Module 9: Substance-Related and Addictive Disorders
Case studies: substance-abuse disorders, learning objectives.
- Identify substance abuse disorders in case studies

Case Study: Benny
The following story comes from Benny, a 28-year-old living in the Metro Detroit area, USA. Read through the interview as he recounts his experiences dealing with addiction and recovery.
Q : How long have you been in recovery?
Benny : I have been in recovery for nine years. My sobriety date is April 21, 2010.
Q: What can you tell us about the last months/years of your drinking before you gave up?
Benny : To sum it up, it was a living hell. Every day I would wake up and promise myself I would not drink that day and by the evening I was intoxicated once again. I was a hardcore drug user and excessively taking ADHD medication such as Adderall, Vyvance, and Ritalin. I would abuse pills throughout the day and take sedatives at night, whether it was alcohol or a benzodiazepine. During the last month of my drinking, I was detached from reality, friends, and family, but also myself. I was isolated in my dark, cold, dorm room and suffered from extreme paranoia for weeks. I gave up going to school and the only person I was in contact with was my drug dealer.
Q : What was the final straw that led you to get sober?
Benny : I had been to drug rehab before and always relapsed afterwards. There were many situations that I can consider the final straw that led me to sobriety. However, the most notable was on an overcast, chilly October day. I was on an Adderall bender. I didn’t rest or sleep for five days. One morning I took a handful of Adderall in an effort to take the pain of addiction away. I knew it wouldn’t, but I was seeking any sort of relief. The damage this dosage caused to my brain led to a drug-induced psychosis. I was having small hallucinations here and there from the chemicals and a lack of sleep, but this time was different. I was in my own reality and my heart was racing. I had an awful reaction. The hallucinations got so real and my heart rate was beyond thumping. That day I ended up in the psych ward with very little recollection of how I ended up there. I had never been so afraid in my life. I could have died and that was enough for me to want to change.
Q : How was it for you in the early days? What was most difficult?
Benny : I had a different experience than most do in early sobriety. I was stuck in a drug-induced psychosis for the first four months of sobriety. My life was consumed by Alcoholics Anonymous meetings every day and sometimes two a day. I found guidance, friendship, and strength through these meetings. To say early sobriety was fun and easy would be a lie. However, I did learn it was possible to live a life without the use of drugs and alcohol. I also learned how to have fun once again. The most difficult part about early sobriety was dealing with my emotions. Since I started using drugs and alcohol that is what I used to deal with my emotions. If I was happy I used, if I was sad I used, if I was anxious I used, and if I couldn’t handle a situation I used. Now that the drinking and drugs were out of my life, I had to find new ways to cope with my emotions. It was also very hard leaving my old friends in the past.
Q : What reaction did you get from family and friends when you started getting sober?
Benny : My family and close friends were very supportive of me while getting sober. Everyone close to me knew I had a problem and were more than grateful when I started recovery. At first they were very skeptical because of my history of relapsing after treatment. But once they realized I was serious this time around, I received nothing but loving support from everyone close to me. My mother was especially helpful as she stopped enabling my behavior and sought help through Alcoholics Anonymous. I have amazing relationships with everyone close to me in my life today.
Q : Have you ever experienced a relapse?
Benny : I experienced many relapses before actually surrendering. I was constantly in trouble as a teenager and tried quitting many times on my own. This always resulted in me going back to the drugs or alcohol. My first experience with trying to become sober, I was 15 years old. I failed and did not get sober until I was 19. Each time I relapsed my addiction got worse and worse. Each time I gave away my sobriety, the alcohol refunded my misery.
Q : How long did it take for things to start to calm down for you emotionally and physically?
Benny : Getting over the physical pain was less of a challenge. It only lasted a few weeks. The emotional pain took a long time to heal from. It wasn’t until at least six months into my sobriety that my emotions calmed down. I was so used to being numb all the time that when I was confronted by my emotions, I often freaked out and didn’t know how to handle it. However, after working through the 12 steps of AA, I quickly learned how to deal with my emotions without the aid of drugs or alcohol.
Q : How hard was it getting used to socializing sober?
Benny : It was very hard in the beginning. I had very low self-esteem and had an extremely hard time looking anyone in the eyes. But after practice, building up my self-esteem and going to AA meetings, I quickly learned how to socialize. I have always been a social person, so after building some confidence I had no issue at all. I went back to school right after I left drug rehab and got a degree in communications. Upon taking many communication classes, I became very comfortable socializing in any situation.
Q : Was there anything surprising that you learned about yourself when you stopped drinking?
Benny : There are surprises all the time. At first it was simple things, such as the ability to make people smile. Simple gifts in life such as cracking a joke to make someone laugh when they are having a bad day. I was surprised at the fact that people actually liked me when I wasn’t intoxicated. I used to think people only liked being around me because I was the life of the party or someone they could go to and score drugs from. But after gaining experience in sobriety, I learned that people actually enjoyed my company and I wasn’t the “prick” I thought I was. The most surprising thing I learned about myself is that I can do anything as long as I am sober and I have sufficient reason to do it.
Q : How did your life change?
Benny : I could write a book to fully answer this question. My life is 100 times different than it was nine years ago. I went from being a lonely drug addict with virtually no goals, no aspirations, no friends, and no family to a productive member of society. When I was using drugs, I honestly didn’t think I would make it past the age of 21. Now, I am 28, working a dream job sharing my experience to inspire others, and constantly growing. Nine years ago I was a hopeless, miserable human being. Now, I consider myself an inspiration to others who are struggling with addiction.
Q : What are the main benefits that emerged for you from getting sober?
Benny : There are so many benefits of being sober. The most important one is the fact that no matter what happens, I am experiencing everything with a clear mind. I live every day to the fullest and understand that every day I am sober is a miracle. The benefits of sobriety are endless. People respect me today and can count on me today. I grew up in sobriety and learned a level of maturity that I would have never experienced while using. I don’t have to rely on anyone or anything to make me happy. One of the greatest benefits from sobriety is that I no longer live in fear.
Case Study: Lorrie

Figure 1. Lorrie.
Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and “popping pills” at the age of 13, and within the following decade, someone introduced her to cocaine and heroin. She lived with family and occasional boyfriends, and as she puts it, “I had no real home or belongings of my own.”
Before the age of 30, she was trying to survive as a heroin addict. She roamed from job to job, using whatever money she made to buy drugs. She occasionally tried support groups, but they did not work for her. By the time she was in her mid-forties, she was severely depressed and felt trapped and hopeless. “I was really tired.” About that time, she fell in love with a man who also struggled with drugs.
They both knew they needed help, but weren’t sure what to do. Her boyfriend was a military veteran so he courageously sought help with the VA. It was a stroke of luck that then connected Lorrie to friends who showed her an ad in the city paper, highlighting a research study at the National Institute of Drug Abuse (NIDA), part of the National Institutes of Health (NIH.) Lorrie made the call, visited the treatment intake center adjacent to the Johns Hopkins Bayview Medical Center, and qualified for the study.
“On the first day, they gave me some medication. I went home and did what addicts do—I tried to find a bag of heroin. I took it, but felt no effect.” The medication had stopped her from feeling it. “I thought—well that was a waste of money.” Lorrie says she has never taken another drug since. Drug treatment, of course is not quite that simple, but for Lorrie, the medication helped her resist drugs during a nine-month treatment cycle that included weekly counseling as well as small cash incentives for clean urine samples.
To help with heroin cravings, every day Lorrie was given the medication buprenorphine in addition to a new drug. The experimental part of the study was to test if a medication called clonidine, sometimes prescribed to help withdrawal symptoms, would also help prevent stress-induced relapse. Half of the patients received daily buprenorphine plus daily clonidine, and half received daily buprenorphine plus a daily placebo. To this day, Lorrie does not know which one she received, but she is deeply grateful that her involvement in the study worked for her.
The study results? Clonidine worked as the NIDA investigators had hoped.
“Before I was clean, I was so uncertain of myself and I was always depressed about things. Now I am confident in life, I speak my opinion, and I am productive. I cry tears of joy, not tears of sadness,” she says. Lorrie is now eight years drug free. And her boyfriend? His treatment at the VA was also effective, and they are now married. “I now feel joy at little things, like spending time with my husband or my niece, or I look around and see that I have my own apartment, my own car, even my own pots and pans. Sounds silly, but I never thought that would be possible. I feel so happy and so blessed, thanks to the wonderful research team at NIDA.”
- Liquor store. Authored by : Fletcher6. Located at : https://commons.wikimedia.org/wiki/File:The_Bunghole_Liquor_Store.jpg . License : CC BY-SA: Attribution-ShareAlike
- Benny Story. Provided by : Living Sober. Located at : https://livingsober.org.nz/sober-story-benny/ . License : CC BY: Attribution
- One patientu2019s story: NIDA clinical trials bring a new life to a woman struggling with opioid addiction. Provided by : NIH. Located at : https://www.drugabuse.gov/drug-topics/treatment/one-patients-story-nida-clinical-trials-bring-new-life-to-woman-struggling-opioid-addiction . License : Public Domain: No Known Copyright

Masks Strongly Recommended but Not Required in Maryland
Respiratory viruses continue to circulate in Maryland, so masking remains strongly recommended when you visit Johns Hopkins Medicine clinical locations in Maryland. To protect your loved one, please do not visit if you are sick or have a COVID-19 positive test result. Get more resources on masking and COVID-19 precautions .
- Vaccines
- Masking Guidelines
- Visitor Guidelines
News & Publications
New research and insights into substance use disorder.
Addictions to alcohol, illicit drugs and other substances remain a serious threat: According to the National Center for Health Statistics, part of the Centers for Disease Control and Prevention, from April 2020 to April 2021, nearly 92,000 people in the U.S. fatally overdosed on drugs — the single highest reported death toll during a 12-month period. The National Center for Drug Abuse Statistics has deemed the situation “a public health emergency.” All groups ages 15 and older experienced a rise in these grim statistics, intensified by the use of fentanyl.
Currently, substance use disorder affects more than 20 million Americans ages 12 and over. These numbers are troubling, says Johns Hopkins neuroscientist and addiction researcher Andrew Huhn , “but with a multifaceted approach, people with substance use disorders can recover.”
Drawing from his background in neuroscience and behavioral pharmacology, Huhn identifies risk factors for relapse and medication strategies — bolstered by supervised withdrawal and counseling — to improve treatment outcomes. “My research focuses on understanding the human experience of substance use disorder,” he says, noting that medications for opioid overdose, withdrawal and addiction “are safe, effective and continue to save lives.”
Now, thanks to a recent collaboration with Ashley Addiction Treatment, a residential treatment center in Havre de Grace, Maryland, Huhn, Kelly Dunn and colleagues are combining efforts to identify patients likely to benefit from supervised withdrawal or opioid maintenance therapy. The goal is to expand treatment options to improve health care for people with the condition. “Relapse remains common, but a subset of patients have done well,” says Dunn.
Concurrently, Huhn, Dunn and colleagues are building a research database based on the Trac9 program, which charts patients’ progress in real-time through technology, such as a tablet or phone — as well as alerting clinicians to a relapse and the need for intervention. They are also using wearable devices to monitor sleep and cardiovascular outcomes, and a smart phone application to track each time a patient notes having successfully ignored a craving for alcohol or a drug. Much of this research takes place at Behavioral Pharmacology Research Unit , located on the Johns Hopkins Bayview Medical Center campus.
Their published work includes studies showing a greater need for treatment of older adults with alcohol and opioid use disorders. Two additional studies have garnered national attention, both on how fentanyl use affects the treatment of opioid use disorder . Much of the illicit opioid supply in the U.S. is mixed with fentanyl, leading to a recent surge in fentanyl-related overdose deaths.
Yet another study showed promise in the use of a sleep medication to improve opioid withdrawal outcomes. Researchers in Huhn’s lab continue to glean insights from neuroimaging, ambulatory monitoring in real time, and repeated measures of behaviors.
Greg Hobelmann , the CEO of Ashley, who trained at Johns Hopkins and is a part-time faculty member, chairs an elective at the Ashley facility in addictions psychiatry. He, along with Eric Strain and Huhn are building infrastructure that includes intake data on every patient, as well as outcomes data when people complete the Ashley program — and for the year that follows. Biospecimens will also be included in the project, for studies in areas such as genetics.
“The biggest and most exciting thing is being able to create predictive models of relapse risk and then create strategies to improve those outcomes,” says Huhn. Jimmy Potash , director of the Johns Hopkins Department of Psychiatry and Behavioral Sciences couldn’t agree more. “This will be a powerful platform for discovery of better approaches to treating addiction,” he says. “I’m eager to see it — and our relationship with Ashley Addiction — move forward.”
Despite enduring challenges in addictions psychiatry, Huhn is hopeful. “We have the ability to continue collecting data and to test hypotheses,” he says. “It’s the kind of stuff we hope will turn into a game-changer, similar to what has happened in cancer and heart disease treatments. We build research into the treatment and let that guide our approach to care.”
Learn about a web-based education intervention to reduce opioid overdose, Low-Cost Intervention Reduces Risk of Opioid Overdose.
Related Reading
Johns hopkins bayview’s center for addiction and pregnancy supports new mothers and their babies in the fight against substance use disorders.
Center offers judgment-free care, helping moms and newborns


- Liberty University
- Jerry Falwell Library
- Special Collections
- < Previous
Home > ETD > Doctoral > 6036
Doctoral Dissertations and Projects
Success treating substance use disorder: a case study of minnesota adult and teen challenge.
John Joseph Lenss , Liberty University Follow
Rawlings School of Divinity
Doctor of Philosophy
Rich Sironen
Substance use disorder, addiction recovery, treatment, long-term recovery, dropout, success rate
Disciplines
Leadership Studies | Social and Behavioral Sciences
Recommended Citation
Lenss, John Joseph, "Success Treating Substance Use Disorder: A Case Study of Minnesota Adult and Teen Challenge" (2024). Doctoral Dissertations and Projects . 6036. https://digitalcommons.liberty.edu/doctoral/6036
Minnesota Adult and Teen Challenge (MNTC) is an addiction treatment center. The reason for this qualitative case study was to discover why clients of substance use disorder treatment programs believe that they can graduate from their program when 50% of those who start the same long-term program drop out. This case study focused on graduates from MNTC in Minneapolis, Minnesota. This study discovered the graduates' common attributes that may improve MNTC treatment center programs, which could decrease the number of people who walk away from addiction recovery programs prematurely and increase the number of those who graduate. According to MNTC records and the literature, 50% of clients in long-term recovery programs at MNTC drop out and must start over in the program before they graduate. This case study documented graduates' opinions on why they successfully completed the long-term program for the Minneapolis, Minnesota Adult and Teen Challenge (MNTC). The definition of an MNTC graduate was graduating from the program and not having a relapse for one year. The theory guiding this study was Ajzen’s theory of planned behavior, which proposes that an individual's decision whether to engage in any specific behavior, such as drug or alcohol use, is predicated by their intention to engage in that behavior. Likewise, Ajzen’s theory can explain a person’s intention to stop substance use as a conscious behavior, which this study collected information to understand. The academic community—mainly those interested in addiction treatment and recovery programs—played a crucial role in this research, as their expertise and insights significantly contributed to understanding and improving addiction recovery programs.
Since September 19, 2024
Included in
Leadership Studies Commons
- Collections
- Faculty Expert Gallery
- Theses and Dissertations
- Conferences and Events
- Open Educational Resources (OER)
- Explore Disciplines
Advanced Search
- Notify me via email or RSS .
Faculty Authors
- Submit Research
- Expert Gallery Login
Student Authors
- Undergraduate Submissions
- Graduate Submissions
- Honors Submissions
Home | About | FAQ | My Account | Accessibility Statement
Privacy Copyright
Substance Use Disorders and Addiction: Mechanisms, Trends, and Treatment Implications
Information & authors, metrics & citations, view options, insights into mechanisms related to cocaine addiction using a novel imaging method for dopamine neurons, treatment implications of understanding brain function during early abstinence in patients with alcohol use disorder, relatively low amounts of alcohol intake during pregnancy are associated with subtle neurodevelopmental effects in preadolescent offspring, increased comorbidity between substance use and psychiatric disorders in sexual identity minorities, trends in nicotine use and dependence from 2001–2002 to 2012–2013, conclusions, information, published in.

- Substance-Related and Addictive Disorders
- Addiction Psychiatry
- Transgender (LGBT) Issues
Competing Interests
Export citations.
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download. For more information or tips please see 'Downloading to a citation manager' in the Help menu .
| Format | |
|---|---|
| Citation style | |
| Style | |
View options
Login options.
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Not a subscriber?
Subscribe Now / Learn More
PsychiatryOnline subscription options offer access to the DSM-5-TR ® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).
Share article link
Copying failed.
NEXT ARTICLE
Request username.
Can't sign in? Forgot your username? Enter your email address below and we will send you your username
If the address matches an existing account you will receive an email with instructions to retrieve your username
Create a new account
Change password, password changed successfully.
Your password has been changed
Reset password
Can't sign in? Forgot your password?
Enter your email address below and we will send you the reset instructions
If the address matches an existing account you will receive an email with instructions to reset your password.
Your Phone has been verified
As described within the American Psychiatric Association (APA)'s Privacy Policy and Terms of Use , this website utilizes cookies, including for the purpose of offering an optimal online experience and services tailored to your preferences. Please read the entire Privacy Policy and Terms of Use. By closing this message, browsing this website, continuing the navigation, or otherwise continuing to use the APA's websites, you confirm that you understand and accept the terms of the Privacy Policy and Terms of Use, including the utilization of cookies.
An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Header - Callout
In Crisis? Call or Text 988
Substance use, mental health challenges widespread in 2021
Data sources used.
- National Survey on Drug Use and Health 2021
- Open Access
- By Publication (A-Z)
- Case Reports
- Publication Ethics
- Publishing Policies
- Editorial Policies
- Submit Manuscript
- About Graphy

New to Graphy Publications? Create an account to get started today.
Registered Users
Have an account? Sign in now.

