

StudyGuider
Your shopping cart is empty!
NRNP 6552 Discussions plus Case Study Discussions Week 1, 3, 4, 5, 7, 8 and 9

NRNP 6552 Week 1 Discussion: Different Roles of the Nurse Practitioner (2 Versions)
NRNP 6552 Week 3 Case Study Discussion: Gynecologic Health
NRNP 6552 Week 4 Case Study Discussion: Common Gynecologic Conditions, Part I
NRNP 6552 Week 5 Case Study Discussion: Common Gynecologic Conditions, Part 2
NRNP 6552 Week 7 Discussion: Health Conditions and Implications for Women
NRNP 6552 Week 8 Case Study Discussion: Common Health Conditions with Implications for Women
NRNP 6552 Week 9 Case Study Discussion: Working Through Ethical Dilemmas and Other Issues in Advanced Nursing Practice
- Description
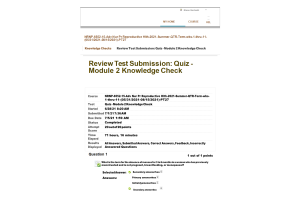
| Course | NRNP 6552 Advanced Nurse Practice in Reproductive Health Care |
| Submitted | Year 2022 |
| Contributed | Martinez |
Related Products

NRNP 6552 Week 1 Assignment; Taking a Health History

NRNP 6552 Week 1 Discussion; Introduction and Professional Interests
NRNP 6552 Week 2 Knowledge Check
NRNP 6552 Week 5 Knowledge Check
NRNP 6552 Week 8 Knowledge Check

NRNP 6552 Week 2 Forum-Case Study

NRNP 6552 Week 4 Forum-Case Study; STI Investigation

NRNP 6552 Week 5 Case Study
NRNP 6552 Week 6 MidtermFall Session
NRNP 6552 Week 6 Midterm
NRNP 6552 Week 6 Midterm Answers
NRNP 6552 Week 6 Midterm Solutions

NRNP 6552 Week 11 Final Exam

NRNP 6552 Week 10 Knowledge Check20 out of 20 Points (Spring QTR)
NRNP 6552 Week 10 Knowledge Check (20 out of 20 points)

NRNP 6552 Week 5 Case Study; Common Gynecologic Conditions - HJ is a 26-year-old
NRNP 6552 Week 5 Knowledge Check (Module 2)

NRNP 6552 Week 7 Discussion; Health Conditions and Implications for Women

NRNP 6552 Week 8 Case Study; Common Health Conditions with Implications for Wome

NRNP 6552 Week 9 Case Study; Working Through Ethical Dilemmas and Other Issues i

NRNP 6552 Week 9 Case Study; Second case study involving a 14-year-old Caucasian
NRNP 6552 Week 10 Knowledge Check (20 out of 20 points; Spring QTR)

NRNP 6552 Week 1 Assignment; Taking a Health History; Building a Health History;

NRNP 6552 Week 1 Discussion; Different Roles of the Nurse Practitioner

NRNP 6552 Week 2 Assignment; Taking a Health History; Building a Health History;
NRNP 6552 Week 3 Case Study 1; Gynecologic Health Charlene Baja
NRNP 6552 Week 3 Case Study 2; Contraception Elaine Goodwin

NRNP 6552 Week 4 Case Study 2; Common Gynecologic Conditions, Part 1 - STI Inves
NRNP 6552 Week 4 Case Study; Common Gynecologic Conditions, Part 1 - Missing Per

NRNP 6552 Week 5 Case Study; Common Gynecologic Conditions, Part 2
NRNP 6552 Exams; Quiz-Knowledge Check, Midterm Exam, Final Exam
NRNP 6552 Quiz-Knowledge Check Week 2, 5, 8 and 10

NRNP 6552 Complete Course Week 1 - 11


NRNP 6552 Course Assignments Week 1, 2, 3, 4, 5, 8 and 9
NRNP 6552 Week 8 Knowledge Check Module 3 (20 out of 20 Point)

NRNP 6552 Week 11 Final Exam Review
NRNP 6552 Week 2 Knowledge Check; Module 1 (20 out of 20 Point Spring QTR)
NRNP 6552 Week 2 Knowledge Check; Module 1 (20 out of 20 Point Spring QTR )
Pardon Our Interruption
As you were browsing something about your browser made us think you were a bot. There are a few reasons this might happen:
- You've disabled JavaScript in your web browser.
- You're a power user moving through this website with super-human speed.
- You've disabled cookies in your web browser.
- A third-party browser plugin, such as Ghostery or NoScript, is preventing JavaScript from running. Additional information is available in this support article .
To regain access, please make sure that cookies and JavaScript are enabled before reloading the page.

