. You can't go to school. You get your methadone and go home. You do that every day. Yeah, the system is broken. Richard, MD, male buprenorphine provider Well, the need to be at the clinic up to six times a week is really not conducive to living a life that’s away from an environment which is going to attract drugs. There’s a certain social control component that goes into that, and even though clients might be encouraged to remain abstinent certainly they’re going to pass their fair length of drug dealers when they go to look forward to clinic. And make acquaintances of people who are at the high possibility of being active users, and also even if you want to work how do you work when you have to go to your clinic five days a week and medical six days a week. [We need more] flexible scheduling. Anthony, MD, male MMT provider
The views of clinicians provide an important point of triangulation that gives added credence to the testimony of patients, particularly since they align so closely with patients’ responses.
These findings provide an in-depth examination of the many ways that restrictive take-home dose policies negatively impact the lives of people on MMT. They describe a situation whereby the organizational approach to take-home doses almost guarantees that patients will encounter significant life disruptions that result in impediments to their ability to maintain employment, travel and respond to important life events.
Very few people in any walk of life would be able to show up to a non-work appointment at 6am every single morning and even less so when administered in the rigid, top-down and punitive manner described by patients. Indeed, it is only because the first author was able to find one of the few clinics that does offer 28 days of take-home doses, that he was able to attend graduate school and pursue a professional career. Had Dr. Frank been required to attend clinic every day, or even a few times a week, for years on end, graduate school and a career would have been entirely impossible.
By revealing how poorly people on MMT are often treated, the study findings also reveal the extent that they are marginalized. Patients’ descriptions evoke Giorgio Agamben’s socio-philosophical work on “bare life”, which highlights that certain (marginalized or oppressed) populations are seen by others as being outside of, or a “state of exception” to, the boundaries of human citizenry and thus not deserving of basic human rights [ 37 , 38 ]. Agamben developed this set of concepts to help explain how certain groups, such as prisoners in Guantanamo Bay, are treated with little regard to standards of decency. Descriptions by MMT patients of being forced to stand in line after clearly going into labor or being denied the opportunity to attend a family members’ funeral—particularly when done in the context of the biological power that clinicians wield over patients through their dependence on methadone [ 39 , 40 ]—show a particular cruelty and dismissiveness of this populations’ human rights, as though they are undeserving of the same standards of ethical humane consideration and respect that are generally and appropriately expected in patient-provider, and indeed -most, relationships.
Similarly, the literature on medicalization describes how medical personnel derive power through the socio-cultural framing of behaviors, particularly those activities seen as deviant, like substance use, as medical problems [ 41 , 42 ]. Not surprisingly, treatment providers often rely on addiction-as-disease narratives that position PWUD as inherently disordered and in need of the clinics’ firm hand, to justify such polies. Yet, Frank’s previous work has contended that this is a mischaracterization of the reasons that PWUD use and benefit from MMT. Rather he has argued that MMT is better understood as a survival strategy that PWUD use in a variety of ways to maintain their use of opioids and reduce the harms of criminalization of drug use [ 9 , 43 ]. In other words, whether patients pursue abstinence or not, MMT provides them with a shelter from harms stemming from the criminalization of drug use. Similarly, Frank & Walters have problematized the notion of consent in MMT by pointing out the ways that structural, legal, and cultural forces constrain the decisions of people who use illegal opioids [ 29 ]. In this light, restrictive take-home policies, and those who enforce them appear as yet another structural barrier preventing PWUD from obtaining safe access to opioids.
The solutions to this problem are, in many ways, not complicated. Programs must be made tolerable to patients, otherwise they will not use them. This is borne out by the consistently low rates of use and retention and correspondingly high rates of patient dropout in MMT [ 44 ]. However, since restrictions are tied to an institutional structure that disincentivizes take-home dose provision, part of the solution requires creating an institutional reimbursement system or health care delivery model that supports, and at a minimum does not structurally disincentive, increased take-home doses. Advocates from the Urban Survivors Union, a harm reduction and drug-user rights organization recently published a “Methadone Manifesto” that also recommends abandoning requirements that limit take-home dose provision to those with long records of attendance and negative drug tests, and similarly, that peoples’ take-home doses not be suspended or rescinded for positive drug screens [ 5 ].
In addition, changes should be made that allow for the provision of methadone in a manner similar to buprenorphine, another maintenance-based medication for people that use opioids. Because they are regulated differently, buprenorphine providers have far more latitude to determine the most appropriate take-home schedule for their patients and generally provide take home doses more often than MMT clinics [ 45 ]. In fact, research shows that some PWUD choose buprenorphine over MMT, despite a preference for methadone, because of the access it provides to take-home doses, and that—since buprenorphine is only a partial agonist and methadone is a full-agonist—such choices could lead to negative healthcare outcomes [ 29 ].
Opponents to providing increased access to take-home doses most often cite fears of diversion [ 46 ]. However, research suggests that this consideration is both exaggerated and mischaracterizes the complex risk environment that MMT addresses [ 47 , 48 , 49 ]. First, studies show that diversion is uncommon and happens more often among people using opioids for pain than for substance use [ 48 , 50 ]. Recent studies examining expanded access to take-home doses during Covid-19 also found that diversion was rare [ 11 , 22 ]. Second, concerns over diversion ignore the more significant risks of not providing take-home doses. As our findings demonstrate, the lack of take-home dose provision incentivizes patients to obtain opioids illegally where they will be exposed to the much greater risks associated with illegal and unregulated opioid use [ 51 , 52 , 53 ]. Restrictive take-home policies also encourage treatment discontinuation and discourage PWUD from engaging in MMT. In short, the risks of diversion, even when it happens, are far less than those produced by the current approach to MMT.
Further, the common clinic policies of using random drug testing or pill/bottle count spot checks and ‘call backs’ to assess if patients are potentially using illicit substances between visits, or potentially diverting methadone, should be reconsidered. While current US Federal guidelines require random urine checks as part of “diversion control plans [ 14 ], quantitative data to ascertain the degrees to which these practices either actually improve relevant outcomes or contribute to non-retention in treatment are scarce [ 54 ]. Our data demonstrate the extent to which these practices function as ‘part of the handcuffs’ and serve as barriers to job attendance and other social responsibilities. Further data to assess the holistic outcomes of random callbacks and spot checks are needed to soundly inform the design of truly evidence based, effective and humane, clinic policies.
Individual clinics can also make changes that would help to improve the burden on patients. For example, using a better organizational approach to scheduling patient appointments would improve many of the difficulties patients face. Similarly, clinicians can be more respectful of patients’ time commitments and outside-of-the-clinic responsibilities, and avoid using punishment, or the threat of punishment, as a response to scheduling issues.
Finally, there is a need for more detailed, publicly-available information on MMT clinics’ take-home dose policies and practices. SAMHSA should collect clinic-level data on how many patients receive take-home doses and according to what schedules. Similarly, clinic level data on individual clinics’ take-home policies, such as the maximum amount of take-home available and what kinds of metrics are used to ascertain whether a patient qualifies for addition take-homes, should also be made more readily available. This would help researchers and policymakers to develop a clearer picture of take-home provision and better determine which policies are working and which are not.
This paper has relevant limitations. It is based on a relatively small sample size. Similarly, and as with all qualitative research, results can not necessarily be generalized to the larger population of people on MMT. Additionally, as noted in the Methods section, it utilized an insider’s perspective which informed the data collection and analysis. Lastly, we would have liked to include demographic information about participants’ race and age in the interview quotations and explored its role in this issue. However, partly because of data collection difficulties that arose as a result of COVID-19, we were unable to collect this information for all of the participants and thus, decided to not include it for any of the quotations.
In conclusion, these data clearly demonstrate that take-home dose policies in MMT are not working for a substantial number of patients, are reasonably seen by participants as degrading and dehumanizing, and directly contribute to both non-engagement in MMT, MMT non-retention, and to significant difficulties with patients’ employment and in their lives. MMT’s many benefits are well known and supported by decades of evidence, and recognized by many PWUD ( 55 ). Yet, if MMT is made so onerous, degrading, and difficult that patients conclude that they cannot remain, or that it is not worth remaining, in treatment and live a ‘regular’ stable, fulfilling life, then they will not. Rather, and has been seen for decades, they will continue to simply ‘remove their liquid handcuffs’ and disengage from MMT, and return to obtaining opioids solely through the riskier illegal market. Revision of MMT regulations and policies regarding take home doses, drug testing and pill/bottle counts, and general operations are essential to improve patient satisfaction and the quality and effectiveness of MMT as a key evidence-based treatment and harm reduction.
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available due to privacy concerns but are available (in a de-identified format) from the corresponding author on reasonable request.
Sordo L, Barrio G, Bravo MJ, Indave BI, Degenhardt L, Wiessing L, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. bmj. 2017;357.
Karki P, Shrestha R, Huedo-Medina TB, Copenhaver M. The impact of methadone maintenance treatment on HIV risk behaviors among high-risk injection drug users: a systematic review. Evid Based Med Public Health. 2016;2.
Schwartz RP, Gryczynski J, O’grady KE, Sharfstein JM, Warren G, Olsen Y, et al. Opioid agonist treatments and heroin overdose deaths in Baltimore, Maryland, 1995–2009. Am J Public Health. 2013;103(5):917–22.
Degenhardt L, Randall D, Hall W, Law M, Butler T, Burns L. Mortality among clients of a state-wide opioid pharmacotherapy program over 20 years: risk factors and lives saved. Drug Alcohol Depend. 2009;105(1–2):9–15.
Article Google Scholar
Union US. The methadone manifesto. Urban Survivors Union; 2021.
Redmond H. The methadone manifesto: a powerful blow against the clinic system. Filter Magazine. 2021.
Substance Abuse and Mental Health Services Administration CfBHSaQ, Rockville, MD. Treatment Episode Data Set (TEDS): 2017. Admissions to and Discharges from Publicly-Funded Substance Use Treatment. 2019.
Saloner B, Karthikeyan S. Changes in substance abuse treatment use among individuals with opioid use disorders in the United States, 2004–2013. JAMA. 2015;314(14):1515–7.
Frank D. “I was not sick and I didn’t need to recover”: Methadone Maintenance Treatment (MMT) as a refuge from criminalization. Subst Use Misuse. 2018;53(2):311–22.
Peles E, Schreiber S, Sason A, Adelson M. Earning, “take-home” privileges and long-term outcome in a methadone maintenance treatment program. J Addict Med. 2011;5(2):92–8.
Figgatt MC, Salazar Z, Day E, Vincent L, Dasgupta N. Take-home dosing experiences among persons receiving methadone maintenance treatment during COVID-19. J Substance Abuse Treat. 2021;123:108276.
Cheng R, Smith C. Engaging people with lived experience for better health outcomes: collaboration with mental health and addiction service users in research, policy, and treatment. Toronto: Ontario Ministry of Health and Long-Term Care; 2009.
Google Scholar
Eddie D, Hoffman L, Vilsaint C, Abry A, Bergman B, Hoeppner B, et al. Lived experience in new models of care for substance use disorder: a systematic review of peer recovery support services and recovery coaching. Front Psychol. 2019;10:1052.
Substance Abuse and Mental Health Services Administration CfBHSaQ, Rockville, MD. Federal Guidelines for Opioid Treatment Programs. 2015.
Frank D. We’re gonna be addressing your pepsi use. J Extreme Anthropol. 2019;3(2):1–20.
Walley AY, Cheng DM, Pierce CE, Chen C, Filippell T, Samet JH, et al. Methadone dose, take home status and hospital admission among Methadone Maintenance patients. J Addict Med. 2012;6(3):186.
Article CAS Google Scholar
Hatch-Maillette MA, Peavy KM, Tsui JI, Banta-Green CJ, Woolworth S, Grekin P. Re-thinking patient stability for methadone in opioid treatment programs during a global pandemic: Provider perspectives. J Substance Abuse Treat. 2021;124:108223.
Pani PP, Pirastu R, Ricci A, Gessa GL. Prohibition of take-home dosages: negative consequences on methadone maintenance treatment. Drug Alcohol Depend. 1996;41(1):81–4.
Pani PP, Pirastu R. Take-home and compliance with methadone maintenance treatment. Heroin Addict Relat Clin Probl. 2000;2(1):33–8.
Amiri S, Lutz R, Socías ME, McDonell MG, Roll JM, Amram O. Increased distance was associated with lower daily attendance to an opioid treatment program in Spokane County Washington. J Subst Abuse Treat. 2018;93:26–30.
Substance Abuse and Mental Health Services Administration CfBHSaQ, Rockville, MD. Opioid Treatment Program (OTP) guidance. In: Health Do, editor. 2020.
Brothers S, Viera A, Heimer R. Changes in methadone program practices and fatal methadone overdose rates in Connecticut during COVID-19. J Substance Abuse Treat. 2021:108449.
Peavy KM, Darnton J, Grekin P, Russo M, Green CJB, Merrill JO, et al. Rapid implementation of service delivery changes to mitigate COVID-19 and maintain access to methadone among persons with and at high-risk for HIV in an opioid treatment program. AIDS Behav. 2020;24(9):2469–72.
Samuels EA, Clark SA, Wunsch C, Keeler LAJ, Reddy N, Vanjani R, et al. Innovation during COVID-19: improving addiction treatment access. J Addict Med. 2020.
Krawczyk N, Fingerhood MI, Agus D. Lessons from COVID 19: are we finally ready to make opioid treatment accessible? J Substance Abuse Treat. 2020;117.
Etikan I, Musa SA, Alkassim RS. Comparison of convenience sampling and purposive sampling. Am J Theor Appl Stat. 2016;5(1):1–4.
Butler AE, Copnell B, Hall H. The development of theoretical sampling in practice. Collegian. 2018;25(5):561–6.
Gibbs GR. Thematic coding and categorizing. Analyzing Qual Data. 2007;703:38–56.
Frank D, Walters SM. “I’m going to stop myself before someone stops me”: complicating narratives of volitional substance use treatment. Front Sociol. 2021;6:6.
Fisher CB, Oransky M, Mahadevan M, Singer M, Mirhej G, Hodge D. Marginalized populations and drug addiction research: realism, mistrust, and misconception. IRB. 2008;30(3):1.
PubMed PubMed Central Google Scholar
Jaiswal J, Halkitis PN. Towards a more inclusive and dynamic understanding of medical mistrust informed by science. Behav Med. 2019;45(2):79–85.
Souleymanov R, Kuzmanović D, Marshall Z, Scheim AI, Mikiki M, Worthington C, et al. The ethics of community-based research with people who use drugs: results of a scoping review. BMC Med Ethics. 2016;17(1):1–13.
Naples NA. Feminism and method: Ethnography, discourse analysis, and activist research: Psychology Press; 2003.
Moradi B, Grzanka PR. Using intersectionality responsibly: Toward critical epistemology, structural analysis, and social justice activism. J Couns Psychol. 2017;64(5):500.
Graham LJ, editor Discourse analysis and the critical use of Foucault. The Australian Association of Research in Education Annual Conference; 2005.
DeVault ML. Talking back to sociology: distinctive contributions of feminist methodology. Ann Rev Sociol. 1996;22(1):29–50.
Agamben G. I. HOMO SACER: Sovereign power and bare life. Stanford University Press; 2020.
Agamben G. State of exception. Nova srpska politička misao. 2005;12(01+ 04):135–45.
Bourgois P. Disciplining addictions: the bio-politics of methadone and heroin in the United States. Cult Med Psychiatry. 2000;24(2):165–95.
Keane H. Foucault on methadone: beyond biopower. Int J Drug Policy. 2009;20(5):450–2.
Conrad P. Medicalization and social control. Ann Rev Sociol. 1992;18(1):209–32.
Conrad P. The discovery of hyperkinesis: notes on the medicalization of deviant behavior. Soc Probl. 1975;23(1):12–21.
Frank D. Methadone maintenance treatment is swapping one drug for another, and that’s why it works: Towards a treatment-based critique of the war on drugs. International Journal of Drug Policy. 2020;83:102844.
Substance Abuse and Mental Health Services Administration CfBHSaQ, Rockville, MD. Treatment Episode Data Set. 2014.
Gryczynski J, Jaffe JH, Schwartz RP, Dušek KA, Gugsa N, Monroe CL, et al. Patient perspectives on choosing buprenorphine over methadone in an urban, equal-access system. Am J Addict. 2013;22(3):285–91.
Saxon AJ, Calsyn DA, Wells EA, Stanton VV. The use of urine toxicology to enhance patient control of take-home doses in methadone maintenance: effects on reducing illicit drug use. Addict Res. 1998;6(3):203–14.
Harris M, Rhodes T. Methadone diversion as a protective strategy: the harm reduction potential of ‘generous constraints.’ Int J Drug Policy. 2013;24(6):e43–50.
Cicero TJ, Inciardi JA. Diversion and abuse of methadone prescribed for pain management. JAMA. 2005;293(3):293–8.
Rettig RA, Yarmolinsky A. Methadone diversion control. Federal Regulation of Methadone Treatment. National Academies Press (US); 1995.
Jones CM, Baldwin GT, Manocchio T, White JO, Mack KA. Trends in methadone distribution for pain treatment, methadone diversion, and overdose deaths—United States, 2002–2014. Morb Mortal Wkly Rep. 2016;65(26):667–71.
Latkin CA, Dayton L, Davey-Rothwell MA, Tobin KE. Fentanyl and drug overdose: perceptions of fentanyl risk, overdose risk behaviors, and opportunities for intervention among people who use opioids in Baltimore, USA. Subst Use Misuse. 2019;54(6):998–1006.
O’Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths involving fentanyl, fentanyl analogs, and U-47700—10 states, July–December 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1197.
Daniulaityte R, Juhascik MP, Strayer KE, Sizemore IE, Harshbarger KE, Antonides HM, et al. Overdose deaths related to fentanyl and its analogs—Ohio, January–February 2017. MMWR Morb Mortal Wkly Rep. 2017;66(34):904.
Blum K, Han D, Femino J, Smith DE, Saunders S, Simpatico T, et al. Systematic evaluation of “compliance” to prescribed treatment medications and “abstinence” from psychoactive drug abuse in chemical dependence programs: data from the comprehensive analysis of reported drugs. PLoS ONE. 2014;9(9):e104275.
Joseph H, Stancliff S, Langrod J. Methadone maintenance treatment (MMT): a review of historical and clinical issues. Mt Sinai J Med New York. 2000;67(5–6):347–64.
CAS Google Scholar
Download references
Acknowledgements
Not applicable.
David Frank and Suzan Walters were supported as postdoctoral fellows and Laura Curran was supported as a predoctoral fellow in the Behavioral Sciences Training in Drug Abuse Research program supported by Grant No. #5T32 DA007233-35 from the National Institute on Drug Abuse and sponsored by New York University. Drs. Frank and Walters were also supported by the Center for Drug Use and HIV Research, NYU School of Global Public Health (NOH P30 DA011041); and Dr. Frank was supported by the Center for Opioid Epidemiology & Policy, NYU Langone Health. Dr. Mateu-Gelabert was supported by NIDA Grants: R01DA041298 and R01DA041501.
Author information
Authors and affiliations.
Behavioral Science Training in Drug Abuse Research, NYU Rory Meyers College of Nursing, 380 2nd Avenue, Suite 306, New York City, NY, 10010, USA
David Frank & Laura Curran
Center for Drug Use and HIV/HCV Research, NYU School of Global Public Health, New York City, NY, USA
David Frank & Suzan M. Walters
Graduate School of Public Health and Health Policy, City University of New York, New York City, NY, USA
Pedro Mateu-Gelabert & Honoria Guarino
Icahn School of Medicine at Mount Sinai, New York, NY, USA
David C. Perlman
School of Global Public Health, New York University, New York City, NY, USA
Suzan M. Walters
You can also search for this author in PubMed Google Scholar
Contributions
DF conducted approximately ¾ of the interviews and did most of the analysis as well as writing the majority of the article. PM helped with the analysis and editing of the paper. DP helped with the analysis and editing of the paper. SW helped with the analysis and editing of the paper. LC conducted ¼ of the interviews and helped with editing the paper. HG helped with the analysis and editing of the paper. All authors read and approved the final manuscript.
Corresponding author
Correspondence to David Frank .
Ethics declarations
Ethics approval and consent to participate.
This study was reviewed and approved by The New York University Institutional Review Board. All participants provided informed consent to participate in this study.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/ . The Creative Commons Public Domain Dedication waiver ( http://creativecommons.org/publicdomain/zero/1.0/ ) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
Reprints and permissions
About this article
Cite this article.
Frank, D., Mateu-Gelabert, P., Perlman, D.C. et al. “It’s like ‘liquid handcuffs”: The effects of take-home dosing policies on Methadone Maintenance Treatment (MMT) patients’ lives. Harm Reduct J 18 , 88 (2021). https://doi.org/10.1186/s12954-021-00535-y
Download citation
Received : 29 June 2021
Accepted : 08 August 2021
Published : 14 August 2021
DOI : https://doi.org/10.1186/s12954-021-00535-y
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Methadone Maintenance Treatment (MMT)
- Take-home doses
- Methadone clinics
- Harm reduction
- Patients’ rights
Harm Reduction Journal
ISSN: 1477-7517
- Submission enquiries: [email protected]
- Health Tech
- Health Insurance
- Medical Devices
- Gene Therapy
- Neuroscience
- H5N1 Bird Flu
- Health Disparities
- Infectious Disease
- Mental Health
- Cardiovascular Disease
- Chronic Disease
- Alzheimer's
- Coercive Care
- The Obesity Revolution
- The War on Recovery
- Adam Feuerstein
- Matthew Herper
- Jennifer Adaeze Okwerekwu
- Ed Silverman
- CRISPR Tracker
- Breakthrough Device Tracker
- Generative AI Tracker
- Obesity Drug Tracker
- 2024 STAT Summit
- All Summits
- STATUS List
- STAT Madness
- STAT Brand Studio
Don't miss out
Subscribe to STAT+ today, for the best life sciences journalism in the industry
Under new rules, methadone clinics can offer more take-home doses. Will they?
By Andrew Joseph Dec. 22, 2022