- Full-Text HTML
- Full-Text PDF
- About This Journal
- Aims & Scope
- Editorial Board
- Editorial Process
- Author Guidelines
- Special Issues
- Articles in Press

Jo-Hanna Ivers 1* and Kevin Ducray 2
In October 2012, 83 front-line Irish service providers working in the addiction treatment field received accreditation as trained practitioners in the delivery of a number of evidence-based positive reinforcement approaches that address substance use: 52 received accreditation in the Community Reinforcement Approach (CRA), 19 in the Adolescent Community Reinforcement Approach (ACRA) and 12 in Community Reinforcement and Family Training (CRAFT). This case study presents the treatment of a 17-year-old white male engaging in high-risk substance use. He presented for treatment as part of a court order. Treatment of the substance use involved 20 treatment sessions and was conducted per Adolescent Community Reinforcement Approach (A-CRA). This was a pilot of A-CRA a promising treatment approach adapted from the United States that had never been tried in an Irish context. A post-treatment assessment at 12-week follow-up revealed significant improvements. At both assessment and following treatment, clinician severity ratings on the Maudsley Addiction Profile (MAP) and the Alcohol Smoking and Substance Involvement Screening Test (ASSIST) found decreased score for substance use was the most clinically relevant and suggests that he had made significant changes. Also his MAP scores for parental conflict and drug dealing suggest that he had made significant changes in the relevant domains of personal and social functioning as well as in diminished engagement in criminal behaviour. Results from this case study were quite promising and suggested that A-CRA was culturally sensitive and applicable in an Irish context.
1. Theoretical and Research Basis for Treatment
Substance use disorders (SUDs) are distinct conditions characterized by recurrent maladaptive use of psychoactive substances associated with significant distress. These disorders are highly common with lifetime rates of substance use or dependence estimated at over 30% for alcohol and over 10% for other substances [1 , 2] . Changing substance use patterns and evolving psychosocial and pharmacologic treatments modalities have necessitated the need to substantiate both the efficacy and cost effectiveness of these interventions.
Evidence for the clinical application of cognitive behavioural therapy (CBT) for substance use disorders has grown significantly [3 - 8] . Moreover, CBT for substance use disorders has demonstrated efficacy both as a monotherapy and as part of combination treatment [7] . CBT is a time-limited, problem-focused, intervention that seeks to reduce emotional distress through the modification of maladaptive beliefs, assumptions, attitudes, and behaviours [9] . The underlying assumption of CBT is that learning processes play an imperative function in the development and maintenance of substance misuse. These same learning processes can be used to help patients modify and reduce their drug use [3] .
Drug misuse is viewed by CBT practitioners as learned behaviours acquired through experience [10] . If an individual uses alcohol or a substance to elicit (positively or negatively reinforced) desired states (e.g. euphorigenic, soothing, calming, tension reducing) on a recurrent basis, it may become the preferred way of achieving those effects, particularly in the absence of alternative ways of attaining those desired results. A primary task of treatment for problem substance users is to (1) identify the specific needs that alcohol and substances are being used to meet and (2) develop and reinforce skills that provide alternative ways of meeting those needs [10 , 11] .
CRA is a broad-spectrum cognitive behavioural programme for treating substance use and related problems by identifying the specific needs that alcohol and or other substances are satisfying or meeting. The goal is then to develop and reinforce skills that provide alternative ways of meeting those needs. Consistent with traditional CBT, CRA through exploration, allows the patient to identify negative thoughts, behaviours and beliefs that maintain addiction. By getting the patient to identify, positive non-drug using behaviours, interests, and activities, CRA attempts to provide alternatives to drug use. As therapy progresses the objective is to prevent relapse, increase wellness, and develop skills to promote and sustain well-being. The ultimate aim of CRA, as with CBT is to assist the patient to master a specific set of skills necessary to achieve their goals. Treatment is not complete until those skills are mastered and a reasonable degree of progress has been made toward attaining identified therapy goals. CRA sessions are highly collaborative, requiring the patient to engage in ‘between session tasks’ or homework designed reinforce learning, improve coping skills and enhance self efficacy in relevant domains.
The use of the Community Reinforcement Approach is empirically supported with inpatients [12 , 13] , outpatients [14 - 16] and homeless populations (Smith et al., 1998). In addition, three recent metaanalytic reviews cited CRA as one of the most cost-effective treatment programmes currently available [17 , 18] .
A-CRA is a evidenced based behavioural intervention that is an adapted version of the adult CRA programme [19] . Garner et al [19] modified several of the CRA procedures and accompanying treatment resources to make them more developmentally appropriate for adolescents. The main distinguishing aspect of A-CRA is that it involves caregivers—namely parents or guardians who are ultimately responsible for the adolescent and with whom the adolescent is living.
A-CRA has been tested and found effective in the context of outpatient continuing care following residential treatment [20 - 22] and without the caregiver components as an intervention for drug using, homeless adolescents [23] . More recently, Garner et al [19] collected data from 399 adolescents who participated in one of four randomly controlled trials of the A-CRA intervention, the purpose of which was to examine the extent to which exposure to A-CRA procedures mediated the relationship between treatment retention and outcomes. The authors found adolescents who were exposed to 12 or more A-CRA procedures were significantly more likely to be in recovery at follow-up.
Combining A-CRA with relapse prevention strategies receives strong support as an evidence based, best practice model and is widely employed in addiction treatment programmes. Providing a CBT-ACRA therapeutic approach is imperative as it develops alternative ways of meeting needs and thus altering dependence.
2. Case Introduction
Alan is a 17 year-old male currently living in County Dublin. Alan presented to the agency involuntarily and as a requisite of his Juvenile Liaison Officer who was seeing him on foot of prior drugs arrest for ‘possession with intent to supply’; a more serious charge than a simple ‘drugs possession’ charge. As Alan had no previous charges he was placed on probation for one year. This was Alan’s first contact with the treatment services. A diagnostic assessment was completed upon entry to treatment and included completion of a battery of instruments comprising the Maudsley Addiction Profile (MAP), The World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) and the Beck Youth Inventory (BYI) (see appendices for full description of outcome measures) (Table 1).

3. Diagnostic Criteria
The apparent symptoms of substance dependency were: (1) Loss of Control - Alan had made several attempts at controlling the amounts of cannabis he consumed, but those times when he was able to abstain from cannabis use were when he substituted alcohol and/or other drugs. (2) Family History of Alcohol/Drug Usage - Alan’s eldest sister who is now 23 years old is in recovery from opiate abuse. She was a chronic heroin user during her early adult years [17 - 21] . During this period, which corresponds to Alan’s early adolescent years [12 - 15] she lived in the family home (3) Changes in Tolerance - Alan began per day. At presentation he was smoking six to eight cannabis joints daily through the week, and eight to twelve joints daily on weekends.
4. Psychosocial, Medical and Family History
At time of intake Alan was living with both of his parents and a sister, two years his senior, in the family home. Alan was the youngest and the only boy in his family. He had two other older sisters, 5 and 7 years his senior. He was enrolled in his 5th year of secondary school but at the time of assessment was expelled from all classes. Alan had superior sporting abilities. He played for the junior team of a first division football team and had the prospect of a professional career in football. He reported a family history positive for substance use disorders. An older sister was in recovery for opiate dependence. Apart from his substance use Alan reported no significant psychological difficulties or medical problems. His motives for substance use were cited as boredom, curiosity, peer pressure, and pleasure seeking. His triggers for use were relationship difficulties at home, boredom and peer pressure. Pre-morbid personality traits included thrill seeking and impulsivity (Table 2).

5. Case Conceptualisation
A CBT case formulation is based on the cognitive model, which hypothesizes that "a person’s feelings and emotions are influenced by their perception of events" . It is not the actual event that determines how the person feels, but rather how they construe the event (Beck, 1995 p14). Moreover, cognitive theory posits that the “child learns to construe reality through his or her early experiences with the environment, especially with significant others” and that “sometimes these early experiences lead children to accept attitudes and beliefs that will later prove maladaptive” [24] . A CBT formulation (or case conceptualisation) is one of the key underpinnings of Cognitive Behavioural Therapy (CBT). It is the ‘blueprint’ which aids the therapist to understand and explain the patient’s’ problems.
Formulation driven CBT enables the therapist to develop an individualised understanding of the patient and can help to predict the difficulties that a patient may encounter during therapy. In Alan’s case, exploring his existing negative automatic thoughts about regarding school and his academic competences highlighted the difficulties he could experience with CBT homework completion. Whilst Alan was good at between session therapy assignments, an exploration of what is meant by ‘homework’ in a CBT context was crucial.
A collaborative CBT formulation was done diagrammatically together with Alan (Figure 1). This formulation aimed to describe his presenting problems and using CBT theory, to explore explanatory inferences about the initiating and maintaining factors of his drug use which could practically inform meaningful interventions.

Simmons and Griffiths et al. make the insightful observation that particular group differences need to be specifically considered and suggest that the therapist should be cognizant of the role of both society and culture when developing a formulation. They firstly suggest that the impact played by gender, sexuality and socio-cultural roles in the genesis of a psychological disorder, namely the contribution that being a member of a group may have on predisposing and precipitating factors, be carefully considered. An example they offer is the role of poverty on the development of psychological problems, such as the link evidenced between socio economic group and onset of schizophrenia. This was clearly evident in the case of Alan, who being a member of a deprived socioeconomic group, growing up and living in an area with a high level of economic deprivation, perceived that his choices for success were limited. His thinking, as an adolescent boy, was dichotomous in that he saw himself as having only two fixed and limited choices (a) being good at sport he either pursue a career as a professional sportsman or alternatively (b) he engage in crime and work his way up through the ranks as a ‘career criminal’. Simmons & Griffiths secondly suggest that being a member of a particular group can heavily influence a person’s understanding of the causality of their psychological disorder. A third consideration when developing a formulation is the degree to which being a member of a particular group may influence the acceptance or rejection of a member experiencing a psychological illness. Again this is pertinent in Alan’s case as he was part of a sub-group, a gang engaged in crime. For this cohort, crime and drug use were synonymous. Using drugs was viewed as a rite of passage for Alan.
Drug use, according to CBT models, are socially learned behaviours initiated, maintained and altered through the dynamic interaction of triggers, cues, reinforcers, cognitions and environmental factors. The application of a such a formulation, sensitive to Simmons and Griffiths (2009) aforementioned observations, proved useful in affording insights into the contextual and maintaining factors of Alan’s drug use which was heavily influenced by the availability of drugs ,his peer group (with whom he spent long periods of time) and their petty drug dealing and criminality. Similarly, engaging with his football team mates during the lead up to an important match significantly reduced his drug use and at certain times of the year even lead to abstinence. Sharing this formulation allowed him to note how his drug use patterns were driven, as per the CBT paradigm, by modifiable external, transient, and specific factors (e.g. cues, reinforcements, social networks and related expectations and social pressures).
Employing the A-CRA model allowed for this tailored fit as A-CRA specifically encourages the patient to identify their own need and desire for change. Alan identified the specific needs that were met by using substances and he developed and reinforced skills that provided him with alternative ways of meeting those needs. This model worked extremely well for Alan as he had identified and had ready access to a pro- social ‘alternative group’ or community. As he had had access to an alternative positive peer group and another activity (sport) which he was ‘really good at’, he simply needed to see the evidence of how his context could radically affect his substance use; more specifically how his beliefs, thinking and actions in certain circumstances produced very different drug use consequences and outcomes.
6. Course of Treatment and Assessment of Progress
One focus of CBT treatment is on teaching and practising specific helpful behaviours, whilst trying to limit cognitive demands on clients. Repetition is central to the learning process in order to develop proficiency and to ensure that newly acquired behaviours will be available when needed. Therefore, behavioural using rehearsal will emphasize varied, realistic case examples to enhance generalization to real life settings. During practice periods and exercises, patients are asked to identify signals that indicate high-risk situations, demonstrating their understanding of when to use newly acquired coping skills. CBT is designed to remedy possible deficits in coping skills by better managing those identified antecedents to substance use. Individuals who rely primarily on substances to cope have little choice but to resort to substance use when the need to cope arises. Understanding, anticipating and avoiding high risk drug use scenarios or the “early warning signals” of imminent drug use is a key CBT clinical activity.
A major goal of a CBT/A-CRA therapeutic approach is to provide a range of basic alternative skills to cope with situations that might otherwise lead to substance use. As ‘skill deficits’ are viewed as fundamental to the drug use trajectory or relapse process, an emphasis is placed on the development and practice of coping skills. A-CRA was manualised in 2001 as part of the Cannabis Youth Treatment Series (CYT) and was tested in that study [21] and more recently with homeless youth [23] . It was also adapted for use in a manual for Assertive Continuing Care following residential treatment [20] .
There are twelve standard and three optional procedures proposed in the A-CRA model. The delivery of the intervention is flexible and based on individual adolescent needs, though the manual provides some general guidelines regarding the general order of procedures. Optional procedures are ‘Dealing with Failure to Attend’, ‘Job-Seeking Skills’, and ‘Anger Management’. Standard procedures are included in table 3 below. For a more detailed description of sessions and procedures please see appendices.

Smith and Myers describe the theoretical underpinnings of CRA as a comprehensive behavioural program for treating substance-abuse problems. It is based on the belief that environmental contingencies can play a powerful role in encouraging or discouraging drinking or drug use. Consequently, it utilizes social, recreational, familial, and vocational reinforcers to assist consumers in the recovery process. Its goal is to essentially make a sober lifestyle more rewarding than the use of substances. Interestingly the authors note: ‘Oddly enough, however, while virtually every review of alcohol and drug treatment outcome research lists CRA among approaches with the strongest scientific evidence of efficacy, very few clinicians who treat consumers with addictions are familiar with it’. ‘The overall philosophy is to promote community based rewarding of non drug-using behaviour so that the patient makes healthy lifestyle changes’ p.3 [25] .
A-CRA procedures use ‘operant techniques and skills training activities’ to educate patients and present alternative ways of dealing with challenges without substances. Traditionally, CRA is provided in an individual, context-specific approach that focuses on the interaction between individuals and those in their environments. A-CRA therapists teach adolescents when and where to use the techniques, given the reality of each individual’s social environment. This tailored approach is facilitated by conducting a ‘functional analysis’ of the adolescent’s behaviour at the beginning of therapy so they can better understand and interrupt the links in the behavioural chain typically leading to episodes of drug use. A-CRA therapists then teach individuals how to improve communication and other skills, build on their reinforcers for abstinence and use existing community resources that will support positive change and constructive support systems.
A-CRA emphasises lapse and relapse prevention. Relapseprevention cognitive behavioural therapy (RP-CBT) is derived from a cognitive model of drug misuse. The emphasis is on identifying and modifying irrational thoughts, managing negative mood and intervening after a lapse to prevent a full-blown relapse [26] . The emphasis is on development of skills to (a) recognize High Risk Situations (HRS) or states where clients are most vulnerable to drug use, (b) avoidance of HRS, and (C) to use a variety of cognitive and behavioural strategies to cope effectively with these situations. RPCBT differs from typical CBT in that the accent is on training people who misuse drugs to develop skills to identify and anticipate situations or states where they are most vulnerable to drug use and to use a range of cognitive and behavioural strategies to cope effectively with these situations [26] .
7. Access and Barriers to Care
Alan engaged with the service for eight months. During this time he received twenty sessions, three of which were assessment focused, the remaining seventeen sessions were A-CRA focused; two of the seventeen involved his mother, the remaining fifteen were individual. As Alan was referred by the probation services, he was initially somewhat ambivalent about drug use focussed interventions. His early motivation for engagement was primarily to avoid the possibility of a custodial sentence.
8. Treatment
My sessions with Alan were guided by the principles of A-CRA [27] which focuses on coping skills training and relapse prevention approaches to the treatment of addictive disorders. Prior to engaging with Alan, I had completed the training course and commenced the A-CRA accreditation process, both under the stewardship of Dr Bob Meyers, whose training and publication offers detailed guidelines on skills training and relapse prevention with young people in a similar context [27] .
During the early part of each session I focused on getting a clear understanding of Alan’s current concerns, his general level of functioning, his substance abuse and pattern of craving during the past week. His experiences with therapy homework, the primary focus being on what insight he gained by completing such exercises was also explored. I spent considerable time engaged in a detailed review of Alan’s experience with the implementation of homework tasks during which the following themes were reviewed:
-Gauging whether drug use cessation was easier or harder than he anticipated? -Which, if any, of the coping strategies worked best? -Which strategies did not work as well as expected. Did he develop any new strategies? -Conveying the importance of skills practice, emphasising how we both gained greater insights into how cognitions influenced his behaviour. After developing a clear sense of Alan’s general functioning, current concerns and progress with homework implementation, I initiated the session topic for that week. I linked the relevance of the session topic to Alan’s current cannabis-related concerns and introduced the topic by using concrete examples from Alan’s recent experience. While reviewing the material, I repeatedly ensured that Alan understood the topic by asking for concrete examples, while also eliciting Alan’s views on how he might use these particular skills in the future.
Godley & Meyers [21] propose a homework exercise to accompany each session. An advantage of using these homework sheets is that they also summarise key points about each topic and therefore serve as a useful reminder to the patient of the material discussed each week. Meyers, et al. (2011) suggests that rather than being bound by the suggested exercises in the manualised approach, they may be used as a starting point for discussing the best way to implement the required skill and to develop individualised variations for new assignments [27] . The final part of each session focused on Alan’s plan for the week ahead and any anticipated high-risk situations. I endeavoured to model the idea that patients can literally ‘plan themselves out of using’ cannabis or other drugs. For each anticipated high-risk situation, we identified appropriate and viable coping skills. Better understanding, anticipating and planning for high-risk situations was difficult in the beginning of treatment as Alan was not particularly used to planning or thinking through his activities. For a patient like Alan, whose home life is often chaotic, this helped promote a growing sense of self efficacy. Similarly, as Alan had been heavily involved with drug use for a long time, he discovered through this process that he had few meaningful activities to fill his time or serve as alternatives to drug use. This provided me with an opportunity to discuss strategies to rebuild an activity schedule and a social network.
During our sessions, several skill topics were covered. I carefully selected skills to match Alan’s needs. I selected coping skills that he has used in the past and introduced one or two more that were consistent with his cognitive style. Alan’s cognitive score indicated a cognitive approach reflecting poor problem solving or planning. Sessions focused on generic skills including interpersonal skills, goal setting, coping with criticism or anger, problem solving and planning. The goal was to teach Alan how to build on his pro- social reinforcers, how to use existing community resources supportive of positive change and how to develop a positive support system.
The sequence in which these topics were presented was based on (a) patient needs and (b) clinician judgment (a full description of individual sessions may be found in appendices).
A-CRA procedures use ‘operant techniques and skills training activities’ to educate patients and present alternative ways of dealing with challenges without substances. Traditionally, CRA is provided in an individual, context-specific approach that focuses on the interaction between individuals and those in their environments. A-CRA therapists teach adolescents when and where to use the techniques, given the reality of each individual’s social environment.
9. Assessment of Treatment Outcome
A baseline diagnostic assessment of outcomes was completed upon treatment entry. This assessment consisted of a battery of psychological instruments including (see appendices for full a description of assessment measures):
-The Maudsley Addiction Profile (MAP). -The Beck Youth Inventories. -The World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST).
In addition to the above, objective feedback on Alan’s clinical and drug use status through urine toxicology screens was an important part of his drug treatment. Urine specimens were collected before each session and available for the following session. The use of toxicology reports throughout treatment are considered a valuable clinical tool. This part of the session presents a good opportunity to review the results of the most recent urine toxicology screen and promote meaningful therapeutic activities in the context of the patient’s treatment goals [28] .
In reporting on substance use since the last session, patients are likely to reveal a great deal about their general level of functioning and the types of issues and problems of most current concern. This allows the clinician to gauge if the patient has made progress in reducing drug use, his current level of motivation, whether there is a reasonable level of support available in efforts to remain abstinent and what is currently bothering him. Functional analyses are opportunistically used throughout treatment as needed. For example, if cannabis use occurs, patients are encouraged to analyse antecedent events so as to determine how to avoid using in similar situations in the future. The purpose is to help the patient understand the trajectory and modifiable contextual factors associated with drug use, challenge unhelpful positive drug use expectancies, identify possible skills deficiencies as well as seeking functionally equivalent non- drug using behaviours so as to reduce the probability of future drug use. The approach I used is based on the work of [28] .
The Functional Analysis was used to identify a number of factors occurring within a relatively brief time frame that influenced the occurrence of problem behaviours. It was used as an initial screening tool as part of a comprehensive functional assessment or analysis of problem behaviour. The results of the functional analysis then served as a basis for conducting direct observations in a number of different contexts to attest to likely behavioural functions, clarify ambiguous functions, and identify other relevant factors that are maintaining the behaviour.
The Happiness Scale rates the adolescent’s feelings about several critical areas of life. It helps therapists and adolescents identify areas of life that adolescents feel happy about and alternatively areas in which they have problems or challenges. Most importantly it identifies potential treatment goals subjectively meaningful to the patient, facilitates positive behaviour change in a range of life domains as well as help clients track their progress during treatment.
Alan’s BYI score (Table 4) indicates that at the time of assessment he was within the average scoring range on ‘self-concept’, and moderately elevated in the areas of ‘depression’, ‘anxiety’, and ‘disruptive behaviour’. His score for ‘anger’ suggested that his anger fell within the extremely elevated range. When this was discussed with Alan he agreed that this was quite accurate. Anger, and in particular controlling his anger, was subjectively identified as a treatment goal.