- Log in ▼
- Our Guarantees
- Our Services
- How it Works
NRNP 6552: Advanced Nurse Practice in Reproductive Health Care
Week 1: health and health promotion.
Much like archaeologists sift through sand to identify artifacts of interest, nurse practitioners must devote time and effort to interviewing patients, sifting through facts to identify relevant information that can be pieced together to create a relevant patient history. These efforts have their own unique challenges and approaches based on the characteristics of the patient, including sex, age, culture, and more.
Female patient interviews have their own unique characteristics. Sensitive matters related to sexual health, physical and/or emotional abuse, pregnancy, menstruation, and other topics may leave patients uncomfortable and create challenges to productive conversations NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
For this week, you will examine the role of the patient interview in health promotion. You also will practice approaches to building a patient history by interviewing a volunteer by creating a script which you use to conduct a mock patient interview with the volunteer.
Learning Objectives
Students will:
- Analyze professional interests of study
- Analyze the different roles related to the a CRNP (certified registered nurse practitioner), a CNM (certified nurse midwife), and a PA (Physician Assistant)
- Create scripts for taking a health history to include difficult questions
- Develop patient health histories related to difficult questions
*These Learning Objectives are introduced this week and assessed in Week 2 NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
- Learning Resources
Discussion: Different Roles of the Nurse Practitioner
The term ‘history” is broad in meaning. Within that broad framework archeologists tend to focus their careers on various specialties and areas of interest, such as specific historical eras or geographical areas.
So it is with nurses. Within the broad framework of healthcare, nurse practitioners focus their careers on various roles. These roles may in part be based on narrower areas of interest such as women’s health. Careers also focus on selected technical nursing specialties NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.