D anielle Russell is, as she says, a “poster child” for methadone. For more than a decade, the medication — one of the most effective treatments for opioid addiction — has helped her move past the heroin she used to use. She finished a series of degrees, and is now a Ph.D. student in justice studies at Arizona State University.
As life-changing as methadone is, the catch is that taking the tightly regulated medication requires reporting to a special clinic nearly every day to get one’s dose. When the Covid-19 pandemic arrived, that changed. In an effort to reduce contact among people at clinics, federal health officials said that providers could give up to 14 days of take-home doses to patients broadly, and up to 28 days to “stable” patients — patients, Russell thought, like her.
advertisement
Russell, who had been going to her Phoenix clinic six days a week prior to Covid, did get an increase in her take-home allowance, but nowhere near 28 days. Instead, the clinic allowed her to come in three days a week, she said, giving her one extra take-home dose with each visit and still requiring her to make multiple trips a week to a crowded building during the height of the pandemic.
“It was pretty bleak how clear it was how little they cared about us,” Russell said.
Related: In Philadelphia, ‘tranq’ is leaving drug users with horrific wounds. Other communities are bracing for the same
Russell was not alone. While many of the country’s 1,900 methadone clinics — called opioid treatment programs, or OTPs — extended some take-home flexibility, particularly early in the pandemic, a fraction of patients got the full weeks of take-home doses that the government enabled clinics to offer, according to studies and interviews with patients, advocates, and researchers. Some clinics, sometimes required by more stringent state rules, have since rolled back the flexibility they did provide.
The tension between looser rules on paper and the resistance among some clinics and states to take-home methadone will only intensify. Last week, the Substance Abuse and Mental Health Services Administration announced it was moving to make the pandemic-era flexibilities permanent, pointing to evidence that expanded take-homes improved patients’ quality of life and didn’t introduce new harms . Experts and advocates have largely celebrated the move. But they also wonder how widely states and individual clinics — which have great autonomy in offering patients take-home doses, and rescinding them — will adopt the changes even with a permanent policy.
“Even though they were given those flexibilities, many didn’t enact those flexibilities” during the pandemic, said Ximena Levander, an addiction medicine physician at Oregon Health & Science University, who has surveyed clinics and patients about take-home policies. “So how much is this going to help?”
How widely clinics will start providing their patients with more doses of methadone is “the million dollar question,” said Erin Madden, a health services researcher at Wayne State University, who has studied the uneasiness of providers to loosen methadone rules. Expanding treatment options as widely as possible is crucial, she and other experts say: 107,000 people died of overdoses in 2021 , largely as a result of opioids.
OTPs have historically defended the system by arguing that addiction treatment requires the expert and comprehensive care they provide, and that a structured routine can help people avoid illicit drugs. But notably, the industry group that represents most OTPs, the American Association for the Treatment of Opioid Dependence, has endorsed SAMHSA’s move, with its president, Mark Parrino, calling it a step that is “enlightened and will move the field forward.”
Related: Top U.S. addiction researcher calls for broad deregulation of methadone
Parrino noted that the policy gives providers the discretion to offer more take-homes. He said providers still have to consider the patients they’re treating and the risk that patients could misuse methadone, which is an opioid itself.
“These are opportunities,” Parrino said. “It is the clinicians and the programs that make the decisions.”
Yngvild Olsen, who leads SAMHSA’s Center for Substance Abuse Treatment, said the agency was focused on finalizing the more flexible policy, and didn’t address questions about whether or how the government would try to get clinics to expand take-homes. But she said that such a substantial shift in methadone rules could itself serve as a motivation to broaden access, and that the experience of take-homes during the pandemic demonstrated the benefits of such a policy.
“This is the first major proposed change to these regulations that has happened in 20 years,” Olsen told STAT.
In Arizona, when Russell found out she wouldn’t be getting the take-home doses she thought she should, and after hearing similar stories, she set out to document what was going on. She and colleagues launched a project that involved interviewing Arizonans on methadone — as well as another medication for opioid use disorder, buprenorphine — about any changes to medication access they saw during the pandemic. As they reported in October, not one person interviewed got a full two weeks of take-home methadone doses, let alone four weeks. Forty percent of patients had to keep going to the clinic every day.