10. Follow-up
Given that follow-up occurred by telephone it was not feasible to administer the full battery of tests. With Alan’s treatment goals in mind it was decided to administer the MAP and ASSIST. Table 5 below illustrates Alan’s score at baseline and follow-up for the MAP and ASSIST. For summary purposes I have taken areas for concern at baseline for both instruments.

Alan’s score for cannabis was the most clinically relevant as it placed him in the 'high risk’ domain while his alcohol score indicated that he had engaged in binge drinking (6+ drinks) at T1. However, at T2 Alan’s score suggests that he had made considerable reductions in the use of both substances. Also his MAP scores for parental conflict and drug dealing suggest that he had also made major positive changes in the relevant domains of personal and social functioning as well as ceasing criminal behaviour.
At 3 months post-discharge I contacted Alan by phone. He had maintained and continued to further his progress. His drug use was at a minimal level (1 or 2 shared joints per month). He was no longer engaged in crime and his probationary period with the judicial system had passed. He had received a caution for his earlier drugs charge. At the time of follow-up he was enjoying participating in a Sports Coaching course and was excelling with his study assignments. Relationships had improved considerably with his mother and sister and he had re-engaged with a previous, positive, peer group linked to his involvement with the GAA . Overall he felt he was doing extremely well.
11. Complicating Factors with A-CRA Model
There are many challenges that may arise in the treatment of substance use disorders that can serve as barriers to successful treatment. These include acute or chronic cognitive deficits, health problems, social stressors and a lack of social resources [7] . Among individuals presenting with substance use there are often other significant life challenges including early school leaving, family conflicts, legal issues, poor or deviant social networks, etc. A particular challenge with Alan’s case was the social and environmental milieu which he shared with his drug using peers. For Alan, who initially had few skills and resources, engaging in treatment meant not only being asked to change his overall way of life but also to renounce some of those components in which he enjoyed a sense of belonging, particularly as he had invested significantly in these friendships. A sense of ‘belonging to the substance use culture’ can increase ambivalence for change [7] . Alan’s mother strongly disapproved of his drug using peer group and failed to acknowledge Alan’s perceived loss. This resulted in mother- son conflict. The use of the caregiver session allowed an exploration of perceived ‘losses’ relative to the ‘gains’ associated with Alan’s abstinence. It was moreover seen to be critical to establish alternatives for achieving a sense of belonging, including both his social connection and his social effectiveness. Alan’s sports ability allowed for this to be fostered. He is a talented sportsman which often meant his acceptance within a team or group is a given.
Despite the positive effects of A-CRA it is not without its shortcomings. The approach is at times quite American- oriented, particularly around identifying local resources and its focus on culturally specific outlets in promoting social engagement as alternatives to substance use. While this is supported in the literature, it may not necessarily be transferable to certain Irish adolescent contexts or subcultures.
12. Treatment Implications of the Case
A-CRA captures a broad range of behavioural treatments including those targeting operant learning processes, motivational barriers to improvement and other more traditional elements of cognitivebehavioural interventions. Overall, this intervention has demonstrated efficacy. Despite this heterogeneity, core elements emerge based in a conceptual model of SUDs as disorders characterized by learning processes and driven by the strongly reinforcing effects of the substances of abuse. There is rich evidence in the substance use disorders literature that improvement achieved by CBT (7) and indeed A-CRA (Godley et al. and Garner et al. [22 , 20] ) generalizes to all areas of functioning, including social, work, family and marital adjustment domains. The present study’s finding that a reduction in substance-related symptoms was accompanied by improved levels of functioning, social adjustment and enhanced quality of life, provides further support for this point.
In conclusion, there is some preliminary evidence that A-CRA is a promising treatment in the rehabilitation of adolescent substance users in Ireland and culturally similar societies. Clearly, results from a case study have limited generalisability and there is need for larger controlled studies providing robust outcomes to confirm the efficacy of A-CRA in an Irish context. A more systematic study of this issue is in the interest of adolescent substance users and the health services providers faced with the challenge of providing affordable, evidencebased mental health and addiction care to young people.
13. Recommendations to Clinicians and Students
The ACRA model is a structured assemblage of a range of cognitive and behavioural activities (e.g. a rationale and overview of the paradigm, sobriety sampling, functional analyses, communication skills, problem solving skills, refusal skills, jobs counselling, anger management and relapse prevention) which are shared in varying degrees with other CBT approaches. The ACRA model has the advantage of established effectiveness. A foundation in empirical research together with its manual- supported approach results in it being an appropriate “off the shelf ” intervention, highly applicable to many adolescent substance misusers. Such a focussed approach also has the advantage of limiting therapist “drift”. Notwithstanding the accessible manual and other resources available on- line, clinicians and students are strongly encouraged to undergo accredited ACRA training and supervision.
Unfortunately such a structured model, despite its many advantages, does have limitations. This model may not meet the sum of all drug misusing adolescent service user treatment needs, nor is it applicable to all adolescent drug users, particularly highly chaotic individuals with high levels of co- morbidities or multi-morbidities as often found in this population [29 , 30] . Whilst focussing on specifically on drug use, ACRA does not directly address co-existing problem behaviours or challenges such as depression, anxiety, personality disorder, or post traumatic stress disorder (PTSD) synergistically linked to drug use. It is possible that given the high levels of dual diagnoses encountered in this population as well as the compounding effect that drug use exerts on multiple systems, clinicians and practitioners may find a strict application of the ACRA model limiting, necessitating the application of an additional range or layer of psychotherapeutic competencies? Additionally the ACRA model does not focus explicitly on other psychological activities useful in the treatment of drug misuse such as the control and management of unhelpful cognitive styles or habits; breathing or progressive relaxation skills; anger management; imagery, visualisation and mindfulness. That is, as a manual based approach comprising a number of fixed components, a major potential challenge facing clinicians and students is the tension they may experience between maintaining strict fidelity to a pure ACRA approach, versus the flexibility l approved by more formulation driven CBT approaches?
The advantages of a skilled application of a formulation driven approach which are cited and summarised in are multiple and include the collaborative nature of goal setting, the facilitation of problem prioritisation in a meaningful and useful manner; a more immediate direction and structuring of the course of treatment; the provision of a rationale for the most fitting intervention point or spotlight for the treatment; an integration of seemingly unrelated or dissimilar difficulties in a meaningful yet parsimonious fashion; an influence on the choice of procedures and “homework” exercises; theory based mechanisms to understand the dynamics of the therapeutic relationship and a sense of targeted and ‘extra-therapeutic’ issues and how they could be best explained and managed, especially in terms of precipitators or triggers, core beliefs, assumptions and automatic thoughts.
Thus given the above observations and together with the importance placed on engagement and retention, the high variability in the cognitive, emotional, social and developmental domains [4] differences in roles (e.g. teenagers who are also parents) and levels of autonomy as well as high degrees of dual diagnosis or co- morbidities found in this group [29 , 30] practitioners are encouraged to also develop competencies in allied psychological treatment models such as Motivational Interviewing [31] ; familiarity with the core principles of CBT, disorder specific and problem-specific CBT competences, the generic and meta- competences of CBT as well as an advanced knowledge and understanding of mental health problems that will provide practitioners with the confidence and capacity to implement treatment models in a more flexible yet coherent manner,. In addition to seeking supervision and mentorship students and practitioners are directed, as a starting point, to University College London’s excellent resources outlining the competencies required to provide a more comprehensive interventions [11] .
Both authors reported no conflict of interest in the content of this paper.
Author Contributions
Conceived and designed the experiments: JI. Recruitment & assessment and on going treatment t of patient JI. On going supervision of case KD. Contributed reagents/materials/analysis tools: JI, & KD. Wrote the paper: JI. Contributed to final draft paper KD.
Acknowledgments
We thank Adolescent Addiction Services, Health Service Executive.
- Compton WM, Thomas YF, Stinson FS, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry 64: 566-576. View
- Hasin DS, Stinson FS, Ogburn E, Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry 64: 830-842. View
- Carroll KM, Nich C, Ball SA, McCance E, Frankforter TL, et al. (2000) Oneyear follow-up of disulfiram and psychotherapy for cocaine-alcohol users: sustained effects of treatment. Addiction 95: 1335-1349. View
- Stetler CB, Ritchie J, Rycroft-Malone J, Schultz A, Charns M (2007) Improving quality of care through routine, successful implementation of evidence-based practice at the bedside: an organizational case study protocol using the Pettigrew and Whipp model of strategic change. Imp Sci 2: 1-13. View
- Carroll KM, Fenton LR, Ball SA, Nich C, Frankforter TL, et al. (2004) Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatients: a randomized placebo-controlled trial. Arch Gen Psychiatry 61: 264-272. View
- Carroll KM, Ball SA, Martino S, Nich C, Babuscio TA, et al. (2008) Computer-assisted delivery of cognitive-behavioral therapy for addiction: a randomized trial of CBT4CBT. Am J Psychiatry 165: 881-888. View
- McHugh RK, Hearon BA, Otto MW (2010) Cognitive behavioral therapy for substance use disorders. Psychiatr Clin North Am 33: 511-525. View
- Waldron HB, Kaminer Y (2004) On the learning curve: the emerging evidence supporting cognitive-behavioral therapies for adolescent substance abuse. Addiction 99 Suppl 2: 93-105. View
- Freeman A, Reinecke MA (1995) Cognitive therapy. New York: Guilford Press.
- Stephens RS, Babor TF, Kadden R, Miller M; Marijuana Treatment Project Research Group (2002) The Marijuana Treatment Project: rationale, design and participant characteristics. Addiction 97 Suppl 1: 109-124. View
- Pilling S, Hesketh K, Mitcheson L (2009) Psychosocial interventions in drug misuse: a framework and toolkit for implementing NICE-recommended treatment interventions. London: British Psychological Society, Centre for Outcomes, Research and Effectiveness (CORE) Research Department of Clinical, Educational and Health Psychology, University College. View
- Azrin NH (1976) Improvements in the community-reinforcement approach to alcoholism. Behav Res Ther 14: 339-348. View
- Hunt GM, Azrin NH (1973) A community-reinforcement approach to alcoholism. Behav Res Ther 11: 91-104. View
- Azrin NH, Sisson RW, Meyers R, Godley M (1982) Alcoholism treatment by disulfiram and community reinforcement therapy. J Behav Ther Exp Psychiatry 13: 105-112. View
- Meyers RJ, Miller WR (2001) A community reinforcement approach to addiction treatment: (International Research Monographs in the Addictions) Cambridge Univ Press.
- Mallams JH, Godley MD, Hall GM, Meyers RJ (1982) A social-systems approach to resocializing alcoholics in the community. J Stud Alcohol 43: 1115-1123.
- Finney JW, Monahan SC (1996) The cost-effectiveness of treatment for alcoholism: a second approximation. J Stud Alcohol 57: 229-243. View
- Rollnick S, Miller WR (1999) What is motivational interviewing? Behav Cogn Psychotherapy. 23: 325-334. View
- Garner BR, Barnes B, Godley SH (2009) Monitoring fidelity in the Adolescent Community Reinforcement Approach (A-CRA): the training process for A-CRA raters. J Behav Anal Health Fit Med 2: 43-54. View
- Dennis M, Godley SH, Diamond G, Tims FM, Babor T, et al. (2004) The Cannabis Youth Treatment (CYT) Study: main findings from two randomized trials. J Subst Abuse Treat 27: 197-213. View
- Garner BR, Godley MD, Funk RR, Dennis ML, Godley SH (2007) The impact of continuing care adherence on environmental risks, substance use, and substance-related problems following adolescent residential treatment. Psychol Addict Behav. 21: 488-497. View
- Slesnick N, Prestopnik JL, Meyers RJ, Glassman M (2007) Treatment outcome for street-living, homeless youth. Addict Behav 32: 1237-1251. View
- Beck AT, Hollon SD, Young JE, Bedrosian RC, Budenz D (1985) Treatment of depression with cognitive therapy and amitriptyline. Arch Gen Psychiatry 42: 142-148. View
- Smith C (1998) Assessing health needs in women's prisons. PSJ 224.
- Maude-Griffin PM1, Hohenstein JM, Humfleet GL, Reilly PM, Tusel DJ, et al. (1998) Superior efficacy of cognitive-behavioral therapy for urban crack cocaine abusers: main and matching effects. J Consult Clin Psychol 66: 832-837. View
- Godley SH, Meyers RJ, Smith JE, Karvinen T, Titus JC, et al. (2001) The adolescent community reinforcement approach for adolescent cannabis users: US Department of Health and Human Services. View
- Carroll KM (1998) A cognitive-behavioral approach: Treating cocaine addiction. National Institute on Drug Abuse. View
- Bukstein OG, Glancy LJ, Kaminer Y (1992) Pattern of affective comorbidity in a clinical population of dually diagonised adolescent substance abusers. J Ame Aca Child Adol Psychiat 31: 1041-1045. View
- Kaminer Y, Burleson JA, Goldberger R (2002) Psychotherapies for adolescent substance abusers: Short- and long-term outcomes. J Nerv Ment Dis 190: 737-745.
- Miller WR, Rollnick S (2002) Motivational interviewing: Preparing people for change. 2nd ed. New York: Guilford Press. View

- Presidential Message
- Nominations/Elections
- Past Presidents
- Member Spotlight
- Fellow List
- Fellowship Nominations
- Current Awardees
- Award Nominations
- SCP Mentoring Program
- SCP Book Club
- Pub Fee & Certificate Purchases
- LEAD Program
- Introduction
- Find a Treatment
- Submit Proposal
- Dissemination and Implementation
- Diversity Resources
- Graduate School Applicants
- Student Resources
- Early Career Resources
- Principles for Training in Evidence-Based Psychology
- Advances in Psychotherapy
- Announcements
- Submit Blog
- Student Blog
- The Clinical Psychologist
- CP:SP Journal
- APA Convention
- SCP Conference
CASE STUDY Richard (bipolar disorder, substance use disorder)
Case study details.
Richard is a 62-year-old single man who says that his substance dependence and his bipolar disorder both emerged in his late teens. He says that he started to drink to “feel better” when his episodes of depression made it hard for him to interact with his peers. He also states that alcohol and cocaine are a natural part of his manic episodes. He also notes that coming off the cocaine and binge drinking contribute to low mood, but he has not responded well to referrals to AA and past inpatient stays have led to only temporary abstinence. Yet, Richard is now trying to forge a closer relationship to his adult children, and he says he is especially motivated to get a better handle on both his bipolar disorder and his substance use. He has been more compliant with his mood stabilizing and antidepressant medication, and his psychiatrist would like his dual diagnoses addressed with psychotherapy.
- Alcohol Use
- Elevated Mood
- Impulsivity
- Mania/Hypomania
- Mood Cycles
- Substance Abuse
Diagnoses and Related Treatments
1. bipolar disorder, 2. mixed substance use/dependence.
Thank you for supporting the Society of Clinical Psychology. To enhance our membership benefits, we are requesting that members fill out their profile in full. This will help the Division to gather appropriate data to provide you with the best benefits. You will be able to access all other areas of the website, once your profile is submitted. Thank you and please feel free to email the Central Office at [email protected] if you have any questions
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
- Immediate Communication
- Published: 14 September 2020
COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States
- Quan Qiu Wang 1 ,
- David C. Kaelber 2 ,
- Rong Xu ORCID: orcid.org/0000-0003-3127-4795 1 &
- Nora D. Volkow ORCID: orcid.org/0000-0001-6668-0908 3
Molecular Psychiatry volume 26 , pages 30–39 ( 2021 ) Cite this article
48k Accesses
400 Citations
1066 Altmetric
Metrics details
A Correction to this article was published on 30 September 2020
This article has been updated
The global pandemic of COVID-19 is colliding with the epidemic of opioid use disorders (OUD) and other substance use disorders (SUD) in the United States (US). Currently, there is limited data on risks, disparity, and outcomes for COVID-19 in individuals suffering from SUD. This is a retrospective case-control study of electronic health records (EHRs) data of 73,099,850 unique patients, of whom 12,030 had a diagnosis of COVID-19. Patients with a recent diagnosis of SUD (within past year) were at significantly increased risk for COVID-19 (adjusted odds ratio or AOR = 8.699 [8.411–8.997], P < 10 −30 ), an effect that was strongest for individuals with OUD (AOR = 10.244 [9.107–11.524], P < 10 −30 ), followed by individuals with tobacco use disorder (TUD) (AOR = 8.222 ([7.925–8.530], P < 10 −30 ). Compared to patients without SUD, patients with SUD had significantly higher prevalence of chronic kidney, liver, lung diseases, cardiovascular diseases, type 2 diabetes, obesity and cancer. Among patients with recent diagnosis of SUD, African Americans had significantly higher risk of COVID-19 than Caucasians (AOR = 2.173 [2.01–2.349], P < 10 −30 ), with strongest effect for OUD (AOR = 4.162 [3.13–5.533], P < 10 −25 ). COVID-19 patients with SUD had significantly worse outcomes (death: 9.6%, hospitalization: 41.0%) than general COVID-19 patients (death: 6.6%, hospitalization: 30.1%) and African Americans with COVID-19 and SUD had worse outcomes (death: 13.0%, hospitalization: 50.7%) than Caucasians (death: 8.6%, hospitalization: 35.2%). These findings identify individuals with SUD, especially individuals with OUD and African Americans, as having increased risk for COVID-19 and its adverse outcomes, highlighting the need to screen and treat individuals with SUD as part of the strategy to control the pandemic while ensuring no disparities in access to healthcare support.
Similar content being viewed by others
Association of COVID-19 with endocarditis in patients with cocaine or opioid use disorders in the US


Associations between classic psychedelics and opioid use disorder in a nationally-representative U.S. adult sample