Photo Credit: Getty Images/Blend Images
For this Discussion, you will explore your professional interests and those interests are addressed in specific guidelines and competencies. You also examine the different nurse practitioner roles related to women’s health and how these roles might impact the way you work.
To prepare:
- Review the modular structure of this course and reflect on how each module defines the specific skills needed as an advanced Nurse Practitioner (NP).
- Review the ANA guidelines, NP competencies, and the Ethic resources found in this week’s Learning Resources and consider how they impact the work of the NP.
Post a brief explanation about the differences in roles related to a CRNP, a CNM, and a PA and how each of these roles might impact the how you practice as a FNP. Be specific and provide examples.
Read a selection of your colleagues’ responses.
Providers present with many different education backgrounds. Some credentials one may see within a women’s health care setting include: certified registered nurse practitioner (CRNP) or advanced practice nurse practitioner (APNP), certified nurse midwife (CNM) and physician’s assistant (PA). This discussion will look at the different roles of an individual based on their educational background NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
When looking at providers one area to discuss includes scope of practice. For nurse practitioners (NPs) in the United States, state level practicing laws vary from state to state despite educational preparation for independent patient care, prescribing practices and diagnostic procedures (Poghosyan, Liu, & Norful, 2017, Kraus & DuBois, 2017). The scope of practice for an NP in Ohio falls under a reduced practice. APNPs, including a CNM, in the state of Ohio must collaborate with a licensed physician with a written agreement for prescribing practices per the Ohio Revised Code (NCSL, 2021, McCleery, et al., Freeman, 2019). Limitations for CNM is also addressed in the state laws. For example, a CNM in Ohio is unable to deliver breech babies or perform version (Legislative Service Commission, 2020). Prescribing practices and scope of practice for PAs also differs in the Ohio revised Code. A supervision agreement between the PA and an appropriate physician that addresses prescriptive authority for schedule II-V controlled substances along with a scope of practice agreed upon by both parties must be submitted to the State Medical Board (NCSL, 2021). As an advanced practice provider, it is important to know the scope of practice within the state, practicing guidelines within the facility, and the agreement with the supervising physician.
Another difference in these three provider roles includes their approach to care. An individual who takes the nursing path, such as a CNM or APNP, directs care with a patient-centered approach to disease prevention and education. An individual who takes the medical school approach, such as a PA, follows a disease-centered approach to health care. Clinical approaches to healthcare vary based on scope of practice, education, and practice influence (Freeman, 2019). These differences in approaches are important in team management planning NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
In conclusion, healthcare is changing rapidly in how care is provided with an emphasis on a team approach to management. As a practitioner, it is important to know the differences between the roles of different advanced practice providers. Knowing an individual’s own scope of practice within their state and surrounding states is an important aspect of providing safe care. As a provider it is also important to ensure safe care is provided to all individuals. Knowing roles of other providers is important when delegation is required.
Freeman, J. (2019). Family Physicians, Nurse Practitioners, Physician Assistants, and Scope of Practice: Who Will Decide? Family Medicine, 51 (4): 305-307. doi: 10.22454/FamMed.2019.356702
Kraus, E. & DuBois, J. (2017). Knowing your limits: A qualitative study of physician and nurse practitioner perspectives on NP independence in primary care. Journal of General Internal Medicine, 32 (3): 284-290. doi: 10.1007/s11606-016-3896-7
Legislative Service Commission. (2020). Section 4723.43 | Scope of specialized nursing services. Retrieved from https://codes.ohio.gov/ohio-revised-code/section-4723.43 .
NCSL. (2021). Scope of Practice Policy. Retrieved from https://scopeofpracticepolicy.org/states/oh/
Poghosyan, L. Liu, J. & Norful, A. (2017). Nurse practitioners as primary care providers with their own patient panels and organizational structures: A cross-sectional study. International Journal of Nursing Studies, 74 : 1-7. doi: 10.1016/j.ijnurstu.2017.05.004 NRNP 6552: Advanced Nurse Practice in Reproductive Health Care
Respond to at least two of your colleagues’ posts on two different days andprovide additional insight to your colleagues related to issues and topics they may want to also consider. Use the Learning Resources and/or the best available evidence from current literature to support your explanation.
Note: For this Discussion, you are required to complete your initial post before you will be able to view and respond to your colleagues’ postings. Begin by clicking on the “Post to Discussion Question” link and then select “Create Thread” to complete your initial post. Remember, once you click on Submit, you cannot delete or edit your own posts, and you cannot post anonymously. Please check your post carefully before clicking on Submit!
I enjoyed reading your post as it highlights the fact that the fundamental differences that exist between a CRNP, CNM, and a PA assistance, lies in their scope of practice. A Family nurse practitioner or APRN has a wide variety of specialties which in some cases, is conducive to the patients. Most patients believe that as an APRN, you can prescribe any medication as long as a diagnosis is established. The APRN profession encompasses a wide variety of advanced nursing specialties; hence a wide variety of scope of practices issues is associated with this profession (Citizen Advocacy Center). This is because sometimes patients believe that as a nurse practitioner you can provide any services they need. At my clinical site today we had a patient who came in for a regular pap smear but while checking her vital signs and doing her labs, her blood pressure was so elevated and the urine dipstick indicated a glucose level of greater than 2000. The patient was referred to the ER and she started crying and requesting to know why they could not prescribe her blood pressure medications. The NP is WHNP and can not prescribe medications for blood pressure and diabetes but it was difficult for the patient to understand NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
The scope of practice for APRNs is also very dynamic as they can acquire new knowledge through education and take on new roles. “The scope of the advanced practices evolves through experience, acquisition of knowledge, evidence-based practices, technology development, and changes in the health care delivery system. Therefore, advanced practice registered nurses may need to practice in new settings, perform new procedures, and develop new skills during their professional careers” (Texas Board of Nursing).
Citizen Advocacy Center (CAC): Scope of Practice FAQs for Consumers. Advanced Practice Registered Nurse (APRNs). Retrieved from; www.ncsbn.org/APRNS_Scope_of_practice_FAQs_for_Consumers.pdf
Texas Board of Nursing: Practice-APRN scope of practice. Retrieved from; https://bon.texas.gov/practice_scope_of_practice_aprn.asp
Submission and Grading Information
Grading criteria.
To access your rubric: Week 1 Discussion Rubric
Post by Day 3 and Respond by Day 6
To Participate in this Discussion: Week 1 Discussion NRNP 6552: Advanced Nurse Practice in Reproductive Health Care Module 1 Assignment: Taking a Health History: Building a Health History: Asking Difficult Questions
Much of an archeologist’s work is done under the mantra “proceed with caution.” Archeologists must dutifully secure permissions to access sites. They also must exercise extreme caution when excavating or analyzing in a lab to avoid potential damage to historical artifacts.
Likewise, nurse practitioners must proceed with caution when building a patient’s health history. Important questions can be difficult for both nurse and patient. Care must be taken to approach such questions with dignity, tact, and respect to create an environment conducive to productive conversations.