T he OTP system dates back five decades, a structure that advocates and many experts have long criticized as paternalistic and burdensome. They say that the hoops patients have to jump through for a medication that’s been proven to tame cravings and reduce deaths pushes some off the treatment, because they don’t want to or simply can’t get to the clinic every day. Experts also note that Black patients are more likely to be routed to methadone clinics, while white patients are more likely to be prescribed buprenorphine, which is not as tightly controlled — a dynamic at play in the growing racial disparities in overdose deaths.
A burgeoning movement has called for making methadone available at pharmacies with a prescription, a policy in other countries like Canada and Australia. Supporters point to the fact that only 400,000 of the millions of Americans with opioid use disorder are on methadone as a sign that the barriers keep people off treatment. Mandating treatment at opioid treatment programs also creates geographic obstacles. A quarter of the U.S. population doesn’t have an OTP in their county. Wyoming has none.
Many OTPs have resisted relaxing the regulations . They note that as an opioid, methadone poses a risk of diversion — that people will sell their doses — and of overdose, and thus warrants supervision and specialized care. OTPs are also equipped to provide additional services like counseling.
The pandemic-inspired flexibility seemed like an intermediate step at loosening the methadone rules. Before Covid, patients could get take-homes, but they had to earn them by adhering to clinic rules and making months of daily trips before becoming eligible. But in March 2020, the government issued its blanket take-home policy, with patients able to get several weeks of doses depending on how “stable” their providers assessed them to be . If a state accepted the new policy, clinics there could offer more take-homes.
The policy was met with enthusiasm. All but seven states allowed clinics to follow SAMHSA’s new flexibility, according to Olsen. A survey of 142 OTPs in June 2020 found that 127 of them had increased take-home doses — though not always to the full extent the rules allowed.
Sign up for Daily Recap
A roundup of STAT's top stories of the day.
Surveys of patients found that the take-homes helped them lead more normal lives, with time for work and family. While some value the structure of daily clinic visits, many said the take-homes made them feel like they were taking a regular medication, no longer penalized for their past drug use.
“I don’t have to stop what I am doing to come in to dose. And it also helps me with my recovery just to get these benefits of take-homes…It makes me feel proud of myself,” one patient reported . Another patient said, “When you get your take-homes it’s like you feel you are being trusted to take care of yourself, and do the right thing.”
Getting a week’s worth of take-home doses was “huge” for Irene Garnett, a Phoenix woman who’s been on methadone for a decade. Some periods during the pandemic, Garnett didn’t have access to a car, and bus service was rolled back, so it was a relief not to have to make daily trips.
But Garnett wondered if getting even a week of take-homes made her an exception. She is involved with a local drug policy advocacy board, and helped conduct the interviews for the paper on which she and Russell were co-authors. Other patients barely had any increase in take-homes, perhaps a day or two of extra doses.
“The inconsistency with which these policies were implemented was really frustrating,” Garnett said.
Months into the pandemic, some clinics started to reimpose normal rules, researchers say. Some patients reported that their clinics returned to in-person dosing as early as summer 2020. By summer 2021, at least five states that allowed for expanded take-homes had already rescinded the policy, and three others said they planned to rescind the policy before the end of the pandemic, according to a Pew Charitable Trusts survey . Many states, however, said they intended to keep the policy as long as the federal government would allow.
Related: ‘This program’s really saved us’: As Canada offers safer opioids to curb overdoses, will U.S. follow?
The results from the pandemic-era methadone experiment have been positive. Not only did it improve quality of life, but a recent study found that patients who got more take-homes were more likely to remain on treatment and were less likely to use illicit opioids. Diversion was rare, researchers found . Moreover, a study found that methadone-involved overdoses remained stable, suggesting that expanding take-homes will not exacerbate the overdose crisis, which is largely driven by illicit fentanyl.
The flexibilities allowed not only for patients and OTP staff to stay safe from Covid, “but have also very much supported people’s ongoing recovery — their ability to be employed, go to work, take care of their families, really practice the recovery they’re engaged in,” said SAMHSA’s Olsen. She described making the flexibility permanent as a shift from “a very rule-based” system, to one based on a provider’s decisions for individual patients.
So why didn’t more clinics offer more take-homes? It could be that providers simply didn’t see many patients qualifying as “stable” according to SAMHSA’s definition , which included factors such as how long patients had been on methadone, how well they adhered to clinic rules, and whether providers thought they could store their take-home doses. Perhaps some clinics didn’t want to extend take-homes under a temporary policy, and will become more open when the flexibility becomes permanent.
Critics of the system also argue that clinics have a financial incentive to maintain the status quo. They can bill insurance or charge patients (many clinics take cash) for more services, from drug tests to counseling sessions, when people come in more frequently. Giving patients more take-homes could amount to lost revenue, at a time when for-profit organizations have been growing their footprint in addiction treatment services.
AATOD’s Parrino called such criticisms “disingenuous.” He said that clinics provide services in the best interest of patients. He also noted that providers have to consider their legal and licensing liability if the medication they prescribe isn’t taken on-site and is misused.
Still, in supporting making permanent the take-home rules, Parrino noted that the flexibility during the pandemic resulted in better retention rates. AATOD has also called on states to align their policies — some of which are stricter than federal rules — with SAMHSA’s regulations.
“It’s wise to give greater clinical flexibility to the clinicians in the OTPs,” he said.
Advocates and experts stress that they support SAMHSA’s move to make the pandemic-era policies permanent , which would also allow patients to start methadone faster and ease access to buprenorphine. They also agree that providers should have discretion in treating their patients.
But they worry that clinics will be slow to offer more take-homes, at a time when they argue that the benefits of widening access to take-home doses for many patients far outweigh the risks. Many OTPs have long histories of enforcing strict rules, sometimes cutting patients off if they don’t remain abstinent, for example, and may not feel a need to change their programs.
“Whether or not the rule is on the books, you’re going to see a lot of” clinics not offering more take-homes, said Noa Krawczyk, a substance use epidemiologist at New York University’s Center for Opioid Epidemiology and Policy. “If you’re the only OTP for 100 miles, you can do whatever you want. Patients are dependent on methadone, and they don’t have another choice.”