Medical and genetic correlates of long-term buprenorphine treatment in the electronic health records
Introduction.
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and has rapidly escalated into a global pandemic [ 1 ]. The global pandemic of COVID-19 is colliding in the United States (US) with the epidemic of opioid use disorders (OUD) and overdose mortality [ 2 , 3 , 4 ]. Currently, there is little if any quantitative analysis of the risks and outcomes for COVID-19 infection in individuals suffering from an OUD and those suffering from other substance use in the US. In addition, there is minimal data on how race and other demographic factors affect the risk and outcomes of COVID-19 among patients with SUD including OUD.
It is estimated that more than 70,000 people will die in the US from an overdose in 2019 mostly from opioid overdoses, which are driven by the respiratory depressant effects of opioids. Considering that COVID-19 affects pulmonary function this combination could be particularly lethal. Additionally, ~10.8% of adults in the US have a substance use disorders (SUD) including alcohol (AUD) and tobacco (TUD) [ 5 ]. To the extent that chronic use of tobacco, alcohol and other drugs is associated with cardiovascular (arrhythmias, cardiac insufficiency, and myocardial infarction), pulmonary (COPD, pulmonary hypertension), and metabolic diseases (diabetes, hypertension) [ 6 , 7 , 8 , 9 , 10 ] all of which are risk factors for COVID-19 infection and for worse outcomes [ 11 , 12 , 13 ] one can also predict that individuals with SUD including OUD would be at increased risk for adverse COVID-19 outcomes [ 2 ]. Preliminary reports regarding higher risk for adverse outcomes with COVID-19 and smoking have been inconclusive [ 14 , 15 , 16 ]. Currently there is little research on the effects of other drugs including opioids, cannabis, cocaine and alcohol on the susceptibility to COVID-19 infection and to adverse outcomes [ 2 ].
Material and methods
Database description.
We performed a retrospective case-control study using de-identified population-level electronic health record (EHR) data collected by the IBM Watson Health Explorys from 360 hospitals and 317,000 providers across 50 states in the US since 1999 [ 17 ]. The EHRs are de-identified according to the Health Insurance Portability and Accountability Act and the Health Information Technology for Economic and Clinical Health Act standards. After the de-identification process, curation process normalizes the data through mapping key elements to widely-accepted standards [ 18 ]. Specifically, disease terms are coded using the Systematized Nomenclature of Medicine-Clinical Terms (SNOMED-CT), a global standard for health terms that provides the core general terminology for EHRs [ 19 ]. Previous studies showed that with this large-scale and standardized EHR database, large case-control studies can be undertaken efficiently [ 20 , 21 , 22 , 23 , 24 ], including our recent studies [ 23 , 24 ].
Study population
At the time of this study (June 15, 2020), the study population consisted of 73,099,850 unique patients, including 7,510,380 patients with a diagnosis with SUD (diagnosis made within the past year or prior) of whom 722,370 had been recently diagnosed with SUD (diagnosed within past year), 12,030 patients diagnosed with COVID-19, 1880 patients with lifetime diagnosis of SUD and COVID-19, and 1050 with recent SUD diagnosis and COVID-19. The status of COVID-19 was based on the concept “Coronavirus infection (disorder)” (SNOMED-CT Concept Code 186747009) and we further limited the diagnosis time frame to within the past year to capture the timing of new cases arising during the COVID-19 pandemic. The outcome measures were COVID-19 diagnosis, rates of death, and hospitalization. The specific types of SUD examined included alcohol use disorder (AUD), OUD, tobacco use disorder (TUD), cannabis use disorder (CUD), and cocaine use disorder (Cocaine-UD). Other types of SUDs were not investigated due to their small number of COVID-19 cases.
The status of “SUD” was based on diagnosis of “Drug dependence (disorder)” on SNOMED-CT Concept Code 191816009, or of “Substance abuse (disorder)” on SNOMED-CT Concept Code 66214007. The status of “AUD” was based on the diagnosis of “Alcohol dependence (disorder)” on Concept Code 66590003, or of “Alcohol abuse (disorder)” on Concept Code 7200002. The status of “CUD” was based on the diagnosis of “Cannabis dependence (disorder)” on Concept Code 85005007 or of “Cannabis abuse (disorder)” on Concept Code 37344009. The status of “Cocaine-UD” was based on the diagnosis of “Cocaine dependence (disorder)” on SNOMED-CT Concept Code 31956009, or of “Cocaine abuse (disorder)” on Concept Code 78267003. The status of “OUD” was based on diagnosis of “Opioid dependence (disorder)” on Concept Code 75544000, or of “Nondependent opioid abuse (disorder)” on Concept Code 191909007. The status of “TUD” was based on diagnosis of “Nicotine dependence (disorder)” on Concept Code 56294008. In our study, patients with SUD were categorized into two groups: patients with a lifetime diagnosis of SUD (diagnosed within past year or prior) and patients with a “recent” SUD (diagnosed within the past year). The first group represents patients with any SUD diagnosis (active or recovered). The second group is a subset of the first group but more likely consists of patients with active SUD. Through this manuscript we use the term SUD, following DSM-5 [ 25 ], which combines the prior categories of substance abuse and substance dependence from DSM-4.
The following analyses were performed: (1) we examined if patients diagnosed with SUD were at increased the risk for COVID-19, adjusted for age, gender, race, and insurance type. The exposure groups were patients diagnosed with SUD, the unexposed groups were patients without SUD, and the outcome measure was diagnosis of COVID-19. Separate analyses were done for patients with a lifetime SUD diagnosis and for patients with a recent SUD. Separate analyses were done for subtypes of SUD. (2) We examined how demographic factors affected COVID-19 risk among patients with recent diagnosis of SUD. The case groups were patients with SUD and one of the following demographic factors: female, senior, African American. The comparison groups were patients with SUD and one of the following corresponding demographic factors (male, adult, Caucasian). The outcome measure was diagnosis of COVID-19. (3) We examined rates of death and hospitalization among patients with COVID-19 and SUD and compared outcomes of African Americans to those of Caucasians with SUD.
Statistical analysis
The adjusted odds ratio (AOR), 95% CI and P values were calculated using the Cochran–Mantel–Haenszel method [ 26 ] by controlling for age groups (juniors age <18 years, adults age 18–65 years, senior age > 65 years), gender (female, male), race (Caucasian, African American), and insurance type (private, medicare, medicaid, self pay). Other demographic groups were not included due to insufficient sample sizes for COVID-19 cases. Two-sided, 2-sample test for equality of proportions with continuity correction were used to compare prevalence of comorbidities and outcomes. Statistical tests were conducted with significance set at P value < 0.05 (two sided). All analyses were done using R, version 3.6.3.
Patient characteristics
The baseline characteristics of the study population (as of June 15, 2020) are presented in Table 1 . Among 73,099,850 patients, 7,510,380 patients had lifetime SUD (diagnosed within the last or prior years) (10.27% of study population), including 1,264,990 with AUD (1.73% of study population), 222,680 with Cocaine-UD (0.30%), 490,420 with CUD (0.67%), 6,414,580 with TUD (8.77%), and 471,520 with OUD (0.65%). Among 73,099,850 patients, 722,370 had recent SUD (diagnosed within the last year) (0.99% of total population), including 83,100 with AUD (0.11%), 14,800 with Cocaine-UD (0.02%), 27,650 with CUD (0.04%), 611,750 with TUD (0.84%), and 43,160 with OUD (0.06%).
Among 12,030 patients diagnosed with COVID-19, 1880 patients had lifetime SUD (15.63% in COVID-19 population), including 320 with AUD (2.66%), 70 with Cocaine-UD (0.58%), 80 with CUD (0.67%), 1470 with TUD (12.22%), and 210 with OUD (1.75%). Among 12,030 patients diagnosed with COVID-19, 1050 had recent SUD (8.73% in COVID-19 population), including 130 with recent AUD (1.03%), 30 with Cocaine-UD (0.25%), 30 with CUD (0.25%), 840 with TUD (6.98%), and 90 with OUD (0.75%).
Risk associations between SUD and COVID-19
Patients with recent SUD diagnosis had significantly higher risk of developing COVID-19 compared to patients without recent SUD diagnosis, after adjusting for age, gender, race, and insurance types. The AOR between recent SUD diagnoses and COVID-19 was 8.699 [8.411–8.997]. Among patients with SUD subtypes, individuals with OUD had the largest risk (AOR = 10.244 [9.107–11.524]), followed by TUD (AOR = 8.222 ([7.925–8.530]), AUD (AOR = 7.752 [7.04–8.536]), Cocaine-UD (AOR = 6.53 [5.242–8.134]) and CUD (AOR = 5.296 [4.392–6.388]) (Fig. 1a ).
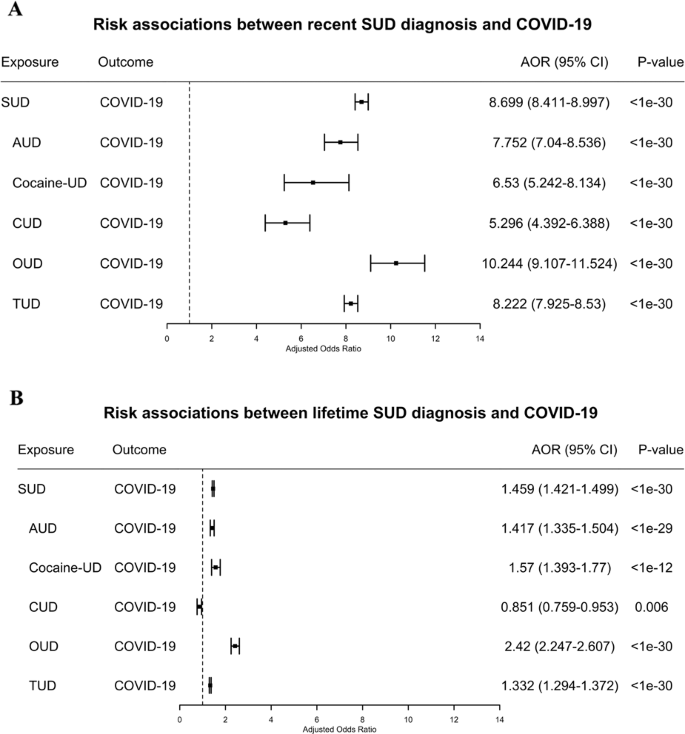
a Risk associations of recent (diagnosis made in the last year) SUD diagnoses (and its subtypes) with COVID-19; b Risk associations of lifetime (diagnosed in the last year or prior) SUD diagnoses (and its subtypes) with COVID-19. SUD substance use disorder, AUD alcohol use disorder, Cocaine-UD cocaine use disorder, CUD cannabis use disorder, OUD opioid use disorder, TUD tobacco use disorder. Subtypes without sufficient sample sizes for COVID-19 cases are not shown.
Patients with lifetime SUD diagnosis had significantly higher risk of developing COVID-19 compared to patients without SUD, after adjusting for age, gender, race, and insurance types. The AOR between those with lifetime SUD and COVID-19 was 1.459 [1.421–1.499]; for whom, individuals with OUD had the largest risk (AOR = 2.42 [2.247–2.607], followed by cocaine-UD (AOR = 1.57 [1.393–1.77], AUD (AOR = 1.417 [1.335–1.504], and TUD (AOR = 1.332 [1.294–1.372]. Among 7,510,380 patients with lifetime SUD diagnosis, 722,370 had recent diagnosis (9.6%) (Fig. 1b ).
Patients with SUD often have multiple comorbidities, including cardiovascular, pulmonary, metabolic diseases, and increased susceptibility to infections [ 6 , 7 , 8 , 9 , 10 ], which are also risk factors for COVID-19 [ 11 , 12 , 13 ]. We then examined prevalence of these known COVID-19 risk factors among adult patients with recent diagnosis of SUD and compared them to adult patients without recent SUD diagnosis. As shown in Table 2 , patients with recent diagnosis of SUD had significantly higher prevalence of asthma, chronic kidney disease, chronic obstructive pulmonary disease, diabetes, cancer, HIV, chronic liver disease, cardiovascular diseases including hypertension, and obesity as compared to patients without recent SUD diagnosis of SUD. Patients with recent diagnosis of OUD had higher risk of COVID-19 than other SUD subtypes, however, the prevalence of risk factors for COVID-19 was not higher than for other SUD subtypes.
Individuals with OUD had the greatest risk for COVID-19 among patients with SUD (Fig. 1 ) but they did not have more comorbidities (known COVID-19 risk factors) than those with other SUDs. We then examined if medications used to treat OUD (MOUD), including methadone (though when used for OUD its dispensed through methadone clinics and not regular prescriptions), buprenorphine (which is also prescribed for pain management) and naltrexone, affected the risk of patients with OUD in getting COVID-19. There was no significant difference in risk for COVID-19 between OUD patients who were not prescribed methadone, buprenorphine or naltrexone vs. those that were (AOR = 1.064, [0.871–1.3], P value = 0.578) after adjusting for age, gender, race, and insurance types. These results indicate that these opioid medications had no significant effects on OUD patients’ risk for COVID-19. However, a limitation in this analysis is that the EHR dataset does not capture methadone given through methadone clinics, which is the authorized way when used for the treatment of OUD. Regardless, our results did not show differences in COVID risk for OUD patients prescribed methadone, buprenorphine or naltrexone compared to those who did not receive those medications.
Effects of demographics on risk of COVID-19 among patients with recent SUD
Among patients with a recent diagnosis of SUD, seniors were more likely to develop COVID-19 compared to adults (AOR = 1.307 (1.207–1.416]) and African Americans were more likely to develop COVID-19 compared to Caucasians (AOR = 2.173 [2.01–2.349], after adjusting for age, gender and insurance types. Gender had no significant effects, after adjusting for age, race, and insurance types. Of the three demographic factors examined, race had the largest effect on COVID-19 risk, which was true across individuals with SUD, AUD, OUD, and TUD with the largest effects for patients with recent diagnosis of OUD. Among patients with recent diagnosis of OUD, African Americans had significantly higher risk of COVID-19 than Caucasians (4.162 [3.13–5.533], after adjusting for age, gender, and insurance types (Fig. 2 ). We examined prevalence of known COVID-19 risk factors among African Americans and Caucasians with recent diagnosis of SUD (and its subtypes). We showed that African Americans with recent diagnosis of SUDs had higher prevalence of asthma, chronic kidney disease, type 2 diabetes, hypertension, obesity, and HIV compared to Caucasians, while prevalence of COPD, chronic liver disease, cardiovascular disorders, and cancer was similar or lower (data not shown).
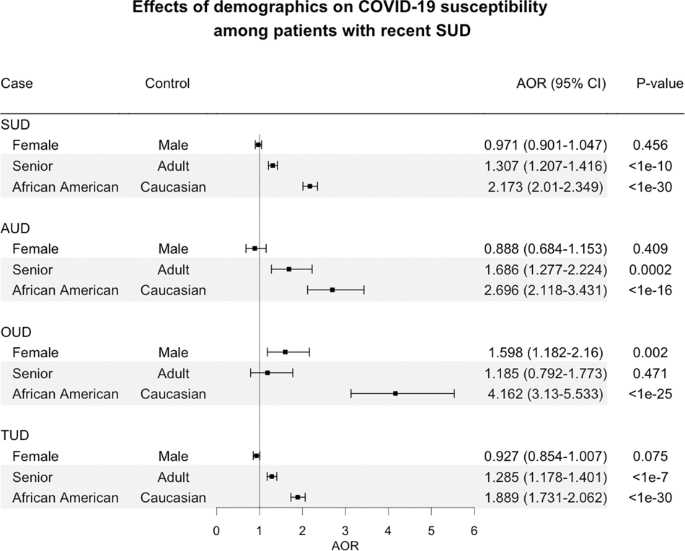
Cocaine-UD and CUD were not examined due to insufficient sample sizes of COVID-19 for stratifications. Senior (age > 65 years). Adult (age 18–65 years).
Rates of deaths and hospitalizations in COVID-19 patients with SUD
Among 12,030 COVID-19 patients, 790 died (6.57%). African Americans with COVID-19 had a death rate of 7.50%, significantly higher than for Caucasians who had a rate of 6.18% ( P = 0.007). Among 1,880 COVID-19 patients with lifetime SUD, 180 died (9.57%), a rate significantly higher than the death rate of 6.57% for all COVID-19 patients ( P < 0.0001). African Americans with COVID-19 and lifetime SUD had a death rate of 12.99%, significantly higher than the rate of 8.57% for Caucasians with COVID-19 and lifetime SUD ( P = 0.003). Among 1050 COVID-19 patients with recent diagnosis of SUD, 100 died (9.52%), a rate significantly higher than that for general COVID-19 patients ( P = 0.003) and similar to that for COVID-19 patients with lifetime SUD (9.57%). Death rates for patients with COVID-19 and a recent diagnosis of SUD did not differ significantly between African Americans (12.20%) and Caucasians (9.84%) ( P = 0.276) (Fig. 3a ). The death rates for SUD subtypes were not examined due to their small sample sizes.
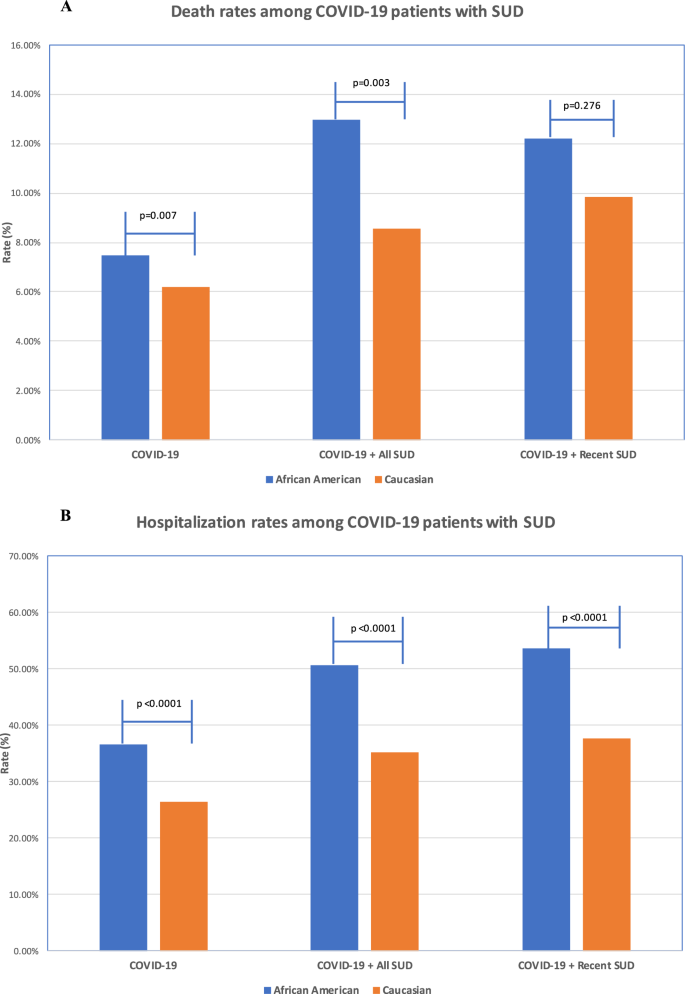
a Death rates among patients with COVID-19 and SUD (African American vs. Caucasians); b Hospital admission rates among patients with COVID-19 and SUD (African American vs. Caucasians). The SNOMED-CT concepts “Hospital admission (procedure)” (ID 32485007) was used to obtain hospitalization status from patient EHRs. Explorys regularly imports from the Social Security Death index for the “deceased” status.
Among 12,030 COVID-19 patients, 3620 were hospitalized (30.09%) and the rate was significantly higher among the African Americans (35.56%) than the Caucasians (26.36%) ( P < 0.0001). Among 1880 COVID-19 patients with lifetime SUD, 770 were hospitalized (40.96%), a rate significantly higher than for all COVID-19 patients (30.09%) ( P < 0.0001) and also significantly higher among the African Americans (50.65%) than the Caucasians (35.24%) ( P < 0.0001). Among 1050 COVID-19 patients with recent diagnosis of SUD, 460 were hospitalized (43.81%), a rate significantly higher than for general COVID-19 patients (30.09%) ( P < 0.0001) and similar to that for COVID-19 patients with lifetime SUD (40.96%) ( P = 0.144). Hospitalization rates for COVID-19 patients with a recent diagnosis of SUD were significantly higher for African Americans (53.66%), than for Caucasians (37.70%) ( P < 0.0001) (Fig. 3b ).
Based on EHR patient data in the US we show that individuals with SUD, particularly recent OUD, were at increased risk for COVID-19 and these effects were exacerbated in African Americans compared to Caucasians. The higher prevalence of kidney, pulmonary, liver, cardiovascular, metabolic, and immune-related disorders in COVID-19 patients with SUD and also in African Americans are likely contribute to their higher risk. These findings identify individuals with SUD as a vulnerable population, especially African Americans with SUDs, who are at significantly increased risk for COVID-19 and its adverse outcomes, highlighting the need to screen and treat SUD as part of the strategy to control the pandemic while ensuring that there are no disparities in access to healthcare support for African Americans.
In the Explorys EHR database, 10.3% of the study population had a diagnosis of SUD, which is similar to the reported prevalence of 10.8% among people aged 18 or older in the US according to the 2018 National Survey on Drug Use and Health (NSDUH) [ 5 ]. However the prevalence rates for SUD subtypes from the Explorys EHR database was lower than for NSDUH (12 years or older population) except for OUD and Cocaine-UD. For TUD the rate was 10.40%, which is also lower than 13.7% of current cigarette smokers in the US adult population [ 27 ]. These discrepancies are likely to be caused by the failure of the health system to adequately screen for and accurately diagnose SUDs, which could have significantly under-estimated the risk of patients with SUD for COVID-19 illness and adverse outcomes.
The analyses showed that a recent diagnosis of SUD significantly increased the risk of COVID-19 that was highest for recent diagnosis of OUD followed by TUD, AUD and Cocaine-UD, and lowest for CUD. Patients with both SUD and COVID-19 also had significantly worse outcomes (death, hospitalization) than general COVID-19 patients. Compared to patients without SUD, patients with recent SUD had significantly higher prevalence of chronic kidney, liver, lung diseases, cardiovascular diseases, type 2 diabetes, obesity and cancer. However, the prevalence of known risk factor for COVID-19 among patients with OUD was not higher than patients with other types of SUD. These results suggest that while comorbidities associated with SUD likely contributed to the increased risk of COVID-19 and to worse outcomes among SUD patients, specific pharmacological effects of drugs of abuse (e.g., opioid induced respiratory depression) as well as behavioral and socioeconomic factors could facilitate COVID-19 infection and increase risk for adverse outcomes.
Among patients with recent diagnosis of SUD, African Americans had significantly higher risk of COVID-19 than Caucasians, an effect that was strongest for African Americans with OUD and they also had worse outcomes (death and hospitalizations). This is consistent with data from states and counties across the US showing that the coronavirus affects African Americans at a disproportionately high rate and that the they suffer a greater death toll [ 28 , 29 , 30 , 31 ]. We showed that adult African Americans with recent diagnosis of SUDs had higher prevalence of asthma, chronic kidney disease, type 2 diabetes, hypertension, obesity and HIV compared to adult Caucasians. These enriched comorbidities in African Americans with SUD could underly their higher susceptibility to COVID-19 and their risk for adverse COVID outcomes along with socioeconomic disparities. However, these comorbidities alone may not be sufficient to explain the observed several-fold increase of COVID-19 diagnosis in African Americans as compared to Caucasians or their increased death rates. Other factors including access to healthcare, socioeconomic status and other social adversity components may have contributed negatively to their increased risk of COVID-19 as well as to the adverse outcomes.
Consistent with other reports [ 12 , 13 ], our study showed that seniors were more likely to develop COVID-19 than adults, which was also expected since hypertension, diabetes, obesity, cardiovascular diseases, and weakened immune function are more common in seniors than in adults. No disparity was observed for gender.
Our study is based on retrospective analysis of patient EHR data. Patient EHR data have been widely used and accepted for observational studies including health utilization, drug utilization, epidemiology (incidence/prevalence), risk factors, and safety surveillance [ 32 , 33 , 34 ]. However patient EHR data have inherent limitations when used for research purposes: data are collected for billing purposes, often suffer from under, over, or misdiagnosis, do not include all confounding factors, have limited time-series information, limited information of medication adherence and patient outcomes, among others. The Explorys EHR Database collects data from multiple health information systems. Since EHR adoption and health IT use generally lags in rural areas due to lack of financial and technical resources, patients from rural areas are likely less represented in our study population. In our study, disease diagnoses in the patient EHR data were coded using SNOMED-CT terminology and for SUD these differ from categories used by DSM-5. A further limitation of our study is that “COVID-19” (Concept ID 840539006) was not yet included the Explorys EHRs database at the time of this study. This new concept was first included in the March 2020 SNOMED-CT International Edition Interim Release, with a planned update in July, 2020 [ 35 ]. At the time of this study, this update has not been yet incorporated in Explorys EHRs. Despite these limitations, this large nationwide database allows us to assess a wide population helping us identify large trends (not necessarily for accurate prevalence estimation) in risks, disparities and outcomes of COVID-19 in SUD patients engaged with healthcare systems.
A major limitation for this and other studies of COVID-19 has been the limited number of individuals who are tested for COVID-19, which can underestimate prevalence in the general population. For our study this is further confounded by the likelihood that patients with pulmonary, cardiac, metabolic or immune conditions, many of which are co-morbid with SUD, might have been more likely to be tested. It is also confounded by the likelihood that patients with specific SUDs (e.g., Cocaine-UD and OUD) might have been less likely to be tested due to socioeconomic factors or stigma. Widespread accessibility to COVID-19 testing in the future will allow more accurate comparisons of COVID prevalence between those with and without SUD.
Additional limitations for this study include: (1) possible ascertainment bias as illicit SUD might have been underreported and individuals with SUD particularly illicit SUD are less likely to access healthcare, which would result in their lower representation in EHR, (2) the EHR database did not encode for current or active drug use, which is why we relied on a recent SUD diagnoses assuming that those patients were more likely to be active drug users, and (3) due to limited information of socioeconomic information on the EHR data, we were unable to assess the effects of social adversity and its interaction with medical conditions to COVID-19 risk, race disparity and adverse outcomes among patients with SUD. Social adversity is likely to have contributed not only to the higher risk for COVID-19 among patients with SUD but also to the even higher risk among African Americans patients with SUD.
In our study, we showed that patients with SUDs has significantly higher prevalence of comorbidities, which are known risk factors for COVID-19, as compared to patients without SUDs. Our study did not control for these comorbidities when assessing the risk associations between SUD and COVID-19 for two main reasons. First, the central hypothesis of this study was that comorbidities associated with SUD, including type 2 diabetes, hypertension, heart disease, chronic kidney, lung, and liver diseases, largely contributed to patients’ risk to COVID-19 and its adverse outcomes. Second, due to limited sample sizes for COVID-19 cases among patients with SUD (1880 cases for all SUD and 210 for OUD), the large number of SUD-associated comorbidities, as well as inter-dependency among comorbidities (e.g., diabetes, hypertension, and obesity), we are currently unable to control for these comorbidities as well as their associated medications, behaviors and other socioeconomic factors in order to assess the direct effects of addictive drugs or of SUD as a disease entity on COVID-19 risk. As more COVID-19 related data will be captured by EHR databases in the future, we will be able to investigate how SUD contributes to COVID-19 risk and outcomes in finer-grained details.
In summary, our findings at a macroscopic level provide evidence that SUD should be considered a condition that increases risk for COVID-19, a comorbidity that has particularly deleterious effects to African Americans. This has implication to healthcare as it relates to expanding testing and making decisions of who might need hospitalizations. Similarly, when vaccine or other treatments become available, this has implication for deciding who is at greater risk. They also highlight the exacerbation of healthcare disparities from COVID-19 driven by social and economic factors that place certain groups at increased risks for both SUD as well as risk and adverse outcomes from COVID-19. Finally, our findings also underscore the importance of providing support for the treatment and recovery of individuals with SUD as part of the strategy to control the COVID pandemic.
Data availability
All the data are publicly available at http://nlp.case.edu/public/data/COVID_SUD/ .
Change history
30 september 2020.
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
Centers for Disease Control and Prevention (CDC). Coronavirus Disease 2019 (COVID-19) Cases in the United States. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html . Accessed 15 June 2020.
Volkow ND. Collision of the COVID-19 and addiction epidemics. Ann Intern Med. 2020;M20-1212. https://doi.org/10.7326/M20-1212 .
Becker WC, Fiellin DA. When epidemics collide: coronavirus disease 2019 (COVID-19) and the opioid crisis. Ann Intern Med. 2020;M20-1210. https://doi.org/10.7326/M20-1210 .
Alexander GC, Stoller KB, Haffajee RL, Saloner B. An epidemic in the midst of a pandemic: opioid use disorder and COVID-19. Ann Intern Med. 2020;M20-1141. https://doi.org/10.7326/M20-1141 .
The Substance Abuse and Mental Health Services Administration (SAMHSA) of the U.S. Department of Health and Human Services. Key Substance Use and Mental Health Indicators in the United States: results from the 2018 National Survey on Drug Use and Health. https://www.samhsa.gov/data/sites/default/files/cbhsq-reports/NSDUHNationalFindingsReport2018/NSDUHNationalFindingsReport2018.pdf . Accessed 15 June 2020.
National Institute on Drug Abuse. Health consequences of drug misuse (2020). https://www.drugabuse.gov/related-topics/health-consequences-drug-misuse . Accessed 10 June 2020.
Bahorik AL, Satre DD, Kline-Simon AH, Weisner CM, Campbell CI. Alcohol, cannabis, and opioid use disorders, and disease burden in an integrated health care system. J Addict Med. 2017;11:3–9. https://doi.org/10.1097/ADM.0000000000000260 .
Article PubMed PubMed Central Google Scholar
Friedman H, Pross S, Klein TW. Addictive drugs and their relationship with infectious diseases. FEMS Immunol Med Microbiol. 2006;47:330–42. https://doi.org/10.1111/j.1574-695X.2006.00097.x .
Article CAS PubMed Google Scholar
Friedman H, Newton C, Klein TW. Microbial infections, immunomodulation, and drugs of abuse. Clin Microbiol Rev. 2003;16:209–19. https://doi.org/10.1128/cmr.16.2.209-219.2003 .
Article CAS PubMed PubMed Central Google Scholar
National Institute on Drug Abuse. Health Consequences of Drug Misuse:HIV, Hepatitis, and Other Infectious Diseases. https://www.drugabuse.gov/publications/health-consequences-drug-misuse/hiv-hepatitis-other-infectious-diseases . Accessed 15 June 2020..
The Centers for Disease Control and Prevention (CDC). Groups at higher risk for COVID-19 severe illness (June, 2020). https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html#serious-heart-conditions . Accessed 10th June 2020.
Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA. 2020;e206775. https://doi.org/10.1001/jama.2020.6775 .
Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–62. https://doi.org/10.1016/S0140-6736(20)30566-3 .
Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020;18:20. https://doi.org/10.18332/tid/119324 .
Patanavanich R, Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res. 2020; ntaa082. https://doi.org/10.1093/ntr/ntaa082 .
Berlin I, Thomas D, Le Faou AL, Cornuz J. COVID-19 and smoking. Nicotine Tob Res. 2020;ntaa059. https://doi.org/10.1093/ntr/ntaa059 .
IBM Explorys EHR solutions. https://www.ibm.com/watson-health/about/explorys . Acessed through May 15 to June 15, 2020.
Bodenreider O. The Unified Medical Language System (UMLS): integrating biomedical terminology. Nucleic Acids Res. 2004;32:D267–70. https://doi.org/10.1093/nar/gkh061 .
SNOMED International. The systematized nomenclature of medicine—clinical terms (SNOMED CT). http://www.snomed.org/snomed-ct/why-snomed-ct .
Kaelber DC, Foster W, Gilder J, Love TE, Jain AK. Patient characteristics associated with venous thromboembolic events: a cohort study using pooled electronic health record data. J Am Med Inf Assoc. 2012;19:965–72. https://doi.org/10.1136/amiajnl-2011-000782 .
Article Google Scholar
Patel VN, Kaelber DC. Using aggregated, de-identified electronic health record data for multivariate pharmacosurveillance: a case study of azathioprine. J Biomed Inf. 2014;52:36–42. https://doi.org/10.1016/j.jbi.2013.10.009 .
Winhusen T, Theobald J, Kaelber DC, Lewis D. Medical complications associated with substance use disorders in patients with type 2 diabetes and hypertension: electronic health record findings. Addiction 2019;114:1462–70. https://doi.org/10.1111/add.14607 .
Zhou M, Xu R, Kaelber DC, Gurney ME. Tumor Necrosis Factor (TNF) blocking agents are associated with lower risk for Alzheimer’s disease in patients with rheumatoid arthritis and psoriasis. PLoS ONE. 2020;15:e0229819. https://doi.org/10.1371/journal.pone.0229819 .
Zhou M, Zheng CL, Xu R. Combining phenome-driven drug target prediction with patients’ electronic health records-based clinical corroboration towards drug discocery. Bioinformatics. 2020. https://doi.org/10.1093/bioinformatics/btaa451.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Association Publishing.
Kuritz SJ, Landis JR, Koch GG. A general overview of Mantel–Haenszel methods: applications and recent developments. Annu Rev Public Health. 1988;9:123–60. https://doi.org/10.1146/annurev.pu.09.050188.001011 .
Creamer MR, Wang TW, Babb S, Cullen KA, Day H, Willis G, et al. Tobacco product use and cessation indicators among adults—United States, 2018. Morb Mortal Wkly Rep. 2019;68:1013–9. https://doi.org/10.15585/mmwr.mm6845a2 .
Yancy CW. COVID-19 and African Americans. JAMA. 2020. https://doi.org/10.1001/jama.2020.6548 .
Owen WF Jr, Carmona R, Pomeroy C. Failing another national stress test on health disparities. JAMA. 2020. https://doi.org/10.1001/jama.2020.6547 .
Wadhera RK, Wadhera P, Gaba P, Figueroa JF, Maddox KE, Yeh RW, et al. Variation in COVID-19 hospitalizations and deaths across New York city Boroughs. JAMA. 2020;e207197. https://doi.org/10.1001/jama.2020.7197 .
Williams DR, Cooper LA. COVID-19 and health equity-a new kind of “herd immunity”. JAMA. 2020. https://doi.org/10.1001/jama.2020.8051 .
Cowie MR, Blomster JI, Curtis LH, Duclaux S, Ford I, Fritz F, et al. Electronic health records to facilitate clinical research. Clin Res Cardiol. 2017;106:1–9. https://doi.org/10.1007/s00392-016-1025-6 .
Article PubMed Google Scholar
Coorevits P, Sundgren M, Klein GO, Bahr A, Claerhout B, Daniel C, et al. Electronic health records: new opportunities for clinical research. J Intern Med. 2013;274:547–60. https://doi.org/10.1111/joim.12119 .
Ahmad FS, Chan C, Rosenman MB, Post WS, Fort DG, Greenland P, et al. Validity of cardiovascular data from electronic sources: the multi-ethnic study of atherosclerosis and HealthLNK. Circulation. 2017;136:1207–16. https://doi.org/10.1161/CIRCULATIONAHA.117.027436 .
SNOMED CT and COVID-19. https://www.snomed.org/snomed-ct/covid-19 . Data Accessed 15th June 2020.
Download references
Acknowledgements
RX acknowledges support from Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under the NIH Director’s New Innovator Award number DP2HD084068, NIH National Institute on Aging R01 AG057557, R01 AG061388, R56 AG062272, American Cancer Society Research Scholar Grant RSG-16-049-01—MPC, The Clinical and Translational Science Collaborative (CTSC) of Cleveland 1UL1TR002548-01.
The funder of the study had no role in study design, data collection, data analysis, data interpretation, and writing of the report. The corresponding author (RX) had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author information
Authors and affiliations.
Center for Artificial Intelligence in Drug Discovery, School of Medicine, Case Western Reserve University, Cleveland, OH, USA
Quan Qiu Wang & Rong Xu
Departments of Internal Medicine and Pediatrics and the Center for Clinical Informatics Research and Education, The MetroHealth System, Cleveland, OH, USA
David C. Kaelber
National Institute on Drug Abuse, National Institutes of Health, Bethesda, MD, USA
Nora D. Volkow
You can also search for this author in PubMed Google Scholar
Contributions
QW, RX, and NDV conceived the study, designed the study, and authored the paper. QW and RX conducted the analysis. DK contributed to Explorys EHR database-related search questions and medical informatics-related questions. All authors approved the paper. QW and RX had access to the original data.
Corresponding authors
Correspondence to Rong Xu or Nora D. Volkow .
Ethics declarations
Conflict of interest.
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Reprints and permissions
About this article
Cite this article.
Wang, Q.Q., Kaelber, D.C., Xu, R. et al. COVID-19 risk and outcomes in patients with substance use disorders: analyses from electronic health records in the United States. Mol Psychiatry 26 , 30–39 (2021). https://doi.org/10.1038/s41380-020-00880-7
Download citation
Received : 22 June 2020
Revised : 20 August 2020
Accepted : 03 September 2020
Published : 14 September 2020
Issue Date : January 2021
DOI : https://doi.org/10.1038/s41380-020-00880-7
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
This article is cited by
Predictors of mental health among u.s. adults during covid-19 early pandemic, mid- pandemic, and post-vaccine eras.
- Niloofar Ramezani
- Bruce G. Taylor
- Faye S. Taxman
BMC Public Health (2024)
The impact of changes in opioid dependency treatment upon COVID-19 transmission in Sydney, Australia: a retrospective longitudinal observational study
- Benjamin T. Trevitt
- Victoria Hayes
- Nicholas Lintzeris
Trajectories of mental health outcomes following COVID-19 infection: a prospective longitudinal study
- Farzaneh Badinlou
- Fatemeh Rahimian
- Markus Jansson-Fröjmark
Hospital admissions among patients with Comorbid Substance Use disorders: a secondary analysis of predictors from the NavSTAR Trial
- Courtney D. Nordeck
- Sharon M. Kelly
- Jan Gryczynski
Addiction Science & Clinical Practice (2024)
Structural and social changes due to the COVID-19 pandemic and their impact on engagement in substance use disorder treatment services: a qualitative study among people with a recent history of injection drug use in Baltimore, Maryland
- Eshan U. Patel
- Suzanne M. Grieb
- Becky L. Genberg
Harm Reduction Journal (2024)
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies

An official website of the United States government
Here’s how you know
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you’ve safely connected to the .gov website. Share sensitive information only on official, secure websites.
Common Comorbidities with Substance Use Disorders Research Report Part 1: The Connection Between Substance Use Disorders and Mental Illness
Many individuals who develop substance use disorders (SUD) are also diagnosed with mental disorders, and vice versa. 2,3 Although there are fewer studies on comorbidity among youth, research suggests that adolescents with substance use disorders also have high rates of co-occurring mental illness; over 60 percent of adolescents in community-based substance use disorder treatment programs also meet diagnostic criteria for another mental illness. 4
Data show high rates of comorbid substance use disorders and anxiety disorders—which include generalized anxiety disorder, panic disorder, and post-traumatic stress disorder. 5–9 Substance use disorders also co-occur at high prevalence with mental disorders, such as depression and bipolar disorder, 6,9–11 attention-deficit hyperactivity disorder (ADHD), 12,13 psychotic illness, 14,15 borderline personality disorder, 16 and antisocial personality disorder. 10,15 Patients with schizophrenia have higher rates of alcohol, tobacco, and drug use disorders than the general population. 17 As Figure 1 shows, the overlap is especially pronounced with serious mental illness (SMI). Serious mental illness among people ages 18 and older is defined at the federal level as having, at any time during the past year, a diagnosable mental, behavior, or emotional disorder that causes serious functional impairment that substantially interferes with or limits one or more major life activities. Serious mental illnesses include major depression, schizophrenia, and bipolar disorder, and other mental disorders that cause serious impairment. 18 Around 1 in 4 individuals with SMI also have an SUD.
Data from a large nationally representative sample suggested that people with mental, personality, and substance use disorders were at increased risk for nonmedical use of prescription opioids. 19 Research indicates that 43 percent of people in SUD treatment for nonmedical use of prescription painkillers have a diagnosis or symptoms of mental health disorders, particularly depression and anxiety. 20
Youth—A Vulnerable Time
Although drug use and addiction can happen at any time during a person’s life, drug use typically starts in adolescence, a period when the first signs of mental illness commonly appear. Comorbid disorders can also be seen among youth. 21–23 During the transition to young adulthood (age 18 to 25 years), people with comorbid disorders need coordinated support to help them navigate potentially stressful changes in education, work, and relationships. 21
Drug Use and Mental Health Disorders in Childhood or Adolescence Increases Later Risk
The brain continues to develop through adolescence. Circuits that control executive functions such as decision making and impulse control are among the last to mature, which enhances vulnerability to drug use and the development of a substance use disorder. 3,24 Early drug use is a strong risk factor for later development of substance use disorders, 24 and it may also be a risk factor for the later occurrence of other mental illnesses. 25,26 However, this link is not necessarily causative and may reflect shared risk factors including genetic vulnerability, psychosocial experiences, and/or general environmental influences. For example, frequent marijuana use during adolescence can increase the risk of psychosis in adulthood, specifically in individuals who carry a particular gene variant. 26,27
It is also true that having a mental disorder in childhood or adolescence can increase the risk of later drug use and the development of a substance use disorder. Some research has found that mental illness may precede a substance use disorder, suggesting that better diagnosis of youth mental illness may help reduce comorbidity. One study found that adolescent-onset bipolar disorder confers a greater risk of subsequent substance use disorder compared to adult-onset bipolar disorder. 28 Similarly, other research suggests that youth develop internalizing disorders, including depression and anxiety, prior to developing substance use disorders. 29
Untreated Childhood ADHD Can Increase Later Risk of Drug Problems
Numerous studies have documented an increased risk for substance use disorders in youth with untreated ADHD, 13,30 although some studies suggest that only those with comorbid conduct disorders have greater odds of later developing a substance use disorder. 30,31 Given this linkage, it is important to determine whether effective treatment of ADHD could prevent subsequent drug use and addiction. Treatment of childhood ADHD with stimulant medications such as methylphenidate or amphetamine reduces the impulsive behavior, fidgeting, and inability to concentrate that characterize ADHD. 32
That risk presents a challenge when treating children with ADHD, since effective treatment often involves prescribing stimulant medications with addictive potential. Although the research is not yet conclusive, many studies suggest that ADHD medications do not increase the risk of substance use disorder among children with this condition. 31,32 It is important to combine stimulant medication for ADHD with appropriate family and child education and behavioral interventions, including counseling on the chronic nature of ADHD and risk for substance use disorder. 13,32
An official website of the United States government
The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you’re on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
The PMC website is updating on October 15, 2024. Learn More or Try it out now .
- Advanced Search
- Journal List
- v.14(11); 2022 Nov