For this Assignment, you will develop a script to be used to interview a volunteer serving in the role of patient.
- Review the Ewing (2004) questionnaire found in this week’s Learning Resources and consider the difficult questions you might have to ask when you take a patient’s health history.
- Review the screening tools found in the Learning Resources and consider how you might use an app or tool to assist in screening.
- Review the media programs related to a vaginal exam, pap test, and breast exam.
- Review the health history guide presented in Chapter 7 of the Schuiling & Likis (2022) text and consider how you would create your own script for building a health history. ( Note: You will also find the Health History Form in Chapter 7)
- Describe the components of a complete gynecologic health history. Include considerations for special populations such as LGBTQ+ individuals NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
- What health maintenance guidelines should be included for initial and follow up might be needed for follow-up assessments? (i.e., bone density test, Gardasil vaccine, shingles, etc.)?
- What is your patient’s living situation?
- Do they have stairs?
- Do they live by themselves?
- Do they have a working refrigerator?
- Create your own script for building a health history and use the Health History Template for guidance (consider the type of language you would use to help your patient be more comfortable). As you create your script, consider the difficult questions you want to include in your script.
Assignment: (1- to 2-page reflection)
- A brief summary of your experiences in developing and implementing your script during your health history.
- Explanations of what you might find difficult when asking these questions. What you found insightful and what would you say or do differently.
Reminder: The College of Nursing requires that all papers submitted include a title page, introduction, summary, and references. The Sample Paper provided at the Walden Writing Center provides an example of those required elements (available at http://writingcenter.waldenu.edu/57.htm). All papers submitted must use this formatting.
No Assignment submission due this week.
By Day 7 of Week 2
Submit your Module 1 Assignment by Day 7 of Week 2.
What’s Coming Up in Week 2?

Photo Credit: [BrianAJackson]/[iStock / Getty Images Plus]/Getty Images
Next week, you continue to explore common health screening but more specifically, how technology tools can support your screening process when working with women and/or LGBTQ+ individuals. You also examine the elements of gynecologic history and the recommended screenings NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
Week 2: Knowledge Check
In Week 2, you will experience your first Knowledge Check which covers the topics from Weeks 1 and 2 of Module 1. Please refer to the Week 2 Knowledge Check Assignment for further details related to the topics covered. Plan your time accordingly.