F or her part, Russell eventually got a month’s worth of take-home doses, after her OTP changed owners. She went from weekly drug tests to monthly.
No longer needing to go to the clinic so often, Russell had more time to devote to school and research, she said. She traveled internationally, including to Australia, where she saw a friend pick up methadone at a pharmacy.
She said she hadn’t realized how limiting the visits to the clinic were until she stopped having to make them.
“It was life-changing,” Russell said. “I knew I hated going in that frequently, but because I had been doing it for so long, I just did it. When it changed, I had all that time back in my life. I felt like a normal person.”
To find treatment options for substance use disorders, visit findtreatment.gov or call 800-662-HELP (4357).
This story is part of a series on addiction in 2022, supported by a grant from the National Institute of Health Care Management. Previous articles covered the spike in overdose deaths among Black Americans, the Americans with Disabilities Act’s protection of people with addiction histories, the debate about “safer supply” programs, and the rise of the tranquilizer xylazine in the drug supply.
Get a roundup of health and medicine news every weekday with STAT’s free newsletter Morning Rounds. Sign up here.
About the Author Reprints
Andrew joseph.
Europe Correspondent
Andrew Joseph covers health, medicine, and the biopharma industry in Europe.
public health
STAT encourages you to share your voice. We welcome your commentary, criticism, and expertise on our subscriber-only platform, STAT+ Connect
To submit a correction request, please visit our Contact Us page .

Recommended

Recommended Stories

STAT Plus: ‘Jerking families around’: Canceled Roche rare disease trial devastates parents, angers researchers

Congress is unprepared for the post-Chevron world. It needs help from subject matter experts

STAT Plus: Health Care's Colossus: How UnitedHealth harnesses its physician empire to squeeze profits out of patients

Mount Sinai mounted aggressive campaign to stifle debate over revelations about its controversial brain research

STAT Plus: Sarepta demanded Duchenne patient advocacy group censor video critical of the company
Health equity news from Boston Medical Center
Mental Health & Addiction
BMC Bridge Clinic Charts a Needed Path to Methadone for Opioid Withdrawal

Faster Paths is showing that accessible methadone treatment is a needed service for patients seeking ongoing care for opioid use disorder.
At Faster Paths, a bridge clinic for substance use disorder at Boston Medical Center, the demand for methadone treatment last year came quickly and entirely through word of mouth.
“Once we started, demand skyrocketed,” says Jessica Taylor, MD , medical director of Faster Paths . “I remember coming in the second week after the official launch, and there was a queue at the door in the morning.”
Last spring, the low-barrier clinic, which offers urgent, transitional care for substance use disorders, launched a new clinical pathway. According to a case study published in Addiction Science & Clinical Practice , Faster Paths may be the first bridge clinic to offer methadone for emergency opioid withdrawal management while referring patients to ongoing care.
Methadone, an opioid agonist, is a first-line treatment for opioid use disorder. Taylor calls it a life-saving treatment for a life-threatening illness. The National Academies of Sciences, Engineering, and Medicine agrees. In the U.S., however, methadone is highly stigmatized , and federal regulations restrict its use for outpatient treatment to licensed opioid treatment programs. At these methadone clinics, as they’re commonly called, patients can often face long wait times and logistical hurdles to starting treatment.
“What we’re seeing is that methadone is more important than ever now, because of the influx of fentanyl into the opioid supply.” Click To Tweet
There are cases, though, when methadone can be used as an emergency treatment for outpatients. These cases use what’s known in f ederal regulations as the 72-hour rule , or three-day rule. It allows providers who do not work at a methadone clinic to administer methadone in person to relieve acute withdrawal symptoms for up to three days while linking the patient to ongoing care, (such as at a methadone clinic).
Bridge clinics offer on-demand opioid treatment
Bridge clinics are relatively new as a service model for substance use disorders. They offer a safe space for patients to work toward their goals, prioritizing patient input and harm reduction. Formed in response to the opioid overdose crisis, bridge clinics make it easier for patients to be treated without delay, providing walk-in, on-demand access to medication treatment. They are often set-up within or in coordination with emergency departments or existing programs that provide medication for opioid use disorder.
Typically, that medication is buprenorphine or naltrexone, two of three FDA-approved drugs for opioid use disorder. The third, methadone, cannot be prescribed and is, by and large, limited to licensed treatment facilities.
“Unfortunately, due to concerns about methadone’s more complicated metabolism, it is typically only accessible through programs that are separate from the rest of healthcare and face more onerous regulations,” says Alexander Walley, MD , MSc, director of BMC’s Grayken Addiction Medicine fellowship and medical director of Massachusetts’s Department of Public Health’s Opioid Overdose Prevention Programs and the Bureau of Substance Addiction Services.
“This metabolism does need to be respected. Yet in the hands of an experienced, trained provider, it’s as safe as any medication.”
The 72-hour rule, not just for the emergency department
To date, using methadone to treat opioid withdrawal under the 72-hour rule has mostly been done in emergency departments, often during times of weather emergencies or natural disasters, when methadone clinics are closed or patients have trouble reaching a clinic, says Walley.
Among outpatient providers, Taylor thinks it’s a widely held belief that the rule can only be used in the emergency department. The idea for applying the 72-hour rule at Faster Paths was born out of frustration and urgency that the demand for methadone wasn’t being met.
Providing addiction support to people with COVID-19 who were experiencing homelessness further motivated the team to find a new treatment pathway.
“Many guests had opioid withdrawal and wanted to initiate methadone. But their COVID-positive status was an added barrier to the already significant challenge of starting methadone through standard outpatient pathways,” says Taylor. “We learned that we needed better ways to rapidly deliver methadone for opioid withdrawal to outpatients who wanted to be connected to long-term care.”
When the team reviewed regulations with the hospital’s legal counsel, they realized that nothing in the rules limits the location of 72-hour rule methadone administration to an emergency department. What’s more, because it’s based in a hospital, Faster Paths had a lot of the infrastructure, support, regulatory benefits, and relationships with local methadone clinics to quickly get a pathway like this off the ground.
In March of 2021, Faster Paths treated its first patient with methadone under the 72-hour rule. Two months later, with clinical protocols and partner agreements in place, the pathway was ready to formally launch.
“On the one hand, it feels good to offer a service like this that isn’t readily available,” says Taylor. “On the other hand, what a terrible indictment of our system that we’ve had to create this workaround pathway to get patients access to a life-saving medication.”
The problem with buprenorphine: fentanyl
Fentanyl, the synthetic opioid largely to blame for the dramatic rise in opioid overdoses the past eight years, has driven the exploding demand for methadone at Faster Paths.
“What we’re seeing is that methadone is more important than ever now, because of the influx of fentanyl into the opioid supply,” says Taylor. “People are having a harder time starting buprenorphine because of what we call precipitated withdrawal. This happens when someone takes buprenorphine too soon after taking another opioid like heroin or fentanyl, which causes them to get sick from opioid withdrawal.”
“The early days of the pathway have demonstrated it’s a needed service, it effectively links people to care, and they are sticking with their care.” Click To Tweet
Why is the switch from fentanyl to buprenorphine tougher than the switch from heroin to buprenorphine? Research on this topic is still emerging, says Walley. But he thinks the rough transition has to do with fentanyl’s interaction with body fat.
“Fentanyl is fast-acting and does not last long when taken acutely or once or twice. But it’s lipophilic, which means that it can be deposited in fat tissue. We think that the buildup of fentanyl in the fat of daily users increases the risk of precipitated withdrawal when people start taking buprenorphine.”
With heroin or oxycodone use, he says patients typically wait 12 hours to start buprenorphine without substantial risk of precipitated withdrawal. With fentanyl, it takes up to 72 hours or longer for many to tolerate starting buprenorphine–if they can tolerate it at all.
“Asking people to be abstinent for 72 hours is too tall of an order for those with opioid use disorder. If it was easy for them to be abstinent, we wouldn’t have this problem that we have.”
Pathway’s early days show ‘it’s a needed service’
Six months after piloting the pathway in March, Faster Paths saw a 50% jump in the overall number of patients, according to Taylor, most of which was due to visits for 72-hour methadone. In that period, there were 150 encounters among 142 patients for methadone withdrawal management. Among a group of 121 patients referred to two opioid treatment programs, 87% attended.
“Our patients face many barriers, including high rates of homelessness, criminalization, lack of transportation, trauma, and medical and psychiatric comorbidities. An 87% linkage rate is very high, and we’re incredibly excited that our pathway is getting patients to the next step of long-term care,” says Taylor.
Retention rates have been promising as well: 58% of the 121 patients remained in care one month later.
“I think the early days of the pathway have demonstrated it’s a needed service, it effectively links people to care, and they are sticking with their care.”
Making methadone as treatment more accessible
Making methadone treatment more accessible is a point of advocacy for Taylor, Walley, and the team at Faster Paths. For others as well. The National Academy of Sciences Engineering and Medicine, in a 2019 report , recommended loosening regulations and allowing patients to work with their providers to decide which medication is best for them.
“We need laws, regulations, and policies that really focus on making the life-saving treatments for opioid use disorder—methadone, buprenorphine, naltrexone—available whenever and wherever people need it,” says Walley.
That would mean allowing methadone in primary care and in pharmacies, as it is in the U.K., Canada, and Australia. In the U.S., the medication one gets often depends on where one shows up for care.
Using the 72-hour rule, Faster Paths has come one step closer to the truly offering patients the choice of all three medications in one setting on demand.
“Ambivalence is a hallmark of addiction. Most people with opioid use disorder have some ambivalence about continuing to use. At the same time, they have ambivalence about seeking treatment,” says Walley.
“When people are open to treatment, we need to be able to offer it to them and we need to be able to offer the best treatment for them in a way that works for them.”
HealthCity elevates the conversation around issues of equity in healthcare. Sign up for our newsletter.
Share on Social
Related articles.

New Center Will Scale Up Successful Approach to Pediatric Mental Health Care
by Meryl Bailey | Jul 31, 2024 | Mental Health & Addiction
BMC’s TEAM UP model has increased screening rates, expedited access to services, and yielded positive health outcomes for children in the Boston area. And now it’s expanding.

Practicing ‘Sawubona’ to Build a Legacy of Mental Health Care in Africa and the Diaspora
by Caitlin White | Jun 7, 2024 | Editor Picks , Mental Health & Addiction
Boston Medical Center’s Chief of Psychiatry co-founded the Africa Global Mental Health Institute to address the urgent need for culturally sensitive mental healthcare on the continent and beyond.
About the Author

David Limm is the digital editor of HealthCity.
HealthCity is dedicated to sharing the most cutting-edge ideas for advancing health justice through inspiring stories, in-depth Q&As with equity pioneers, research news that could change the medical landscape, and more.

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
To address the fentanyl crisis, greater access to methadone is needed
This blog was also published in the American Society of Addiction Medicine (ASAM) Weekly on July 24, 2024.