Substance Abuse Amongst Adolescents: An Issue of Public Health Significance
1 School of Epidemiology and Public Health, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Sonali G Choudhari
2 School of Epidemiology and Public Health; Community Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha, IND
Sarika U Dakhode
3 Department of Community Medicine, Dr. Panjabrao Deshmukh Memorial Medical College, Amravati, IND
Asmita Rannaware
Abhay m gaidhane.
Adolescence is a crucial time for biological, psychological, and social development. It is also a time when substance addiction and its adverse effects are more likely to occur. Adolescents are particularly susceptible to the negative long-term effects of substance use, including mental health illnesses, sub-par academic performance, substance use disorders, and higher chances of getting addicted to alcohol and marijuana. Over the past few decades, there have been substantial changes in the types of illegal narcotics people consume. The present article deals with the review of substance abuse as a public health problem, its determinants, and implications seen among adolescents. A systematic literature search using databases such as PubMed and Google Scholar was undertaken to search all relevant literature on teenage stimulant use. The findings have been organized into categories to cover essential aspects like epidemiology, neurobiology, prevention, and treatment. The review showed that substance addiction among adolescents between 12 to 19 years is widespread, though national initiatives exist to support young employment and their development. Research on psychological risk factors for teenage substance abuse is vast, wherein conduct disorders, including aggression, impulsivity, and attention deficit hyperactivity disorder, have been mentioned as risk factors for substance use. Parents' attitudes toward drugs, alcohol, academic and peer pressure, stress, and physical outlook are key determinants. Teenage drug usage has a significant negative impact on users, families, and society as a whole. It was found that a lot has been done to provide correct intervention to those in need with the constant development of programs and rehabilitative centers to safeguard the delicate minds of youths and prevent them from using intoxicants. Still, there is much need for stringent policy and program guidelines to curb this societal menace.
Introduction and background
Drug misuse is a widespread issue; in 2016, 5.6% of people aged 15 to 26 reported using drugs at least once [ 1 ]. Because alcohol and illegal drugs represent significant issues for public health and urgent care, children and adolescents frequently visit emergency rooms [ 2 ]. It is well known that younger people take drugs more often than older adults for most drugs. Drug usage is on the rise in many Association of Southeast Asian Nations, particularly among young males between the ages of 15 and 30 years [ 3 ]. According to the 2013 Global Burden of Disease report, drug addiction is a growing problem among teenagers and young people. Early substance use increases the likelihood of future physical, behavioral, social, and health issues [ 4 ]. Furthermore, recreational drug use is a neglected contributor to childhood morbidity and mortality [ 5 ]. One of the adverse outcomes of adolescent substance use is the increased risk of addiction in those who start smoking, drinking, and taking drugs before they are of 18 years. Moreover, most individuals with Substance Use Disorders begin using substances when they are young [ 6 ]. Substance use disorders amongst adolescents have long-term adverse health effects but can be mitigated with efficient treatment [ 7 ].
Childhood abuse is linked to suicidal thoughts and attempts. The particular mental behavior that mediates the link between childhood trauma and adult suicidal ideation and attempts is yet unknown. Recent studies show teens experiencing suicidal thoughts, psychiatric illness symptoms like anxiety, mood, and conduct disorders, and various types of child maltreatment like sexual abuse, corporal punishment, and emotional neglect that further leads to children inclining toward intoxicants [ 8 ]. Although teen substance use has generally decreased over the past five years, prolonged opioid, marijuana, and binge drinking use are still common among adolescents and young adults [ 9 ]. Drug-using students are more prone to commit crimes, including bullying and violent behavior. It has also been connected to various mental conditions, depending on the substance used. On the other hand, it has been linked to social disorder, abnormal behavior, and association with hostile groups [ 10 ]. Adolescent substance users suffer risks and consequences on the psychological, sociocultural, or behavioral levels that may manifest physiologically [ 11 ]. About 3 million deaths worldwide were caused by alcohol consumption alone. The majority of the 273,000 preventable fatalities linked to alcohol consumption are in India [ 12 ], which is the leading contributor. The United Nations Office on Drug and Crime conducted a national survey on the extent, patterns, and trends of drug abuse in India in 2003, which found that there were 2 million opiate users, 8.7 million cannabis users, and 62.5 million alcohol users in India, of whom 17% to 20% are dependent [ 13 ]. According to prevalence studies, 13.1% of drug users in India are under the age of 20 [ 14 ].
In India, alcohol and tobacco are legal drugs frequently abused and pose significant health risks, mainly when the general populace consumes them. States like Punjab and Uttar Pradesh have the highest rates of drug abuse, and the Indian government works hard to provide them with helpful services that educate and mentor them. This increases the burden of non-communicable illnesses too [ 15 ]. In addition, several substances/drugs are Narcotic and Psychotropic and used despite the act named ‘Narcotic Drugs and Psychotropic Substances Act, 1985.
This review article sheds light on ‘substance abuse’ amongst adolescents as an issue of public health significance, its determinants, and its implications on the health and well-being of adolescents.
Methodology
The present article deals with the narrative review of substance abuse as a public health problem, its determinants, and implications seen among adolescents. A systematic literature search using databases such as PubMed and Google Scholar was undertaken to search all relevant literature on teenage stimulant use. The findings have been organized into categories to cover essential aspects like epidemiology, neurobiology, prevention, and treatment. Various keywords used under TiAb of PubMed advanced search were Stimulants, "Drug abuse", "Psychotropic substance", "Substance abuse", addiction, and Adolescents, teenage, children, students, youth, etc., including MeSH terms. Figure Figure1 1 shows the key substances used by youth.

Reasons for abuse
People may initially choose to take drugs for psychological and physical reasons. Psychological issues, including mental illness, traumatic experiences, or even general attitudes and ideas, might contribute to drug usage. Several factors can contribute to emotional and psychosocial stress, compelling one to practice drug abuse. It can be brought on by a loss of a job because of certain reasons, the death of a loved one, a parent's divorce, or financial problems. Even medical diseases and health problems can have a devastating emotional impact. Many take medicines to increase their physical stamina, sharpen their focus, or improve their looks.
Students are particularly prone to get indulged in substance abuse due to various reasons, like academic and peer pressure, the appeal of popularity and identification, readily available pocket money, and relatively easy accessibility of several substances, especially in industrial, urban elite areas, including nicotine (cigarettes) [ 16 , 17 ]. In addition, a relationship breakup, mental illness, environmental factors, self-medication, financial concerns, downtime, constraints of work and school, family obligations, societal pressure, abuse, trauma, boredom, curiosity, experimentation, rebellion, to be in control, enhanced performance, isolation, misinformation, ignorance, instant gratification, wide availability can be one of the reasons why one chooses this path [ 18 ].
The brain grows rapidly during adolescence and continues to do so until early adulthood, as is well documented. According to studies using structural magnetic resonance imaging, changes in cortical grey matter volume and thickness during development include linear and nonlinear transformations and increases in white matter volume and integrity. This delays the maturation of grey and white matter, resulting in poorer sustained attention [ 19 ]. Alcohol drinking excessively increases the likelihood of accidents and other harmful effects by impairing cognitive functions like impulse control and decision-making and motor functions like balance and hand-eye coordination [ 20 ]. Lower-order sensory motor regions of the brain mature first, followed by limbic areas crucial for processing rewards. The development of different brain regions follows different time-varying trajectories. Alcohol exposure has adversely affected various emotional, mental, and social functions in the frontal areas linked to higher-order cognitive functioning that emerge later in adolescence and young adulthood [ 21 ].
Smoking/e-cigarettes
The use of tobacco frequently begins before adulthood. A worryingly high percentage of schoolchildren between 13 and 15 have tried or are currently using tobacco, according to the global youth tobacco survey [ 22 ]. It is more likely that early adolescent cigarette usage will lead to nicotine dependence and adult cigarette use. Teenage smoking has been associated with traumatic stress, anxiety, and mood problems [ 23 ]. Nicotine usage has been associated with a variety of adolescent problems, including sexual risk behaviors, aggressiveness, and the use of alcohol and illegal drugs. High levels of impulsivity have been identified in adolescent smokers.
Additionally, compared to non-smokers, smoking is associated with a higher prevalence of anxiety and mood disorders in teenagers. Smoking is positively associated with suicidal thoughts and attempts [ 24 ]. Peer pressure, attempting something new, and stress management ranked top for current and former smokers [ 25 ]. Most teenagers say that when they start to feel down, they smoke to make themselves feel better and return to their usual, upbeat selves. Smoking may have varying effects on people's moods [ 26 ]. Teenagers who smoke seem more reckless, less able to control their impulses, and less attentive than non-smokers [ 27 ].
Cannabis/Marijuana
Marijuana is among the most often used illegal psychotropic substances in India and internationally. The prevalence of marijuana usage and hospitalizations related to marijuana are rising, especially among young people, according to current trends. Cannabis usage has been connected to learning, working memory, and attention problems. Cannabis has been shown to alleviate stress in small doses, but more significant amounts can cause anxiety, emotional symptoms, and dependence [ 28 ]. Myelination and synaptic pruning are two maturational brain processes that take place during adolescence and the early stages of adulthood. According to reports, these remodeling mechanisms are linked to efficient neural processing. They are assumed to provide the specialized cognitive processing needed for the highest neurocognitive performance. On a prolonged attentional processing test, marijuana usage before age 16 was linked to a shorter reaction time [ 29 ]. Cannabis use alters the endocannabinoid system, impacting executive function, reward function, and affective functions. It is believed that these disturbances are what lead to mental health problems [ 30 ].
MDMA (Ecstasy/Molly)
MDMA (3,4-methylenedioxy-methamphetamine) was a synthetic drug used legally in psychotherapy treatment throughout the 1970s, despite the lack of data demonstrating its efficacy. Molly, or the phrase "molecular," is typically utilized in powder form. Serotonin, dopamine, and norepinephrine are produced more significantly when MDMA is used. In the brain, these neurotransmitters affect mood, sleep, and appetite. Serotonin also causes the release of other hormones that may cause emotions of intimacy and attraction. Because of this, users might be more affectionate than usual and possibly develop ties with total strangers. The effects wear off three to six hours later, while a moderate dose may cause withdrawal symptoms to continue for a week. These symptoms include a decline in sex interest, a drop in appetite, problems sleeping, confusion, impatience, anxiety, sorrow, Impulsivity and violence, issues with memory and concentration, and insomnia are a few of them. Unsettlingly, it is rising in popularity in India, particularly among teenagers [ 31 ].
Opium
In addition to being a top producer of illicit opium, India is a significant drug consumer. In India, opium has a long history. The most common behavioral changes are a lack of motivation, depression, hyperactivity, a lack of interest or concentration, mood swings or abrupt behavior changes, confusion or disorientation, depression, anxiety, distortion of reality perception, social isolation, slurred or slow-moving speech, reduced coordination, a loss of interest in once-enjoyed activities, taking from family members or engaging in other illegal activity [ 32 ]. Except for the chemical produced for medicinal purposes, it is imperative to prohibit both production and usage since if a relatively well-governed nation like India cannot stop the drug from leaking, the problem must be huge in scope [ 33 ].
Cocaine is a highly addictive drug that causes various psychiatric syndromes, illnesses, and symptoms. Some symptoms include agitation, paranoia, hallucinations, delusions, violence, and thoughts of suicide and murder. They may be caused by the substance directly or indirectly through the aggravation of co-occurring psychiatric conditions. More frequent and severe symptoms are frequently linked to the usage of cocaine in "crack" form. Cocaine can potentially worsen numerous mental diseases and cause various psychiatric symptoms.
Table Table1 1 discusses the short- and long-term effects of substance abuse.
| Substance | Mode | Behavioral changes | Short-term physical effects | Long-term physical effects |
| Alcohol | Oral/drinking | Growingly aggressive self-disclosure racy sexual behavior [ ]. | Unsteady speech, Drowsiness, Vomiting, Diarrhea, Uneasy stomach, Headache, Breathing problems, Vision and hearing impairment, Faulty judgment, Diminution of perception and coordination, Unconsciousness, Anemia (loss of red blood cells), Coma, and Blackouts [ ]. | Unintentional injuries such as car crashes, falls, burns, drowning; Intentional injuries such as firearm injuries, sexual assault, and domestic violence; Increased on-the-job injuries and loss of productivity; increased family problems and broken relationships. Alcohol poisoning, High blood pressure, Stroke, and other heart-related diseases; Liver disease, Nerve damage, Sexual problems, Permanent damage to the brain [ ]. Vitamin B deficiency can lead to a disorder characterized by amnesia, apathy, and disorientation. Ulcers, Gastritis (inflammation of stomach walls), Malnutrition, Cancer of the mouth and throat [ ]. |
| Cannabis | Smoked, Vaped, Eaten (mixed in food or brewed as tea) | Hallucinations, emotional swings, forgetfulness, Depersonalization, Paranoia, Delusions Disorientation. Psychosis, Bipolar illness, Schizophrenia [ ]. | Enhanced sensory perception and euphoria followed by drowsiness/relaxation; Slowed reaction time; problems with balance and coordination; Increased heart rate and appetite; problems with learning and memory; anxiety. | Mental health problems, Chronic cough, Frequent respiratory infections. |
| Cocaine (coke/crack) | Snorted, smoked, injected | Violence and hostility, paranoia and hallucinations, and monotonous or stereotyped simple conduct [ ]. Suspiciousness anger\giddiness Irritability, and Impatience [ ]. | Narrowed blood vessels; enlarged pupils; increased body temperature, heart rate, and blood pressure; headache; abdominal pain and nausea; euphoria; increased energy, alertness; insomnia, restlessness; anxiety; erratic and violent behavior, panic attacks, paranoia, psychosis; heart rhythm problems, heart attack; stroke, seizure, coma. | Loss of sense of smell, nosebleeds, nasal damage and trouble swallowing from snorting; Infection and death of bowel tissue from decreased blood flow; Poor nutrition and weight loss; Lung damage from smoking. |
| Heroin | Injected, smoked, snorted | Exaggerated efforts to keep family members out of his or her room or being secretive about where he or she goes with friends; drastic changes in behavior and relationships with family and friends; sudden requests for money without a good reason; sudden disinterest in school activities or work; a drop in grades or work performance; a lack of energy and motivation; and lack of interest in clothes are all examples of these behaviors [ ]. | Euphoria; dry mouth; itching; nausea; vomiting; analgesia; slowed breathing and heart rate. | Collapsed veins; abscesses (swollen tissue with pus); infection of the lining and valves in the heart; constipation and stomach cramps; Liver or kidney disease; pneumonia. |
| MDMA | Swallowed, snorted | A state of exhilarated tranquility or peace greater sensitivity -More vigor both physically and emotionally -Increased intimacy and sociability -Relaxation -Bruxism -Empathy [ ]. | Lowered inhibition; enhanced sensory perception; increased heart rate and blood pressure; muscle tension; nausea; faintness; chills or sweating; sharp rise in body temperature leading to kidney failure or death. | Long-lasting confusion, Depression, problems with attention, memory, and Sleep; Increased anxiety, impulsiveness; Less interest in sex. |
| Cigarettes, Vaping devices, e-cigarettes, Cigars, Bidis, Hookahs, Kreteks | Smoked, snorted, chewed, vaporized | Hyperactivity Inattention [ ]. Anxiety, Tension, enhanced emotions, and focus lower rage and stress, relax muscles, and curbs appetite [ ]. | Increased blood pressure, breathing, and heart rate; Exposes lungs to a variety of chemicals; Vaping also exposes the lungs to metallic vapors created by heating the coils in the device. | Greatly increased risk of cancer, especially lung cancer when smoked and oral cancers when chewed; Chronic bronchitis; Emphysema; Heart disease; Leukemia; Cataracts; Pneumonia [ ]. |
Other cheap substances ( sasta nasha ) used in India
India is notorious for phenomena that defy comprehension. People in need may turn to readily available items like Iodex sandwiches, fevibond, sanitizer, whitener, etc., for comfort due to poverty and other circumstances to stop additional behavioral and other changes in youth discouragement is necessary [ 42 - 44 ].
Curbing drug abuse amongst youth
Seventy-five percent of Indian households contain at least one addict. The majority of them are fathers who act in this way due to boredom, stress from their jobs, emotional discomfort, problems with their families, or problems with their spouses. Due to exposure to such risky behaviors, children may try such intoxicants [ 45 ]. These behaviors need to be discouraged because they may affect the child's academic performance, physical growth, etc. The youngster starts to feel depressed, lonely, agitated and disturbed. Because they primarily revolve around educating students about the dangers and long-term impacts of substance abuse, previous attempts at prevention have all been ineffective. To highlight the risks of drug use and scare viewers into abstaining, some programs stoked terror. The theoretical underpinning of these early attempts was lacking, and they failed to consider the understanding of the developmental, social, and other etiologic factors that affect teenage substance use. These tactics are based on a simple cognitive conceptual paradigm that says that people's decisions to use or abuse substances depend on how well they are aware of the risks involved. More effective contemporary techniques are used over time [ 46 ]. School-based substance abuse prevention is a recent innovation utilized to execute changes, including social resistance skills training, normative education, and competence enhancement skills training.
Peer pressure makes a teenager vulnerable to such intoxicants. Teenagers are often exposed to alcohol, drugs, and smoking either because of pressure from their friends or because of being lonely. Social resistance training skills are used to achieve this. The pupils are instructed in the best ways to steer clear of or manage these harmful situations. The best method to respond to direct pressure to take drugs or alcohol is to know what to say (i.e., the specific content of a refusal message) and how to say it. These skills must be taught as a separate curriculum in every school to lower risk. Standard instructional methods include lessons and exercises to dispel misconceptions regarding drug usage's widespread use.
Teenagers typically exaggerate how common it is to smoke, drink, and use particular substances, which could give off the impression that substance usage is acceptable. We can lessen young people's perceptions of the social acceptability of drug use by educating them that actual rates of drug usage are almost always lower than perceived rates of use. Data from surveys that were conducted in the classroom, school, or local community that demonstrate the prevalence of substance use in the immediate social setting may be used to support this information. If not, this can be taught using statistics from national surveys, which usually show prevalence rates that are far lower than what kids describe.
The role social learning processes have in teen drug use is recognized by competency-improvement programs, and there is awareness about how adolescents who lack interpersonal and social skills are more likely to succumb to peer pressure to use drugs. These young people might also be more inclined to turn to drug usage instead of healthier coping mechanisms. Most competency enhancement strategies include instruction in many of the following life skills: general problem-solving and decision-making skills, general cognitive abilities for fending off peer or media pressure, skills for enhancing self-control, adaptive coping mechanisms for reducing stress and anxiety through the use of cognitive coping mechanisms or be behavioral relaxation techniques, and general social and assertive skills [ 46 ].
Programs formulated to combat the growing risk of substance abuse
The Ministry of Health and Family Welfare developed Rashtriya Kishor Swasthya Karyakram for teenagers aged 10 to 19, with a focus on improving nutrition, sexual and reproductive health, mental health, preventing injuries and violence, and preventing substance abuse. By enabling them to make informed and responsible decisions about their health and well-being and ensuring that they have access to the tools and assistance they need, the program seeks to enable all adolescents in India in realizing their full potential [ 47 ].
For the past six years, ‘Nasha Mukti Kendra’ in India and rehabilitation have worked to improve lives and provide treatment for those who abuse alcohol and other drugs. They provide cost-effective and dedicated therapy programs for all parts of society. Patients come to them from all around the nation. Despite having appropriate programs and therapies that can effectively treat the disorder, they do not employ medication to treat addiction.
Conclusions
Around the world, adolescent drug and alcohol addiction has significantly increased morbidity and mortality. The menace of drugs and alcohol has been woven deep into the fabric of society. As its effects reach our youth, India's current generation is at high stake for the risk associated with the abuse of drugs like cannabis, alcohol, and tobacco. Even though the issue of substance abuse is complicated and pervasive, various stakeholders like healthcare professionals, community leaders, and educational institutions have access to a wealth of evidence-based research that can assist them to adopt interventions that can lower rates of teenage substance misuse. It is realized that while this problem is not specific to any one country or culture, individual remedies might not always be beneficial. Due to the unacceptably high rate of drug abuse that is wreaking havoc on humanity, a strategy for addressing modifiable risk factors is crucial. Because human psychology and mental health influence the choices the youth make related to their indulgence in drug misuse, it is the need of the hour to give serious consideration to measures like generating awareness, counseling, student guidance cells, positive parenting, etc., across the world. It will take time to change this substance misuse behavior, but the more effort we put into it, the greater the reward we will reap.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
- Subscribe to journal Subscribe
- Get new issue alerts Get alerts
Secondary Logo
Journal logo.
Colleague's E-mail is Invalid
Your message has been successfully sent to your colleague.
Save my selection
Guidance for Writing Case Reports in Addiction Medicine
Oldfield, Benjamin J. MD, MHS; Saitz, Richard MD, MPH
Departments of Medicine and Pediatrics, Yale School of Medicine, New Haven, CT (BJO); Fair Haven Community Health Care, New Haven, CT (BJO); Clinical Addiction Research and Education (CARE) Unit, Section of General Internal, Medicine, Department of Medicine, Boston University School of Medicine and Boston Medical, Boston, MA (RS); Department of Community Health Sciences, Boston University School of Public Health, Boston, MA (RS).
Send correspondence to Benjamin J. Oldfield, MD, MHS, Yale University School of Medicine, 374 Grand Avenue, New Haven, CT 06513. E-mail: [email protected]
Received 20 December, 2019
Accepted 20 December, 2019
The authors report no conflicts of interest.