Practicum – Upcoming Deadline
In the Nurse Practitioner programs of study (FNP, AGACNP, AGPCNP, and PMHNP) you are required to take several practicum courses. If you plan on taking a practicum course within the next two terms, you will need to submit your application via Meditrek .
For information on the practicum application process and deadlines, please visit the Field Experience: College of Nursing: Application Process – Graduate web page.
Please take the time to review the Appropriate Preceptors and Field Sites for your courses.
Please take the time to review the practicum manuals, FAQs, Webinars and any required forms on the Field Experience: College of Nursing: Student Resources and Manuals web page.
- Field Experience: College of Nursing Quick Answers
- Field Experience: MSN Nurse Practitioner Practicum Manual
- Student Practicum Resources: NP Student Orientation
To go to the next week: Week 2 NRNP 6552: Advanced Nurse Practice in Reproductive Health Care Week 2: Common Health Screenings
Archeologists do not begin their work by simply selecting a site and digging for historical finds. Their initial steps involve laying the groundwork through research to apply expertise in their historical areas of focus, combined with best practices for excavation and analysis.
Similarly, nurse practitioners do not simply develop a treatment plan for patients. They methodically construct a patient’s history and apply best practices to conduct health screenings that help inform treatment. For practitioners of women’s healthcare this means applying expertise in specialized areas such as gynecology and gynecologic history taking and screening.
For this week, you examine the elements that comprise a patient’s gynecologic history. As part of your Module 1 assignment, you will describe elements of a complete gynecologic history.
- Analyze the elements of gynecologic history and recommended screenings for individuals (i.e., LGBTQ+)
- Analyze health maintenance guidelines when conducting patient assessments
- Identify key terms, concepts, and principles related to the primary care of individuals, families, and communities NRNP 6552: Advanced Nurse Practice in Reproductive Health Care
Likewise, nurse practitioners must proceed with caution when building a patient’s health history. Important questions can be difficult for both nurse and patient. Care must be taken to approach such questions with dignity, tact, and respect to create an environment conducive to productive conversations NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
- Review the Ewing (2004) questionnaire found in the Week 1 Learning Resources and consider the difficult questions you might have to ask when you take a patient’s complete health history.
- Review the health history guide presented in Chapter 7 of the Schuiling & Likis (2022) text and consider how you would create your own script for building a complete health history. ( Note: You will also find the Health History Form in Chapter 7)
- Include considerations for special populations such as LGBTQ+ individuals.
- What health maintenance guidelines should be included for initial and follow up might be needed for follow-up assessments? (i.e., bone density test, Gardasil vaccine, shingles, etc.)?
- Create your own script for building a health history and use the Health History Template for guidance (consider the type of language you would use to help your patient be more comfortable). As you create your script, consider the difficult questions you want to include in your script. There is no sample template to provide to you. You are the one to develop the script. Think of it as you are writing a movie and you need to write the script for the movie. What lines would you provide for the actor to utilize when sitting down with a patient to perform a COMPLETE Medical History which also entails those DIFFICULT GYN questions. You do not need to provide the answers to the questions however, if you find that beneficial, you may do so NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
To submit your completed Assignment for review and grading, do the following:
- Please save your Assignment using the naming convention “M1Assgn+last name+first initial.(extension)” as the name.
- Click the Module 1 Assignment Rubric to review the Grading Criteria for the Assignment.
- Click the Module 1 Assignment link. You will also be able to “View Rubric” for grading criteria from this area.
- Next, from the Attach File area, click on the Browse My Computer button. Find the document you saved as “M1Assignment+last name+first initial.(extension)” and click Open .
- If applicable: From the Plagiarism Tools area, click the checkbox for I agree to submit my paper(s) to the Global Reference Database .
- Click on the Submit button to complete your submission.
To access your rubric: Module 1 Assignment Rubric NRNP 6552: Advanced Nurse Practice in Reproductive Health Care
Check Your Assignment Draft for Authenticity
To check your Assignment draft for authenticity: Submit your Module 1 Assignment draft and review the originality report.
Submit Your Assignment by Day 7
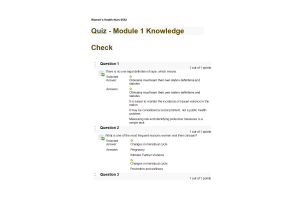
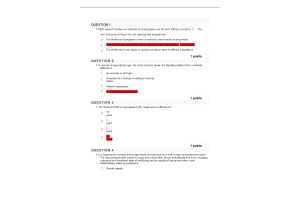
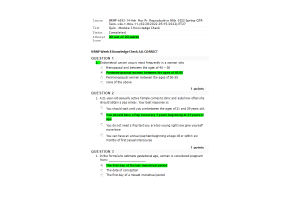
To participate in this Assignment: Module 1 Assignment Knowledge Check: Module 1
In this exercise, you will complete a 20-question Knowledge Check to gauge your understanding of this module’s content. You will have 1 attempt for each question. Each question is worth 1 point.
Possible topics to be covered from Weeks 1 and 2:
- Adult Gerontology
- Women’s Health and Health Promotion
- Gynecologic Health care for Sexual and Gender Minorities
- Using Evidence to Support Clinical Practice
- Role of women’s health NP
- Gynecologic Anatomy and Physiology
- Gynecologic History and Physical Exam
- Gynecologic Screening and Health Maintenance
- Sexual Violence
- Women’s Health Care Across the Life Span
- Well-Woman Exam
- Osteoporosis
- Tobacco Cessation NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
Photo Credit: kyoshino / iStock / Getty Images Plus / Getty Images
Complete and submit your Knowledge Check.
Submission Information
Submit your knowledge check by day 7.
To submit your Knowledge Check: Module 1 Knowledge Check What’s Coming Up in Module 2?
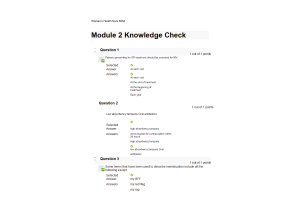