Over the past several years, the increasing prevalence of fentanyl in the drug supply has created an unprecedented overdose death rate and other devastating consequences. People with an opioid use disorder (OUD) urgently need treatment not just to protect them from overdosing but also to help them achieve recovery, but highly effective medications like buprenorphine and methadone remain underused. Amid this crisis, it is critical that methadone, in particular, be made more accessible, as it may hold unique clinical advantages in the age of fentanyl.
Growing evidence suggests that methadone is as safe and effective as buprenorphine for patients who use fentanyl. In a 2020 naturalistic follow-up study, 53% of patients admitted to methadone treatment who tested positive for fentanyl at intake were still in treatment a year later, compared to 47% for patients who tested negative. Almost all (99%) of those retained in treatment achieved remission . An earlier study similarly found that 89% of patients who tested positive for fentanyl at methadone treatment intake and who remained in treatment at 6 months achieved abstinence .
Methadone may even be preferable for patients considered to be at high risk for leaving OUD treatment and overdosing on fentanyl. Comparative effectiveness evidence is emerging which shows that people with OUD in British Columbia given buprenorphine/naloxone when initiating treatment were 60% more likely to discontinue treatment than those who received methadone (1). More research is needed on optimal methadone dosing in patients with high opioid tolerance due to use of fentanyl, as well as on induction protocols for these patients. It is possible that escalation to a therapeutic dose may need to be more rapid.
It remains the case that only a fraction of people who could benefit from medication treatment for OUD (MOUD) receive it, due to a combination of structural and attitudinal barriers. A study using data from the National Survey on Drug Use and Health (NSDUH) from 2019—that is, pre-pandemic—found that only slightly more than a quarter (27.8%) of people who needed OUD treatment in the past year had received medication to treat their disorder. But a year into the pandemic, in 2021, the proportion had dropped to just 1 in 5 .
Efforts have been made to expand access to MOUD. For instance, in 2021, the U.S. Department of Health and Human Services (HHS) advanced the most comprehensive Overdose Prevention Strategy to date. Under this strategy, in 2023, HHS eliminated the X-waiver requirement for buprenorphine. But in the fentanyl era, expanded access to methadone too is essential, although there are even greater attitudinal and structural barriers to overcome with this medication. People in methadone treatment, who must regularly visit an opioid treatment program (OTP), face stigma from their community and from providers . People in rural areas may have difficulty accessing or sticking with methadone treatment if they live far from an OTP.
SAMHSA’s changes to 42 CFR Part 8 (“Medications for the Treatment of Opioid Use Disorder”) on January 30, 2024 were another positive step taken under the HHS Overdose Prevention Strategy. The new rule makes permanent the increased take-home doses of methadone established in March 2020 during the COVID pandemic, along with other provisions aimed to broaden access like the ability to initiate methadone treatment via telehealth. Studies show that telehealth is associated with increased likelihood of receiving MOUD and that take-home doses increase treatment retention.
Those changes that were implemented during the COVID pandemic have not been associated with adverse outcomes. An analysis of CDC overdose death data from January 2019 to August 2021 found that the percentage of overdose deaths involving methadone relative to all drug overdose deaths declined from 4.5% to 3.2% in that period. Expanded methadone access also was not associated with significant changes in urine drug test results, emergency department visits, or increases in overdose deaths involving methadone. An analysis of reports to poison control centers found a small increase in intentional methadone exposures in the year following the loosening of federal methadone regulations, but no significant increases in exposure severity, hospitalizations, or deaths .
Patients themselves reported significant benefits from increased take-home methadone and other COVID-19 protocols. Patients at one California OTP in a small qualitative study reported increased autonomy and treatment engagement . Patients at three rural OTPs in Oregon reported increased self-efficacy, strengthened recovery, and reduced interpersonal conflict .
The U.S. still restricts methadone prescribing and dispensing more than most other countries, but worries over methadone’s safety and concerns about diversion have made some physicians and policymakers hesitant about policy changes that would further lower the guardrails around this medication. Methadone treatment, whether for OUD or pain, is not without risks. Some studies have found elevated rates of overdose during the induction and stabilization phase of maintenance treatment, potentially due to starting at too high a dose, escalating too rapidly, or drug interactions .
Although greatly increased prescribing of methadone to treat pain two decades ago was associated with diversion and a rise in methadone overdoses, overdoses declined after 2006, along with methadone’s use as an analgesic, even as its use for OUD increased. Most methadone overdoses are associated with diversion and, less often, prescription for chronic pain; currently, 70 percent of methadone overdoses involve other opioids (like fentanyl) or benzodiazepines .
Recent trials of models of methadone dispensing in pharmacies and models of care based in other settings than OTPs have not supported concerns that making methadone more widely available will lead to harms like overdose. In two feasibility studies, stably maintained patients from OTPs in Baltimore, Maryland and Raleigh, North Carolina who received their methadone from a local pharmacy found this model to be highly satisfactory, with no positive urine screens, adverse events, or safety issues. An older pilot study in New Mexico found that prescribing methadone in a doctor’s office and dispensing in a community pharmacy, as well as methadone treatment delivered by social workers, produced better outcomes than standard care in an OTP for a sample of stably maintained female methadone patients.
Critics of expanded access to methadone outside OTPs sometimes argue that the medication should not be offered without accompanying behavioral treatment. Data suggest that counseling is not essential. In wait-list studies , methadone treatment was effective at reducing opioid use on its own, and patients stayed in treatment. However, counseling may have benefits or even be indispensable for some patients to help them improve their psychosocial functioning and reduce other drug use. How to personalize the intensity and the level of support needed is a question that requires further investigation.
Over the past two decades, the opioid crisis has accelerated the integration of addiction care in the U.S. with mainstream medicine. Yet methadone, the oldest and still one of the most effective medications in our OUD treatment toolkit, remains siloed. In the current era of powerful synthetic opioids like fentanyl dominating the statistics on drug addiction and overdose, it is time to make this effective medication more accessible to all who could benefit. The recent rules making permanent the COVID-19 provisions are an essential step in the right direction, but it will be critical to pursue other ways that methadone can safely be made more available to a wider range of patients with OUD. Although more research would be of value, the initial evidence suggests that providing methadone outside of OTPs is feasible, acceptable, and leads to good outcomes.
- Nosyk B, Min JE, Homayra F, Kurz M, Guerra-Alejos BC, Yan R, et al, Comparative effectiveness of buprenorphine/naloxone versus methadone for treatment of opioid use disorder: emulating target trials with population-level data. Poster session presented at: The College on Problems of Drug Dependence (CPDD) 86th Annual Scientific Meeting; 2024 Jun 15-19; Montreal, CAN.

Dr. Nora Volkow, Director
Here I highlight important work being done at NIDA and other news related to the science of drug use and addiction.
Recent Blog Posts

We should leverage the successes of HIV care to prevent overdose mortality

Everyone deserves addiction treatment that works — including those in jail
50 years after founding, NIDA urges following science to move beyond stigma
Quality Care
Publications, guest editorial: to address the fentanyl crisis, greater access to methadone is needed.substring(0, maxlength), guest editorial: to address the fentanyl crisis, greater access to methadone is needed.
By Nora D. Volkow, MD
Director, National Institute on Drug Abuse (NIDA) at the National Institutes of Health NIDA is the world’s largest funder of scientific research on the health aspects of drug use and addiction.
Over the past several years, the increasing prevalence of fentanyl in the drug supply has created an unprecedented overdose death rate and other devastating consequences. People with an opioid use disorder (OUD) urgently need treatment not just to protect them from overdosing but also to help them achieve recovery, but highly effective medications like buprenorphine and methadone remain underused. Amid this crisis, it is critical that methadone be made more accessible, as it may hold unique clinical advantages in the age of fentanyl.
Growing evidence suggests that methadone is as safe and effective as buprenorphine for patients who use fentanyl. In a 2020 naturalistic follow-up study, 53% of patients admitted to methadone treatment who tested positive for fentanyl at intake were still in treatment a year later, compared to 47% for patients who tested negative. Almost all (99%) of those retained in treatment achieved remission . An earlier study similarly found that 89% of patients who tested positive for fentanyl at methadone treatment intake and who remained in treatment at 6 months achieved abstinence .
Methadone may even be preferable for patients considered to be at high risk for leaving OUD treatment and overdosing on fentanyl. Comparative effectiveness evidence is emerging which shows that people with OUD in British Columbia given buprenorphine/naloxone when initiating treatment were 60% more likely to discontinue treatment than those who received methadone.i More research is needed on optimal methadone dosing in patients with high opioid tolerance due to use of fentanyl, as well as on induction protocols for these patients. It is possible that escalation to a therapeutic dose may need to be more rapid.
It remains the case that only a fraction of people who could benefit from medication treatment for OUD (MOUD) receive it, due to a combination of structural and attitudinal barriers. A study using data from the National Survey on Drug Use and Health (NSDUH) from 2019 (pre-pandemic) found that only slightly more than a quarter (27.8%) of people who needed OUD treatment in the past year had received medication to treat their disorder. But a year into the pandemic, in 2021, the proportion had dropped to just 1 in 5 .
Efforts have been made to expand access to MOUD. For instance, in 2021, the U.S. Department of Health and Human Services (HHS) advanced the most comprehensive Overdose Prevention Strategy to date. Under this strategy, in 2023, HHS eliminated the X-waiver requirement for buprenorphine. But in the fentanyl era, expanded access to methadone too is essential, although there are even greater attitudinal and structural barriers to overcome with this medication. People in methadone treatment, who must regularly visit an opioid treatment program (OTP), face stigma from their community and from providers . People in rural areas may have difficulty accessing or sticking with methadone treatment if they live far from an OTP.
SAMHSA’s changes to 42 CFR Part 8 (“Medications for the Treatment of Opioid Use Disorder”) on January 30, 2024 were another positive step taken under the HHS Overdose Prevention Strategy. The new rule makes permanent the increased take-home doses of methadone established in March 2020 during the COVID pandemic, along with other provisions aimed to broaden access like the ability to initiate methadone treatment via telehealth. Studies show that telehealth is associated with increased likelihood of receiving MOUD and that take-home doses increase treatment retention.
Changes implemented during the COVID pandemic have not been associated with adverse outcomes. An analysis of CDC overdose death data from January 2019 to August 2021 found that the percentage of overdose deaths involving methadone relative to all drug overdose deaths declined from 4.5% to 3.2% in that period. Expanded methadone access also was not associated with significant changes in urine drug test results, emergency department visits, or increases in overdose deaths involving methadone. An analysis of reports to poison control centers found a small increase in intentional methadone exposures in the year following the loosening of federal methadone regulations, but no significant increases in exposure severity, hospitalizations, or deaths.
Patients themselves reported significant benefits from increased take-home methadone and other COVID-19 protocols. Patients at one California OTP in a small qualitative study reported increased autonomy and treatment engagement . Patients at three rural OTPs in Oregon reported increased self-efficacy, strengthened recovery, and reduced interpersonal conflict .
The U.S. still restricts methadone prescribing and dispensing more than most other countries but worries over methadone’s safety and concerns about diversion have made some physicians and policymakers hesitant about policy changes that would further lower the guardrails around this medication. Methadone treatment, whether for OUD or pain, is not without risks. Some studies have found elevated rates of overdose during the induction and stabilization phase of maintenance treatment, potentially due to starting at too high a dose, escalating too rapidly, or drug interactions .
Although increased prescribing of methadone to treat pain two decades ago was associated with diversion and a rise in methadone overdoses, overdoses declined after 2006, along with methadone’s use as an analgesic, even as its use for OUD increased. Most methadone overdoses are associated with diversion and, less often, prescription for chronic pain; currently, 70 percent of methadone overdoses involve other opioids (like fentanyl) or benzodiazepines .ii
Recent trials of models of methadone dispensing in pharmacies and models of care based in other settings than OTPs have not supported concerns that making methadone more widely available will lead to harms like overdose. In two feasibility studies, stably maintained patients from OTPs in Baltimore, Maryland and Raleigh, North Carolina who received their methadone from a local pharmacy found this model to be highly satisfactory, with no positive urine screens, adverse events, or safety issues. An older pilot study in New Mexico found that prescribing methadone in a doctor’s office and dispensing in a community pharmacy, as well as methadone treatment delivered by social workers, produced better outcomes than standard care in an OTP for a sample of stably maintained female methadone patients.
Critics of expanded access to methadone outside OTPs sometimes argue that the medication should not be offered without accompanying behavioral treatment. Data suggest that counseling is not essential. In waitlist studies , methadone treatment was effective at reducing opioid use on its own, and patients stayed in treatment. However, counseling may have benefits or even be indispensable for some patients to help them improve their psychosocial functioning and reduce other drug use. How to personalize the intensity and the level of support needed is a question that requires further investigation.
Over the past two decades, the opioid crisis has accelerated the integration of addiction care in the U.S. with mainstream medicine. Yet methadone, the oldest and still one of the most effective medications in our OUD treatment toolkit, remains siloed. In the current era of powerful synthetic opioids like fentanyl dominating the statistics on drug addiction and overdose, it is time to make this effective medication more accessible to all who could benefit. The recent rules making permanent the COVID-19 provisions are an essential step in the right direction, but it will be critical to pursue other ways that methadone can safely be made more available to a wider range of patients with OUD. Although more research would be of value, the initial evidence suggests that providing methadone outside of OTPs is feasible, acceptable, and leads to good outcomes.
Advertisement
Supported by
Britain’s Weekend of Violence: What We Know
The country begins a new week on edge after anti-immigrant riots, fanned by disinformation from the far right, broke out in cities across Britain.
- Share full article