Methodologically sound interventional and observational studies contribute to knowledge of prognosis, efficacy, effectiveness, and risk. Evidence pyramids place the highest value on systematic reviews and meta-analyses of such studies. 1 These studies do provide generalizable results in populations that can be applied to individuals. But they do not reflect the richness and complexity of individual patient experiences or cases in their contexts. Case reports, although they cannot provide conclusive evidence for efficacy or risk, can provide valuable information of a different type that can impact medicine across several domains.
Case reports:
- (1) can foster clinical reasoning,
- (2) are feasible scholarship for many,
- (3) can serve as an alert to hazards,
- (4) can signal new clinical and service delivery practices, and
- (5) inform health policy.
In medical education, grappling with real cases is a long-lasting way to foster clinical reasoning among trainees in accordance with adult learning theory, 2 so cases often form the bases of grand rounds presentations and standardized test questions. Case reports also are considered a form of practical scholarship for those in training and clinical practice who have frequent occasions to make direct clinical observations, and opportunities for their publication have grown exponentially in recent years. 3 These scholarly reports can alert clinicians and public health agencies to health hazards beyond the reach of clinical trials—eg, vaping and lung injury 4 or the harms of synthetic cannabinoids 5 —and to signals of possibly efficacious new practices that should be tested in more rigorously designed studies. 6,7 They can serve as stimuli for clinical and systems improvement by highlighting challenges and pitfalls in current practice. 8 In health policy, cases capture the minds of voters and lawmakers, informing the allocation of resources based on a combination of facts and the emotional tug of storytelling. Consider Matthew Casey Wethington, who died in 2002 from a heroin overdose at the age of 23, whose story—and the advocacy of his parents—led to Casey's Law in Kentucky that supports involuntary treatment of people with substance use disorders. 9 It is no surprise, then, that cases can play a particularly important role in teaching, studying, generating new knowledge, and advocating for change in addiction medicine, a field whose context is rapidly evolving.
Our experiences editing case report submissions to the Journal of Addiction Medicine have reaffirmed to us the important contributions of case reports to the field of addiction medicine and have also alerted us to their challenges and hazards. Our purpose in this editorial is to identify 4 potential pitfalls of case reports in addiction medicine, and to offer guidance for authors considering writing and publishing case reports in addiction medicine and related fields.
The first potential pitfall emerges from a relative lack of expertise and established standards in case report writing compared to the writing of other scientific articles, for which norms of accuracy, completion, and transparency of reporting have been compiled. 10 The available reviewers for a journal, as well as its editors, may have less experience with case reports than other types of reports. Instruments to assess rigor in case reports are generally lacking, whereas other research approaches such as randomized trials or cohort studies can be systematically assessed for bias and quality via tools like the Cochrane Risk of Bias Tool 11 and the Newcastle-Ottawa Scale, 12 respectively. Such reporting standards ensure completeness and transparency of published reports and facilitate their systematic aggregation.
The second potential pitfall emerges from the sometimes murky distinction between case reports and human subjects research, particularly in scenarios where a new treatment is tried by one or a few patients. How ought consent be obtained in case reports, and when is ethical review (eg, by an institutional review board [IRB] or ethics committee) required? Consent to be the subject of a published case report and consent to participate in a research study are different processes with different guidelines, and authors of case reports may not clearly identify to exactly what the subject(s) consented.
A third pitfall involves a lack of enough information in the report to reliably make substance use disorder diagnoses, assess change over time, or claim effect of an intervention. Internal validity in case reports depends on the triangulation of multiple forms of data, such as clinical history, physical exam findings, and biochemical testing. 13 Given the care fragmentation experienced by many people with addiction and other comorbid conditions, 14,15 whereby primary care services, addiction services, and the management of other conditions may occur in different institutions, data triangulation can be logistically difficult for authors of case reports just as it is for clinicians. Data triangulation can be further complicated by federal regulations specific to addiction medicine, such as Title 42 of the Code of Federal Regulations Part 2, which controls the release of patient information about treatment for substance use disorders. 16 Furthermore, patients with substance use disorders are subject to overlapping forms of stigma, discrimination, and power relations with health care providers 17 , which may impact their reachability by clinicians seeking to verify or collect additional information for the construction of a case report.
A final pitfall is a structural and stylistic one. Unlike other types of scientific articles, case reports do not have specific aims or hypotheses so readers searching for a “take-home point” may not find one as easily as they might while reading other articles. Therefore, without clear statements of the reason for reporting the case, and efforts towards contextualizing the report in the medical literature, it can be unclear to editors and to readers what is novel about the report and how it should inform readers’ thinking about a clinical or systems problem.
Bearing in mind the unique potential pitfalls and strengths for case reports in addiction medicine, we propose the following ethical, reporting, and writing guidance for those writing and publishing them ( Table 1 ).