By The New York Times
After a weekend of violent uprisings across Britain, set off by a deadly stabbing rampage and a disinformation campaign aimed primarily at immigrant Muslims that followed it, tensions are high from the streets to government leaders’ offices.
Here is what we know as the country enters a new week of uncertainty.
Where has the unrest taken place?
Protesters over the weekend took to the streets of a dozen cities across the United Kingdom, most of them in England. Trouble broke out from Aldershot in the south to Sunderland in the north and Liverpool in the west. Belfast, in Northern Ireland, was also drawn into the fray.
In some cases, the protesters were merely unruly, but in others the violence was far more pronounced.
Where arrests have been reported
On Sunday, rioters set upon a hotel that was housing asylum seekers in the town of Rotherham, in northern England, breaking windows before surging inside as the police struggled to control them. No guests were injured in the melee, the police said.
In Middlesbrough, a group of rioters, some masked, hurled bottles and rocks at officers. Cars were set on fire, and at least nine people were arrested. On Saturday, a library and a food bank were set alight in Liverpool as groups damaged and looted businesses, and in Hull, fires were set and storefronts smashed in the city center.
We are having trouble retrieving the article content.
Please enable JavaScript in your browser settings.
Thank you for your patience while we verify access. If you are in Reader mode please exit and log into your Times account, or subscribe for all of The Times.
Thank you for your patience while we verify access.
Already a subscriber? Log in .
Want all of The Times? Subscribe .

Methadone treatment raises questions about profit motive, patient care
DAYTONA BEACH — It's 5 a.m., and the streets are deserted.
But at the Daytona Methadone Treatment Center, more than 100 people stand in line for their daily dose of methadone, a drug that helps quell cravings for heroin and oxycodone.
The orange glows from cigarettes puncture the darkness as a security guard paces in the parking lot. A few people sit in chairs near the entrance of Florida's second-busiest clinic like Black Friday shoppers waiting for a doorbuster sale.
But this isn't a holiday. It's not a special occasion. For these people, it's a daily ritual.
As part of the $14 people pay for their daily methadone dose, clients are supposed to have access to counselors to help them with their recovery.
Yet counselor caseloads at Daytona Beach's methadone clinic have been two to three times higher than what they are supposed to be under state regulations, records show. And fewer than 2 percent of the 1,800 clients served by the clinic were weaned off the drug or successfully discharged from the program during the 2011-12 fiscal year, the last year for which records are available.
Methadone treatment is seen by the Centers for Disease Control and Prevention and others as an intervention that helps addicts get their lives back. One advocate who's taken a daily dose of the drug for more than 40 years says methadone saved her life.
At the same time, the treatment has long faced backlash from critics who say it simply swaps one drug for another. For-profit providers like Orlando-based Colonial Management Group, the company that runs the Daytona clinic, have come under fire from those who view them as "dose-and-go" operations that put profits ahead of patient care.
In Minnesota, inspectors are in the process of revoking the license of a Colonial Management methadone clinic where counselors had similarly high caseloads and other compliance issues.
In Florida, though, regulators rewarded the Daytona Beach clinic with a performance rating of 94 out of a possible 100 points.
A FOR-PROFIT BUSINESS
Methadone maintenance treatment programs were developed during the 1960s, primarily to help heroin users. Getting addicts off needles, which can spread disease, was seen at the time as a major benefit of treatment.
The drug works by occupying the same brain receptors as heroin and other opioids, such as oxycodone, hydrocodone and morphine — drugs often used as painkillers that can lead to dependence. Quitting can cause aches, chills, vomiting, diarrhea and anxiety.
To be admitted, clients must be addicted to opioids for at least a year. Treatment providers can accept medical records, statements from loved ones and arrest records to determine a person has been addicted for at least a year.
Methadone relieves withdrawal symptoms and combats the craving for opioids. It's cheaper than the other drugs and is excreted so slowly it can be taken once a day. If administered properly, it's not intoxicating. While it produces dependence, if the dosage is slowly reduced over time methadone users can be weaned off without painful withdrawal symptoms.
That doesn't mean it's harmless. Though methadone comprised only 2 percent of painkiller prescriptions in 2009, it was involved in 30 percent of the 15,500 prescription painkiller overdose deaths that year, according to the Centers for Disease Control and Prevention. Because it has a longer half-life than other opioids, it is more likely to build up in a person's body and depress the respiratory system or have adverse reactions with other drugs.
Pill mills and an explosion of painkiller abuse have brought tremendous growth to the methadone industry, said Mark Parrino, president of the American Association for the Treatment of Opioid Dependence.
The industry has been identified as one of the most lucrative sectors in health care because of its cash-only nature and high profit margin. In 2006, Bain Capital, the private equity firm co-founded by former Republican presidential contender Mitt Romney, paid $723 million to acquire CRC Health Group, the nation's largest chain of for-profit methadone clinics, according to corporate filings. (Romney left Bain seven years before it acquired CRC.)
The past 10 years have seen about 200 new opioid treatment programs open, a significant amount considering only 1,250 programs are in operation nationwide. Most of those new clinics have been for-profit entities, Parrino said, because states and local governments are reluctant to devote funding to methadone maintenance treatment.
That's the case in Daytona Beach, where the clinic is operated by Colonial Management, which runs 56 other treatment centers in 18 states.
The Daytona Beach clinic's program director referred questions to Colonial Management's corporate office. Mike Ford, director of accreditation and corporate compliance, said company officials would not comment for this story.
Business is good at the Daytona Beach clinic, which serves Volusia and Flagler counties. Last year, it moved from International Speedway Boulevard near Bethune-Cookman University to a nondescript office building near the Veterans Affairs clinic just off Bill France Boulevard to accommodate more patients.
Even with the larger location, the state has determined a need exists for three more clinics in northeast Florida, making it one of the most underserved parts of the state. The northeast region includes Volusia, Flagler, St. Johns and Duval counties, along with 16 other counties. On Feb. 21, Colonial opened a new clinic in St. Augustine.
The next closest clinics are in Orlando, Jacksonville and Brevard County. Flagler County does not have a methadone clinic.
The Daytona Beach treatment center accepts cash, traveler's checks and money orders only — no credit cards or personal checks, according to guidelines given to patients. Medicaid is not accepted, and patients are given little leeway if they are unable to pay.
Profits generated through continued methadone treatment often overlap with what is best for the patient, Parrino said. He compared the treatment to providing insulin to a diabetic or administering cholesterol-lowering drugs.
"The general view is retention (in a methadone program) and treatment is considered favorable, not unfavorable," Parrino said. "I think people look at addiction to drugs in a unique framework. It's an illness. It's a disease, and it's a treatable disease."
A PATIENT'S EXPERIENCE
Tracy Williams used to be one of the people standing outside the Daytona Beach methadone clinic.
Clinics dispense the drug early in the morning with the idea that patients can get their dose and still get to work. Federal and state regulations prohibit patients from receiving take-home doses until they demonstrate they are adhering to the clinic guidelines and are not taking other drugs.
Wanting to avoid long waits, clients arrive early to drink their dose, which must be taken in person to avoid abuse. In Daytona Beach, dosing starts at 5 a.m. on weekdays.
Williams, 29, had been addicted to oxycodone until she was jailed last summer in Volusia County for theft — while she was pregnant.
Because opioid withdrawal can be damaging to a fetus, she was prescribed methadone. A guard took her to the methadone clinic for a daily dose of 20 milligrams, which Williams said should have been sufficient to quell her cravings without intoxicating her.
But she said she kept asking for more methadone as a way to feel high while in jail. The clinic obliged, upping her dosage to 125 milligrams, she said.
"I think a lot of people are using the methadone clinic as a way to get high," she said.
Williams paid the price upon her release from jail.
She was living in Lake County and had to drive to Daytona Beach every morning. Her methadone was costing her $100 a week, more than she could afford. The higher dosage she'd started taking in jail meant it would take her longer to undergo detoxification — if she ever got off the drug.
Counselors were swamped, and it seemed the clinic focused more on dosing than helping patients work through their issues with therapy, Williams said.
Finally, out of options, she recalled coming to the clinic one day with tears rolling down her cheeks. She was seven and a half months pregnant, out of money and still dependent on the drug.
Though 18 of Florida's 35 clinics were licensed during the 2011-12 fiscal year to accept Medicaid, a federal-state program that helps pay for health care for the needy, the Daytona Beach clinic does not.
"They told me there was nothing they could do — pretty much I was left lingering," Williams said.
Abrupt withdrawal from opioids addiction can result in "preterm labor, fetal distress or fetal demise," according to the American Congress of Obstetricians and Gynecologists, which advises physicians to keep dependent pregnant women on methadone through the duration of their pregnancy.
Through her gynecologist, Dr. Pam Carbiener, Williams managed to secure a waiver that allowed her to pay for the drug through Medicaid. But that was far from the end of her troubles.
QUESTIONS ABOUT COLONIAL
Questions have been raised in other states about Colonial Management Group's business practices and its adherence to federal and state regulations.
In September, the Minnesota Department of Human Services issued an order of revocation for a Colonial Management Group clinic in Duluth after inspectors found the clinic had excessive counselor caseloads, insufficient training and "a clearly demonstrated failure by the program director to understand the licensing regulations."
Colonial Management is appealing the state's revocation.
Minnesota's action came two years after a class-action lawsuit filed in Montgomery, Ala., accused Colonial Management of failing to provide counseling. The case was settled, said a spokeswoman for the law firm that brought the suit.
In Florida, counselors at methadone clinics must have a caseload equivalent of no more than 32 clients. The state uses a complex formula based on how often a client must be seen to calculate counselor loads. When inspectors visited the Daytona Beach clinic in September, they found some counselors had caseloads that were two to three times higher than state requirements.
Regulators could have fined the clinic, suspended or revoked its license or issued a moratorium on accepting new patients. But none of those actions were taken.
Instead, the clinic achieved a performance rating score of 94.25 on a 100-point scale.
State officials reviewed the performance rating following questions from The News-Journal. They said at the time the inspection was done, the clinic had just moved into its new building and was under new management. Counselor vacancies have since been filled, officials said, and the clinic is in compliance with staffing levels.
"We are doing a good job of managing methadone as a controlled substance," said Sheila Barbee, team leader for substance abuse with the Department of Children and Families. "This is an area we take very seriously. I think we have good staff in the field, and we have good standards."
In the Minnesota case, inspectors took action after finding recurring excessive caseloads that were similar to what Florida found at the Daytona Beach clinic.
What inspectors found at a Colonial Management clinic in Duluth was troubling, said Jerry Kerber, inspector general for the Minnesota Department of Human Services.
"It is intended in Minnesota to be more than a dose-and-go kind of service," he said. "It's more than picking up methadone and going on their way."
COUNSELING VS. TREATMENT
Methadone treatment isn't necessarily intended to wean patients from the drug. Dr. Kelly Clark, chief medical officer at another for-profit methadone provider, said the larger goal is to ensure patients are achieving their highest level of functioning at the lowest possible dose.
Clark compared methadone doses to a nicotine patch. Even though former smokers are not entirely nicotine free, they are still avoiding cancer-causing chemicals found in cigarette smoke.
A good clinic, whether it's for-profit or not-for-profit, will gain referrals if it is able to help addicts get their lives back, she said.
"I don't think there is any misalignment when there is a profit motive in providing medical care," said Clark, chief medical officer for Dallas-based Behavioral Health Group and a member of the American Society of Addiction Medicine's Board of Directors. "(Opioid treatment programs) are a classic example of doing well by doing good. You do well by doing good work."
Society benefits when addicts are shifted to methadone from costlier, illicit street drugs, said Dr. Bruce A. Goldberger, director of toxicology at the University of Florida College of Medicine.
Methadone treatment stops addicts from trading drugs for sex, injecting or smoking drugs or resorting to theft to support their expensive habit, Goldberger said. The street value of a single pill of oxycodone can be $20, and addicts can spend more than $100 a day on their habit.
Because methadone is slower acting, patients can take their dose once a day and then lead a productive life, he said.
"It's not like we are just swapping one drug for another and letting this person go along with their addiction," Goldberger said.
While no one doubts methadone is a better alternative to heroin, some question the commitment to counseling at the clinics.
While medication can play an important role, counseling is invaluable when it comes to combating drug addiction, said Randy Croy, the longtime director of Haven Recovery Center, a substance abuse treatment program headquartered in Daytona Beach.
"It's my experience that medications without counseling are insufficient to accomplish that goal of getting people clean, sober and productive," Croy said. "Thus, most of us in the treatment world feel that counseling — whether inpatient, outpatient or supportive — is critical to long-term success in recovery."
For clinics that rely on addicts for daily cash payments, there's little incentive to help them break their dependency, said Steven Hayes, who ran the Novus Medical Detox Center in Port Richey and is one of Florida's most outspoken critics of methadone treatment.
"The problem with methadone usage is it's like any other opioid," he said. "If you are not particularly disciplined, you keep seeing the dose go up. Obviously, the clinics profit."
Detoxification and counseling would be the better first approach to helping opioid addicts, Hayes said. Instead, patients — even those who have been using only a short time — start going to for-profit methadone clinics.
"Their profit model is to increase the sale of their drugs," Hayes said. "Are they going to put themselves out of business? Upton Sinclair said, 'It's difficult to get a man to understand something when his salary depends on his not understanding it.' "
Nanette Wollfarth's understanding is simple. Having been hooked on heroin as a teen, she says getting on methadone made it possible for her to have a salary and a normal life.
"I would have been dead — no doubt," said Wollfarth, whose account is similar to a long string of testimonials trumpeting the drug's life-changing possibilities on Colonial Management's website.
Now 64, Wollfarth has been using methadone for 42 years. Without it, she doubts she would have been able to open her own beauty salon. She estimates she and her husband — who also uses methadone — have spent more than $250,000 over the past four decades on the drug.
Based on her experience, Wollfarth, who lives near Gainesville, said younger patients who get on methadone shouldn't expect to wean themselves off the drug in a couple of years.
"It's a lifetime commitment," she said.
NEVER GOT TO HOLD HER
Williams is one of the patients who managed to get off methadone, but it didn't lead to the happy ending she dreamed of while expecting her baby.
Her baby, Heavenlee, was born with gastroschisis, a birth defect in which an infant's intestines stick out of its body. The baby battled for its life for four days before dying in an Orlando hospital.
Williams' doctor said drug use likely played no role in the defect, but the experience had a radical effect on the young mother, and no amount of assurances can assuage her guilt.
"I know the baby died from all the drugs I was using," she said. "Instead of wanting them, I despise them. They took something from me."
Afterward, she immediately entered a detox program to free herself from methadone.
A box filled with memories of Heavenlee rests on a shelf in the hall of Williams' DeLand home. It is a memorial to the daughter she lost — and a reminder of a lifestyle she intends to never experience again.
Inside the box are the baby's bracelet and a tiny diaper that would have fit her 3 pound, 8 ounce body. Pictures of Heavenlee surrounded with tubes are there, too, but Williams can't stand to look at them.
Her hands shook as she removed photographs from the box. As she handed the pictures over, she looked away to avoid catching a glimpse.
"I never got to hold her," she said.
Tears rolled down Williams' cheek as she returned the items to the box and slid it back on the shelf.
Benefits of methadone treatment
Critics of methadone say it just swaps one drug for another and doesn't address the root cause of addiction. In a 2002 fact sheet, the Centers for Disease Control and Prevention found several benefits of methadone maintenance treatment.
- reduced or stopped use of injection drugs
- reduced risk of acquiring or spreading diseases, such as HIV or hepatitis
- reduced chance of overdose; the median death rate of dependent individuals in methadone maintenance treatment is 30 percent of the rate of those not in a methadone treatment program
- possible reduction in sexual risk behaviors
- reduced criminal activity
- improved family stability and employment potential
- improved pregnancy outcomes
SOURCE: Centers for Disease Control and Prevention
Busiest methadone clinics in Florida
Colonial Management Group operates four of the five busiest methadone clinics in the state.
1. Orlando Metro Treatment Center: 2,016 clients
2. Daytona Methadone Treatment Center: 1,824 clients
3. Jacksonville Metro Treatment Center: 1,355 clients
4. Bay Area Treatment Center (Pinellas County): 1,022 clients
5. Drug Abuse Comprehensive Coordinating Office Inc. (Pinellas County): 800 clients
* Census numbers are from Dec. 13.
SOURCE: Florida Department of Children and Families
Getting clean has its costs — and profits
Pill addicts can easily spend hundreds of dollars a week to feed their habit.
But getting access to methadone or another drug to help them quit isn't cheap either. At the Daytona Beach Methadone Treatment Center, clients spend about $100 a week to get their daily dose of methadone.
Buprenorphine, a newer maintenance drug sold under the brand name Suboxone that came to market in 2002, costs even more. Clients will spend $175 per week for this alternative to methadone.
Because of the cash-only nature of the methadone business, addiction and substance abuse treatment providers have emerged "as some of the most sought after — and valuable — acquisition candidates in health care," according to The Braff Group, a Pittsburgh-based mergers and acquisitions company.
Providers in this health care sector frequently run profit margins of more than 10 percent and often approaching 20 percent or more, according to Braff.
Not all clinics are cash-only businesses, though. In Florida, providers can elect to accept Medicaid, which pays up to $67.48 a week for methadone treatment. In total, Florida's Medicaid program paid out $9.5 million for methadone treatment during the 2011-12 fiscal year, according to the Agency for Health Care Administration.
The closest clinics to Daytona Beach that accept Medicaid are in Jacksonville and Orlando.
Rules designed to safeguard against abuse
In some states, concerns are mounting that methadone clinics are contributing to the illicit sale of the drug, as well as overdoses, despite tight regulations on take-home doses.
Clients can take home doses of methadone if they demonstrate good behavior and pass drug screens. After 30 days of compliance, clients can take home one dose a week. That amount increases to up to six doses a week after three years of compliance, according to state regulations.
"It's not completely foolproof because we do see it on the streets," said Dan Danielson, an investigator with the Carlton County Sheriff's Office in Minnesota. "There is a huge amount of pressure on users who bring it home to flip it for cash or trade it for other products."
Locally, illegal methadone sales have not been a significant problem, said Brandon Haught, a spokesman for the Volusia County Sheriff's Office. For the few cases investigators have encountered, it's been difficult to determine where the methadone originated.
To guard against abuse, clinics send doses home in locked boxes and conduct random audits to ensure the medication is taken correctly, said Dr. Kelly Clark, chief medical officer for the methadone provider Behavioral Health Group. Patients who abuse the drug are terminated from the treatment program.
Methadone clinics are being unfairly blamed for overdose deaths and illicit sales, Clark said. A bigger culprit is the prescribing of methadone for pain management, which allows the drug to be taken home in larger batches with less oversight, she said.
Federal authorities have been active recently in ensuring methadone clinics are keeping up with the drugs they dispense.
In March, the U.S. Department of Justice levied a $95,000 fine in a settlement with Colonial Management Group's clinic in Huntsville, Ala., because the clinic could not account for 3,423 doses of methadone. It was the largest penalty ever collected in Alabama in a Drug Enforcement Administration diversion investigation. The clinic denied any intentional violation of regulations and revised its record-keeping at the DEA's request.
- Politics & Government
- National Politics
Building owners kill plan for methadone clinic
The owners of an industrial building at 708 W. Magazine St. where a Texas company proposed opening a controversial methadone clinic have ended all negotiations with the firm.
The owners, Brain Chase and Walter Crutcher, sent an email Friday to BayMark Health Services saying they side with Seven Counties Services in opposing the clinic that would dispense methadone in an attempt to cure primarily heroin addicts.
Seven Counties rents about 40,000 square feet of space in the two-story, 120,000-square-foot building along Seventh Street. The meth clinic would have occupied about 7,500 square feet.
Seven County officials had opposed the clinic as unnecessary and saw it as an attempt by a private company to make a profit off Louisville's serious heroin problem .
Nick Pregliasco, the Louisville attorney for BayMark, said he didn't have any comment on the building owners' decision. He said BayMark has an extensive site-selection process for its clinics and that he wouldn't be surprised if the company looked elsewhere in Louisville for a location for the methadone clinic.
►RELATED: Heroin Resource Guide: Local places to get help
The decision not to negotiate a lease for the clinic was termed wonderful news by Gwen Cooper, the Seven Counties Services spokeswoman. "We provide comprehensive services in that building and will continue to do so. We are thrilled that the community stood behind Seven Counties Services."
Chase said Friday that he and Crutcher, partners in 708 W. Magazine Street LLC that owns the building, sent an email earlier in the day to BayMark, advising that the clinic plans at the site are history.
He provided a copy of the email that said, "We hereby support our major tenant Seven Counties Services' desire to stay and operate (its own) drug rehabilitation clinic at our location. ... We are hereby closing any further negotiations with Baymark Health."
The owners said, "We support the work and local community efforts (that) Seven Counties provides to its clientele and to the local community."
An initial community meeting Monday on plans for the downtown methadone clinic met some strenuous opposition that included concerns by officials of Seven Counties, a public health-services agency that would share space in the downtown building with the methadone clinic.
Other objectors included a former heroin addict, an employee of the nearby Federal Building, and a resident of the Russell neighborhood.
BayMark, of Lewisville, Texas, hosted the public meeting at the Western Library to explain the plans and field questions. It had intended to file an application for a needed permit with the Metro Board of Zoning Adjustment. Other approvals are also would have been required, including a state-issued license.
The Magazine Street building dates to 1956, and Seven Counties rents space there for its adult services operations. Its activities include group therapy, outpatient drug-addiction treatment, recovery programs, and services for those with mental-health problems.
Seven Counties doesn't use methadone to treat addiction. Dr. Anthony Zipple, Seven Counties CEO, said, "Seven Counties already operates comprehensive behavioral health services at this very location, including medication-assisted treatment, intensive outpatient treatment for addictions, and other services for people with opiate addiction."
Zipple said, "We get great results, without the use of methadone."
He added that "opening a new addictions-treatment program in the same building as an existing clinic is simply a bad idea."
BayMark currently operates more than 40 drug-treatment clinics in nine states, but a Louisville clinic would be its first in Kentucky.
The city planning staff and the county attorney's office, at the direction of the Louisville Metro Council, are currently studying possible guidelines for methadone clinics. Current regulations are few.
There are two operating methadone clinics in Louisville — one run by the Metro Health Department on 15th Street and a privately operated site, the Center for Behavioral Health, in St. Matthews. Those sites, respectively, are treating about 1,300 and 300 patients, BayMark said.
Methadone is a federally controlled substance — and a synthetic opiate that is consumed orally. It tends to counteract the ill effects of heroin and some other narcotics.
Reporter Sheldon S. Shafer can be reached at (502) 582-7089, or via email at [email protected].