1. Obtain consent and state clearly in the report what was obtained (eg, written consent was obtained from the patient to report their case in the medical literature). Accepted standards of consent, such as those supported by the International Committee of Medical Journal Editors (ICMJE), should be adhered to. 18 Consent guidelines specific to case reports, such as those presented by the Committee on Publication Ethics (COPE), can guide writers. 19 While individual journals may vary in their guidance to authors regarding the format in which consent should be obtained, the ICMJE and COPE generally recommend written consent to report the case and that the subjects of the report approve the final manuscript if any potentially identifying information is presented.
Authors of case reports need not consider consent to be a one-off, but an ongoing process that may include multiple points of contact between the writers of the case report and its subject(s). 20 At the least, agreement between subject(s) and author(s) as to the decision to write the report as well as approval of its submission should be documented in the report. More than consent, seeking feedback from patients during manuscript preparation can raise the voices of marginalized persons and help disseminate their perspectives. 21,22 In cases where consent cannot be obtained, reasonable efforts in multiple modalities (such as in-person outreach, phone, internet search, or mail) to obtain consent should be documented in the report. In these situations, the authors should explain their reasoning for not obtaining consent and their efforts to do so, they should minimize identifiable features in the report, and the authors (and editors) should attempt to balance the risk of deductive disclosure with the benefit of the case report to public health and science. For example, an identifiable case report (with associated disclosure risks) with little impactful content should not be published (without consent). An anonymous case that has great value could be published without consent after extraordinary efforts to obtain consent failed.
2. Obtain IRB/ethics committee review if appropriate. Authors should reflect on whether their project constitutes human subjects research, and if it may, ethics review by an IRB should be performed and documented in the report. While consent to report a case and consent to participate in research are not the same, the former is always needed for case reports. The latter is needed when there has been human subjects research that requires consent. IRB review is required when the activity is human subjects research, whose definition is widely accepted to include any research involving a living individual about whom data (including private information) or biospecimens are obtained systematically for research purposes to generate new, generalizable knowledge. 23 Therefore, a trial of a new treatment in a single patient with such intent would require review by an IRB. However, a report of a clinical case, in which no information was collected solely for research purposes but was instead done so for clinical care, and no new therapy was trialed, would not. When more than one patient is the focus of the report (which thus constitutes a case series), IRB review is more strongly encouraged. Several major research institutions have concluded that a case series involving greater than three patients ought to undergo IRB review because they are more likely to meet the definition of research as a systematic investigation. 23
For the sole benefit of a patient, clinicians sometimes try new treatments. Such cases might be reported retrospectively as case reports if the initial intent did not include systematic evaluation to generate generalizable knowledge. However, to avoid any confusion regarding whether a new treatment is research or not, we strongly encourage IRB review and approval of any new treatments delivered whose results might be reported with the intent to generalize the findings in a case report. Such new treatments for clinical purposes may also come under Food and Drug Administration (FDA) “single patient expanded access” or “emergency use” regulations for which there are specific IRB and FDA procedures. 24 When drugs are used off-label or with novel dosing strategies in a patient for whom clinicians prospectively decide to collect and report outcomes, these clinicians should consult the FDA's guidelines regarding whether an investigational new drug application (IND) is warranted. 25
3. Triangulate data from multiple sources to minimize threats to internal validity. 26 For example, substance use can be documented by history as well as by body fluid testing, and substance use disorders and their severity can be diagnosed based on criteria established by the Diagnostic and Statistical Manual, 5th revision. 27 Authors should also state how they assessed for diagnostic criteria, for example, via checklists or other instruments, structured interview, and/or a clinical examination. Case reports in addiction medicine that do not include laboratory testing of substances often have limited value.
4. Characterize the relationship between author(s) and subject(s) to clarify potential bias and allow readers to interpret power relationships between writers and subjects. 26 Who solicited historical information, and who obtained informed consent from the patient and at which time periods during the unfolding of the case should be clear to readers so they may determine if internal validity is threatened by bias related to social desirability or coercion.
5. Use reporting standards and structure the report. Cite the standard(s) to which the report adheres. We suggest using internationally accepted reporting standards for case reports. 28 Corresponding checklists ought to be made available to editors on request.
Case reports should have an introduction, the report itself, and a discussion of the case's implications. Introductions to case reports can offer up-to-date, concise reviews of the literature that educates readers about the topic and justifies the need for sharing the case. The justification may address the novelty or uniqueness of the case (eg, a rare disease or rare presentation) or its relationship to a contemporary phenomenon (eg, a success or failure of a feature of a care system, or demonstration of how to apply evidence from a clinical trial). After the case is presented, a discussion should follow that integrates the case in the larger context of what is known on the topic. If hypotheses are generated by the case, they may represent opportunities for future research and these should be stated. In stating a “take-home point,” authors should avoid drawing firm conclusions regarding efficacy or harm given the methodological limitations of the case report. Limitations in drawing conclusions and threats to internal validity should be stated clearly for readers. Strengths should also be noted (eg, the use of biological fluid testing). The discussion section may also include a perspective from the patient(s).
6. Use non-stigmatizing, person-centered language so that the case report may reduce, and not perpetuate, the stigma embodied in certain outdated terms (eg, addict, abuse) that can influence providers’ attitudes and behaviors. 29 Authors are encouraged to reference the statement made by the International Society of Addiction Journal Editors that refers to the destigmatization of language surrounding addiction. 30
William Osler, a foundational figure in clinical practice and medical education, is credited with many famous pearls, including “the good physician treats the disease; the great physician treats the patient who has the disease.” Case reports shift our gaze from the disease to the patient, and in so doing, can help identify novel disease presentations, successes and failures of health systems, and share the experiences of vulnerable patients. As the field of addiction medicine—as well as its legal, cultural, and policy milieu—evolve, case reports represent an opportunity to inform clinical practice, research, and policy. We hope that those who study and treat patients with substance use disorders will take advantage of this form of inquiry and dissemination of knowledge and, in so doing, will encourage readers to take more thoughtful and person-centered approaches to addiction medicine and related fields.
- Cited Here |
- Google Scholar
- + Favorites
- View in Gallery
Readers Of this Article Also Read
The asam national practice guideline for the treatment of opioid use disorder:..., treatment of kratom withdrawal and dependence with buprenorphine/naloxone: a..., low dose buprenorphine induction with full agonist overlap in hospitalized..., management of xylazine withdrawal in a hospitalized patient: a case report, grief at the heart of the opioid overdose crisis: past lessons and present....
- Continuing Education
- Practice Tools
- Partnerships
- Interest Form
- Case Studies
- MyU : For Students, Faculty, and Staff
Co-occurring Mental Health and Substance Use Disorders: Guiding Principles and Recovery Strategies in Integrated Care (Part 1)
Individuals with co-occurring mental health and substance use disorders (CODs) have complex treatment needs. Historically, these issues were treated separately, as competing discreet needs. Barriers in access to integrated care for substance related and mental health disorders prevented many individuals from finding relief from their COD. The structures in place that prevented integrated care were many. Public and private funding, research, and public policy all created troughs between disciplines of care. Researchers and practitioners have noted how the separation of mental health and substance abuse treatment has created additional barriers and obstacles for clients with CODs: Parallel treatment results in fragmentation of services, non-adherence to interventions, dropout, and service extrusion, because treatment programs remain rigidly focused on single disorders and individuals with dual disorders are unable to negotiate the separate systems and to make sense of disparate messages regarding treatment and recovery (Osher, Drake, 1996; Drake, Mueser, Brunette, and McHugo. 2004).
Mental health services and treatment structures for substance related disorders were on divergent paths and many professionals considered one another with skepticism. Today, some, but not all, of those barriers have been eliminated.
According to the Substance Abuse and Mental Health Services Administration’s (SAMHSA) 2011 National Survey on Drug Use and Health, Mental Health Findings, more than 8 million adults in the United States have CODs. Only 6.9% of individuals receive treatment for both conditions and 56.6% receive no treatment at all (SAMHSA, 2012).
This is the first of two practice briefs that will explore eight principles of integrated care for CODs (Mueser et al., 2003). This brief will examine the first four of the following principles:
- Principle 1: Integration of mental health and substance use services
- Principle 2: Access to comprehensive assessment of substance use and mental health concerns
- Principle 3: Comprehensive variety of services offered to clients
- Principle 4: An assertive approach to care/service delivery
- Principle 5: Using a harm reduction approach to care
- Principle 6: Motivation-based and stage wise interventions
- Principle 7: Long-term perspective of care
- Principle 8: Providing multiple psychotherapeutic modalities
After a brief review of each principle, an illustrative case study will be provided and suggestions for implementing each of the principles in a client session will be offered (SAMHSA, 2009a; 2009b).
Principle 1: Integration of Mental Health and Substance Use Services
Multidisciplinary teams provide integrated services and relevant care that is client centered and longitudinal in nature. Agency policies and practices recognize the relapse potential with CODs and do not penalize clients for exhibiting symptoms of their mental health or substance related disorders. Team members may include the client and their family members or supportive persons, practitioners who are trained in substance abuse and mental health counseling, and a combination of physicians, nurses, case managers, or providers of ancillary rehabilitation services (therapy, vocational, housing, etc.) such as social workers, psychologists, psychiatrists, marriage and family therapists and peer support specialists. Based on their respective areas of expertise, team members collaborate to deliver integrated services relevant to the client’s specific circumstances, assist in making progress toward goals, and adjust services over time to meet individuals’ evolving needs (Mueser, Drake, & Noordsy, 2013). The team members consistently and regularly communicate with the client to discuss progress towards goals, and they work together to meet the individual treatment needs of each client.
Penny, 43, experienced her first depressive episode in her mid teens. During her first treatment for substance use (marijuana and alcohol) at age 17, Penny was diagnosed with attention deficit hyperactivity disorder (ADHD). However, over the next few years, she became increasingly edgy and irritable with intermittent periods of euphoria, accelerated energy and impulsive behaviors followed by periods of despair. She had repeated hospitalizations and concurrent and sequential contact with both mental health and substance abuse treatment systems over the years. Penny was labeled with a variety of diagnoses, including bipolar disorder, ADHD, major depression, anxiety disorder, borderline personality disorder, and chemical dependence.
Penny’s multi-disciplinary team consisted of her primary practitioner who held LADC/LPCC dual licenses, a primary care physician, a psychiatrist, a family therapist, a peer recovery support specialist, and a vocational specialist. Penny participated in individual therapy as well as recovery skills groups with her primary practitioner. Her primary care physician monitored Penny’s physical concerns including her diabetes and hypothyroid disorder. Penny’s psychiatrist prescribed and monitored Penny’s mood-stabilizing medications and provided case consultation to Penny’s team. The family therapist provided ongoing support to Penny and her boyfriend Don, and helped Penny and her team decide if and when to begin reparations in her relationship with her children. In addition, the family therapist provided feedback to the team about how Penny’s relationships impacted her recovery status and overall stability. The vocational specialist acted as a resource for Penny once she expressed a desire to return to work, helped Penny and her team identify resources for employment, and acted as liaison with Penny’s employer. The peer recovery support specialist helped Penny identify recovery support groups and helped Penny and her team identify barriers and resources to overcome those barriers to recovery success.
Principle 2: Access to Comprehensive Assessment of Substance Use and Mental Health Concerns
Integrated care recognizes that CODs and the resulting consequences of those conditions are commonplace. Therefore, practice protocols that standardize comprehensive biopsychosocial assessments are essential to identifying major mental illnesses and substance use. A comprehensive assessment includes screening, and when needed, further examination of substance use and mental health concerns. Practitioners utilize information collected from the comprehensive assessment to provide recommendations for treatment —such as the role one condition has on the efficacy of particular treatment strategies for the other condition(s). Screening tools for substance related disorders can include the CAGE-AID (Brown & Rounds, 1995), the Michigan Alcohol Screening Test (MAST) (Selzer, 1971), the Drug and Alcohol Screen Test (DAST) or the Alcohol Use Disorders Identification Test (AUDIT) (Saunders et al., 1993). For mental health concerns the Global Appraisal of Individual Needs-Short Screener (GAIN-SS) (Dennis, Chan, & Funk, 2006), or Brief Symptom Inventory (BSI) (Derogatis & Melisaratos, 1983) may be used.
When feasible, the practitioner gathers information from the client’s family and other professional resources who might have relevant information regarding symptom severity, substance use, and role functioning. Information gathered during the initial assessment can assist in a collaborative goal setting process. Ongoing assessment is critical in the treatment of co-occurring disorders and involves evaluation of changes in circumstances, substance use, stability and symptom expression, and goal attainment. Conducting a comprehensive integrated assessment helps define areas that can be addressed in treatment and identify specific treatment recommendations (Mueser et al., 2013). The context of the comprehensive assessment should occur within a recovery-oriented perspective. Progress toward recovery is individualized as described in the following definition: A process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential (SAMHSA, CMHS, 2011).
Penny and her primary practitioner completed a comprehensive biopsychosocial assessment that included questions about distressing mental health symptoms as well as substance use patterns and periods of abstinence/remission. During her early 20s Penny entered college to become a nurse. Soon after beginning school, her anxiety increased. She experienced racing thoughts, extreme irritability, interruptions in sleep and a pronounced overconfidence followed by periods of despair and an inability to get out of bed. Penny returned to using alcohol and marijuana and eventually discontinued her education.
In her early 30s, Penny completed substance abuse treatment and was abstinent from alcohol and marijuana. She also participated in individual therapy and was prescribed lithium. She experienced a period of relative stability and returned to school. However, Penny disliked the side effects of her medication and felt she was stable enough to discontinue taking the lithium. She sought care from a physician for her anxiety and was placed on the benzodiazepine Xanax.
Penny currently lives with Don, her boyfriend of 8 years. Due to chronic conflict in their relationship, she is in danger of becoming homeless. Don has a construction business and manages to make a solid living. They both smoke marijuana most evenings as a way to wind down from the day. Don occasionally uses cocaine and in very rare situations Penny has joined him. She has been abstinent from alcohol since receiving a DWI 9 months ago. Penny has been estranged from her two adult children, Linda, 24, and Jeff, 22, for 6 months and 3 years, respectively. Her parents are deceased.
Penny’s practitioner was able to collect information from Penny’s boyfriend, her children, previous therapists, agencies and hospitals with whom she has had contact. During the assessment the practitioner discovered information about periods of increased mental illness symptoms while Penny was abstinent from substances, and a return to substance use in correlation with mental illness symptoms. The comprehensive assessment provided initial information about Penny’s current mental illness symptoms and substance use and was used to determine treatment priorities and programs that align with Penny’s needs.
Principle 3: Comprehensive Variety of Services Offered to Clients
Clients are provided with comprehensive integrated services that are cohesive, relevant and responsive to their identified needs and goals (Bipolar Disorder, n.d.). Practitioners coordinate with one another and collaborate with the client to prioritize treatment needs in a manner that does not overwhelm the client. A multidisciplinary team provides support for a broad range of issues relevant to the client population served by the agency. This includes culturally relevant information about community support systems and an array of mental health or substance related resources available to clients and their support persons.
Comprehensive services that are relevant to persons with CODs often include but are not limited to: medication assisted therapy, cognitive behavioral therapy (CBT), family therapy, life skills/ psychosocial rehabilitation, psychoeducation, and supported employment. Medication assisted therapy helps control distressing symptoms of many health and mental health dis-orders and is helpful for mood stabilization. Medication is also used in the treatment of substance use disorders to inhibit substance use, reduce cravings, reduce withdrawal symptoms, and as replacement therapy. CBT helps people with CODs learn to change harmful or negative thought patterns and behaviors.
Family therapy enhances coping strategies and focuses on improving communication and problem solving amongst family members and significant others. Life skills/rehabilitation provides clients with new information and opportunities to practice skills such as sleep hygiene practices, self-care, stress reduction and management, and medication maintenance. Psychoeducation provides information about the interacting dynamics of CODs and treatment (e.g., recognition of early signs of relapse so they can seek support before a full-blown episode occurs.) Supported employment provides opportunities for the client to contribute meaningfully in a work environment. A vocational specialist is part of the treatment team and works as a liaison with employers, client and the rest of the treatment team to support the client in the work environment. A case manager/navigator assists the client and their support persons in access-ing resources necessary to their recovery. These relationships are longitudinal in nature and supportive rather than therapeutic.
Penny and her treatment team agreed that she would benefit from mood stabilizing medication for her mental health disorder as well as cognitive behavioral therapy to help her develop coping strategies to help regulate and stabilize symptoms such as feelings of despair, racing thoughts, and behavioral dysregulation. Penny and Don recently began family counseling to explore the role and impact of substance use on their relationship, to develop communication skills and to identify strategies to help Don support Penny in her recovery from COD. Penny expressed interest in mending the relationship with her children in the future. If they are reunited, Penny identified a goal of attending family therapy with her children to improve communication and explore the impact of her COD on her relationship with them. Penny also identified a desire to return to work and will be making an appointment to discuss her work goals with the supported employment specialist.
Penny participates in a skills group to assist her in managing the symptoms of her CODs such as emotional and behavioral regulation, self care, sleep hygiene, and to manage triggers related to her substance use.
Principle 4: An Assertive Approach to Care/Service Delivery
Assertive outreach involves reaching out to individuals who are at risk or in crisis and their concerned persons, by providing support and engaging them in the change process. Sometimes this occurs by engaging the individual who seeks care for a substance use issue and providing services that stabilize a COD. An assertive approach is time unlimited and occurs in a variety of situations, including a client’s own community setting (Bond, 1991; Bond, McGrew, & Fekete, 1995). Assertive outreach includes meeting the client in community locations and providing practical assistance in daily living needs. These strategies increase or decrease in intensity depending on the client’s day-to-day living needs such as housing, transportation, money management, or seeking employment. This approach also provides opportunities to explore and address how substance use interferes with goal attainment.
Assertive outreach by Penny’s multidisciplinary team included meeting with a vocational specialist to assist Penny in looking for a job. Penny’s primary practitioner met with Penny weekly in Penny’s home and discussed progress towards her goals. Although Penny had not declared she wanted to stop using or cut down this provided Penny’s practitioner with an opportunity to introduce discrepancy by exploring how substance use interfered with taking steps toward Penny’s goals and practicing or using coping skills. Penny and her primary practitioner examined how Penny’s use impeded her ability to follow through with completing job applications and job interviews as steps toward finding steady, meaningful work.
This brief examined four of the eight principles of COD treatment. The first four principles underscore the importance of the integration of COD services and access to comprehensive assessment and care using assertive outreach and a client centered approach. The next brief will explore the latter four COD principles and implementation strategies. The final COD principles emphasize a long-term care model using a harm-reduction approach, motivation-based stage-wise treatment interventions and multiple treatment modalities (Mueser et al., 2003). The principles in both briefs place the client and their support persons, front and center as active participants, guides, resources and experts in their own recovery. Unpacking the principles of integrated treatment for CODs provides opportunities for practitioners to utilize multiple strategies to engage clients in treatment as discussed in this practice brief.
As you consider the practice of integrated care, examine your agency and your own clinical practice. Consider how you might try new strategies in an effort to implement the principles of COD treatment. We invite practitioners to engage in a dialogue surround-ing the strategies implemented in sessions to engage COD clients. Please consider the following and email us to describe successful COD strategies and challenges utilizing the principles of COD treatment.
- What strategies have you tried using one of the above principles that worked particularly well?
- What challenges have you encountered?
- Please provide suggestions for additional strategies you found helpful.

COMMENTS
Case Study: Lorrie. Figure 1. Lorrie. Lorrie Wiley grew up in a neighborhood on the west side of Baltimore, surrounded by family and friends struggling with drug issues. She started using marijuana and "popping pills" at the age of 13, and within the following decade, someone introduced her to cocaine and heroin.
Wakeman, SE, Pham-Kanter, G, Donelan, K. Attitudes, practices, and preparedness to care for patients with substance use disorder: results from a survey of general internists. Subst Abus 2016;37: ...
Alcohol use was reported in 5.02%, tobacco in 3. 21% and sedative- hy pnotics in 0.04% respondents. Th e study also r eveals. increasing u se o f substan ces among females: substance abuse was ...
Many studies have been conducted on cannabis, nicotine, and other dependencies; however, many others concentrate on alcohol, when investigating the co-occurrence of alcohol and substance use disorder (ASUD) and SAD . It is widely acknowledged that people with SAD will more likely be the consumers of alcoholic beverages and/or abuse drugs.
This case is first of the kind depicting clinical features as well as withdrawal of combined volatile and moderate alcohol abuse. The feature of combined intoxication of the two abused substances makes it difficult for the clinician to reach a diagnosis. Our case report thus puts forward the scenario of increasing combined alcohol and volatile ...
Substance Use Disorder in the U.S. 11.7% of Americans 12 and over use illegal drugs. 53 million or 19.4% of people 12 and over have used illegal drugs or misused prescription drugs within the last year. If alcohol and tobacco are included, 165 million, or 60.2% of Americans ages 12 years or older currently abuse drugs.
In this article, a case-based format is used to address complex clinical issues in addiction medicine. The cases were developed from the authors' practice experience, and were presented at the American College of Medical Toxicology Addiction Academy in 2015. Section I: Drug and Alcohol Dependence and Pain explores cases of patients with co ...
Substance use disorders are no longer split into abuse and dependence but rather are specified by course and severity. Each case vignette is titled with the presenting problem. The cases are formatted similarly throughout and include history of present illness, collateral information, past psychiatric history, social history, examination, any ...
ubstance Abuse Treatment Client With Borderline Personality DisorderMing L., an Asian female, was 32 years old when. she was taken by ambulance to the local hospital's emergency room. Ming L. had taken 80 T. lenol capsules and an unknown amount of Ativan in a suicide attempt. Once medically stable, Ming L. was evaluat.
Minnesota Adult and Teen Challenge (MNTC) is an addiction treatment center. The reason for this qualitative case study was to discover why clients of substance use disorder treatment programs believe that they can graduate from their program when 50% of those who start the same long-term program drop out. This case study focused on graduates from MNTC in Minneapolis, Minnesota. This study ...
This study aimed to describe the adverse effects that adolescent substance abuse has on the levels of care giving and well-being of families. The researchers used a qualitative case study design which focused on an issue of concern (such as adolescent substance abuse) and thus selected one case to elucidate the issue, i.e., a single case study.
The numbers for substance use disorders are large, and we need to pay attention to them. Data from the 2018 National Survey on Drug Use and Health suggest that, over the preceding year, 20.3 million people age 12 or older had substance use disorders, and 14.8 million of these cases were attributed to alcohol.When considering other substances, the report estimated that 4.4 million individuals ...
SAMHSA's mission is to lead public health and service delivery efforts that promote mental health, prevent substance misuse, and provide treatments and supports to foster recovery while ensuring equitable access and better outcomes.
The journal publishes case studies or case report, commentary, editorials, letters to the editor, describing original contents in the fields of medical and life sciences. A Case Study of Adolescent Substance Misuse: A Successful Application of the Adolescent Community Reinforcement (A-CRA) approach in an Irish context
Approximately 12% of surveyed teens indicated "severe" substance use disorder, defined by this study as reporting six or more symptoms. Among this group, more than 60% exhibited at least two symptoms of substance use disorder in adulthood - an association found across alcohol, cannabis, and other drug use disorders.
Case Study Details. Richard is a 62-year-old single man who says that his substance dependence and his bipolar disorder both emerged in his late teens. He says that he started to drink to "feel better" when his episodes of depression made it hard for him to interact with his peers. He also states that alcohol and cocaine are a natural part ...
CSWE Practitioner Education in Substance Use Disorders | Case Study Analysis 3 Case Study Analysis General Instructions Managing personal biases and using a strengths-based perspective, describe your approach to working with the client. Please use person-first, nonstigmatizing language throughout. (C1) Engagement and Assessment
This is a retrospective case-control study of electronic health records (EHRs) data of 73,099,850 unique patients, of whom 12,030 had a diagnosis of COVID-19. ... or of "Substance abuse ...
Many individuals who develop substance use disorders (SUD) are also diagnosed with mental disorders, and vice versa.2,3 Although there are fewer studies on comorbidity among youth, research suggests that adolescents with substance use disorders also have high rates of co-occurring mental illness; over 60 percent of adolescents in community-based substance use disorder treatment programs also ...
Efficacy of CBT for SUDs. Evidence from numerous large scale trials and quantitative reviews supports the efficacy of CBT for alcohol and drug use disorders.[4, 5] For example, our group conducted a meta-analytic review of CBT for drug abuse and dependence including 34 randomized controlled trials (with 2,340 patients treated) and found an overall effect size in the moderate range (d = 0.45 ...
Introduction and background. Drug misuse is a widespread issue; in 2016, 5.6% of people aged 15 to 26 reported using drugs at least once [].Because alcohol and illegal drugs represent significant issues for public health and urgent care, children and adolescents frequently visit emergency rooms [].It is well known that younger people take drugs more often than older adults for most drugs.
Although a significant proportion of adults recover from substance use disorders (SUDs), little is known about how they reach this turning point or why they stop using. The purpose of the study was to explore the factors that influence reasoning and decision making about quitting substance use after a long-term SUD. Semistructured interviews were conducted with 18 participants, each of whom ...
Specific Guidance for Writing Case Reports in Addiction Medicine. 1. Obtain consent and state clearly in the report what was obtained (eg, written consent was obtained from the patient to report their case in the medical literature). Accepted standards of consent, such as those supported by the International Committee of Medical Journal Editors ...
Team members may include the client and their family members or supportive persons, practitioners who are trained in substance abuse and mental health counseling, and a combination of physicians, nurses, case managers, or providers of ancillary rehabilitation services (therapy, vocational, housing, etc.) such as social workers, psychologists ...
How would you diagnose and treat a 54-year-old man with alcohol withdrawal and altered mental status? Read this case challenge and test your knowledge.