COMMENTS
Marketing promotion expenses for the grand opening of Jason Collins® Methadone Clinic, Inc. in the amount of $3,500 and as well as flyer printing (2,000 flyers at $0.04 per copy) for the total amount of - $3,580. The cost for hiring business consultant - $2,500.
But addiction is certainly a big part of the business. It has more than 100 inpatient detox and rehab centers and runs 110 opioid treatment programs, better known as methadone clinics, ...
SAMHSA's OTP Compliance Officers will review all documentation to confirm the OTP is eligible for certification to provide treatment under 42 CFR 8. Programs seeking provisional certification as an OTP must use the online Form SMA-162: Application for Certification to Use Opioid Drugs in a Treatment Program. Each application requires different ...
Overview. Opioid treatment programs (OTPs) are the only health care facilities that can offer patients all three forms of FDA-approved medication for opioid use disorder (OUD): methadone, buprenorphine, and injectable extended-release naltrexone. 1 But Pew found that nearly all states have rules governing OTPs that are not based in evidence and in turn limit access to care or worsen patient ...
On February 1, 2024, the Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services, announced a final rule updating the regulations regarding Opioid Treatment Programs (OTPs) as part of the Biden Administration's Overdose Prevention Strategy. These announced changes are the first update to the OTP regulations in over 20 years and ...
Grants to Focus on Increasing Access to Medication-Assisted Treatment for People Battling Opioid Use Disorder. Today, the Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), is announcing two grant programs totaling $25.6 million that will expand access to medication-assisted treatment for opioid use disorder and ...
A liquid dose of methadone at the clinic in Rossville, Ga. The medication is only available at designated opioid treatment centers and that won't change. But more clinicians will be able to ...
The overdose and addiction crisis continues to intensify, taking the lives of more than 100,000 Americans in 2021. Despite strong evidence that the three Food and Drug Administration (FDA ...
Business Plan for Medication-Assisted Treatment. Presents a business plan for health centers and practices who treat opioid use disorder (OUD). Source. Providers Clinical Support System and National Association of Community Health Centers. Link.
Opioid treatment programs (OTPs) like Methadone clinics offer medication to assist someone with an addiction to opioids. Methadone is a synthetic opioid given at minimal doses under the supervision of medical staff daily. It has a long history of successfully helping people with opioid use disorders (OUDs), as it blocks the effects of opioids ...
Federal statutes, regulations, and guidelines govern medications for opioid addiction. SAMHSA's Division of Pharmacologic Therapies (DPT), part of SAMHSA's Center for Substance Abuse Treatment (CSAT), manages the day-to-day oversight activates required to implement federal regulations surrounding the use medications approved by the Food and Drug Administration (FDA) such as methadone and ...
Methadone has been used for decades to treat opioid addiction. It is also difficult to come by, a problem health providers hope to ease with a new fleet of vans that can provide the drug.
T he federal government is unveiling new regulations meant to modernize methadone treatment, the first major update to patient care standards at methadone clinics in more than 20 years. The new ...
Methadone clinics are not free; however, public methadone clinics are usually more affordable. More than 2 million people in the U.S. abuse opioids and more than 90 Americans die of an opioid overdose every day. Methadone is a long-acting synthetic opioid that may be used to treat opioid addiction and chronic pain.
The U.S. Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), is announcing Notices of Funding Opportunities (NOFOs) for five grant programs aimed at preventing substance misuse and treating substance use disorder (SUD) throughout the nation. The grant opportunities total about $73.4 million and align with the Biden ...
Methadone Maintenance Treatment (MMT) is widely recognized as one of the most effective ways of reducing risk of overdose, arrest, and transmission of blood-borne viruses like HIV and HCV among people that use opioids. Yet, MMT's use of restrictive take-home dose policies that force most patients to attend their clinic on a daily, or near-daily, basis may be unpopular with many patients and ...
As life-changing as methadone is, the catch is that taking the tightly regulated medication requires reporting to a special clinic nearly every day to get one's dose. When the Covid-19 pandemic ...
Grays Harbor Comprehensive Treatment Center . Acadia Healthcare 516 East 1st St. Aberdeen, WA 98520. mobile-screen-button (877) 774-6565 • 360-743-4610. King County. Bothell Comprehensive Treatment Center. Acadia Healthcare 22026 20th Ave SE, Ste 101 . Bothell, WA 98021. mobile-screen-button (425) 672-7293 • 877-541-4619 Evergreen Treatment ...
Drug Administration." Currently, these drugs are methadone and pharmaceutical products containing buprenorphine, hereafter referred to as buprenorphine. The regulations apply equally to both of these medications, with the only difference being the time and treatment requirement for unsupervised dosing spelled out in 42 CFR § 8.12(i)(3).
According to a case study published in Addiction Science & Clinical Practice, Faster Paths may be the first bridge clinic to offer methadone for emergency opioid withdrawal management while referring patients to ongoing care. Methadone, an opioid agonist, is a first-line treatment for opioid use disorder. Taylor calls it a life-saving treatment ...
Critics of expanded access to methadone outside OTPs sometimes argue that the medication should not be offered without accompanying behavioral treatment. Data suggest that counseling is not essential. In wait-list studies, methadone treatment was effective at reducing opioid use on its own, and patients stayed in treatment. However, counseling ...
Common dosing strategies for opioid use disorder include 50 mg per day (can start with 25 mg daily for a few days to mitigate side effects). 30. , 31. A typical daily dose (50 mg) will block the pharmacologic effects of 25 mg intravenous (IV) heroin up to 24 hours, with increasing doses extending the duration. 50.
Critics of expanded access to methadone outside OTPs sometimes argue that the medication should not be offered without accompanying behavioral treatment. Data suggest that counseling is not essential. In waitlist studies, methadone treatment was effective at reducing opioid use on its own, and patients stayed in treatment. However, counseling ...
With a similar mechanism of action to duloxetine, methadone has rationale for treating neuropathic pain. This study is a retrospective chart review to evaluate the outcomes of using methadone for CIPN pain. Out of 31 patients, 65% felt that methadone was an effective treatment, 19% felt that it was ineffective, and 16% felt that it was ...
The country begins a new week on edge after anti-immigrant riots, fanned by disinformation from the far right, broke out in cities across Britain. By The New York Times After a weekend of violent ...
UF Health, the health system for the University of Florida, has paused its plans to be part of a new hospital proposed in Palm Beach Gardens, but Jupiter Medical Center plans to move forward with ...
Self and professional referrals are welcome. We also accept transfers from other methadone programs. If you have any questions or would like to make an appointment, please call (718) 470-8950. The Methadone Maintenance Treatment Program (MMTP) provides voluntary, long-term pharmacological treatment to those struggling with opioid addiction.
COLUMBIA, S.C. - Governor Henry McMaster today issued Executive Order 2024-16, declaring a State of Emergency in preparation for the potential effects of Tropical Storm Debby, and asks South Carolinians to monitor local forecasts and to begin taking proper precautions.The executive order activates the South Carolina Emergency Operations Plan and enables all state agencies to coordinate ...
At the Daytona Beach Methadone Treatment Center, clients spend about $100 a week to get their daily dose of methadone. Buprenorphine, a newer maintenance drug sold under the brand name Suboxone ...
There are two operating methadone clinics in Louisville — one run by the Metro Health Department on 15th Street and a privately operated site, the Center for Behavioral Health, in St. Matthews.