In Module 2, you explore important aspects of gynecologic health. You will examine common gynecologic conditions through a variety of case studies. You also will complete a Knowledge Check covering the topics from Weeks 3 through 5, and you will complete a Midterm Exam to assess your understanding of the content examined in Weeks 1 – 6 of the course.
Week 5: Knowledge Check
In Week 5, you will complete your next Knowledge Check which covers the topics from Weeks 3, 4 and 5 of Module 2. Please refer to the Week 5 Knowledge Check Assignment for further details related to the topics covered. Plan your time accordingly NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
ORDER A PLAGIARISM FREE PAPER NOW
To go to the next module: Module 2 Week 3: Gynecologic Health
Western movies often portray dusty old towns with limited available resources that include a single general store, a single saloon, and a single sheriff. Within these settings, healthcare is revealed to be the responsibility of the single town doctor.
Unlike these theatrical towns of old, most modern developed communities enjoy the luxury of diverse choices in shopping, entertainment, and more. Thankfully, this includes healthcare options that extend the concept of the “old west” town doctor to diverse specialty areas of practice, including those focused on women’s health care and wellness, such as gynecology.
For this week, you will use a case study to analyze information obtained from well-woman examinations. You also will consider and propose treatment plans for diagnoses.
- Analyze pertinent patient information obtained from a comprehensive well-woman exam
- Formulate differential diagnoses
- Recommend diagnostics to support differential diagnoses
- Develop treatment and management plans
- Develop additional questions to support patient assessments NRNP 6552: Advanced Nurse Practice in Reproductive Health Care
Case studies provide the opportunity to simulate realistic scenarios involving patients presenting with various health problems or symptoms. Such case studies enable nurse learners to apply concepts, lessons, and critical thinking to interviewing, screening, diagnostic approaches, as well as the development of treatment plans.
Photo Credit: Teodor Lazarev / Adobe Stock
For this Case Study Discussion, you will review a case study scenario to obtain information related to a comprehensive well-woman exam and determine differential diagnoses, diagnostics, and develop treatment and management plans.
- By Day 1 of this week, you will be assigned to a specific case study scenario for this Discussion. Please see the “Course Announcements” section of the classroom for your case study assignment from your Instructor.
- Review the Learning Resources for this week and pay close attention to the media program related to the basic microscope skills. Also, consider re-reviewing the media programs found in Week 1 Learning Resources.
- Carefully review the clinical guideline resources specific to your assigned case study.
- Use the Focused SOAP Note Template found in the Learning Resources to support Discussion. Complete a SOAP note and critically analyze this and focus your attention on the diagnostic tests. You are NOT to post your SOAP note. This is for your information only to help you develop your differential diagnosis and additional questions NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
DO NOT POST A SOAP NOTE. Post your differential diagnosis. Include the additional questions you would ask the patient. Be sure to include an explanation of the tests you might recommend, ruling out any other issues or concerns and include your rationale. Be specific and provide examples. Use your Learning Resources and/or evidence from the literature to support your explanations.
Respond to at least two of your colleagues’ posts on two different days and explain how you might think differently about the types of tests you might recommend and explain why. Use your Learning Resources and/or evidence from the literature to support your position.
To access your rubric: Week 3 Case Study Discussion Rubric
To Participate in this Discussion: Week 3 Case Study Discussion NRNP 6552: Advanced Nurse Practice in Reproductive Health Care. What’s Coming Up in Week 4?
Next week, you will explore common gynecologic conditions as they relate to sexually transmitted infections (STIs), and contraceptive issues, as well as other conditions through a specific case study.
To go to the next week: Week 4
Week 4: Common Gynecologic Conditions, Part 1
Patients can present a variety of symptoms including breast or vaginal discomfort that may indicate gynecologic conditions. These conditions may range from minor and easy- to-treat infections to more serious issues related to cancer or sexually transmitted diseases.
Nurse practitioners must apply expertise and best practices to early interventions to contribute to diagnoses of issues and plans for treatments. These activities typically begin with analysis of findings from interviews and screenings.
For this week, you will practice these approaches by considering circumstances of case study. You will analyze a patient history and symptoms presented and recommend tests and treatment options.
- Identify key symptoms consistent with a medical diagnosis
- Analyze the health history and presentation of a patient
- Analyze patient diagnoses
- Apply case-specific clinical guidelines
- Recommend diagnostic tests and treatment options NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
Case studies provide the opportunity to simulate realistic scenarios involving patients presenting with various health problems or symptoms. Such case studies enable nurse learners to apply concepts, lessons, and critical thinking to interviewing, screening, and diagnostic approaches, as well as to the development of treatment plans.

For this Case Study Discussion, you will once again review a case study scenario to obtain information related to a comprehensive well-woman exam and determine differential diagnoses, diagnostics, and develop treatment and management plans NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
- By Day 1 of this week, you will be assigned to a specific case study scenario for this Discussion. Please see the “Course Announcements” section of the classroom for your assignment from your Instructor.
- Review the Learning Resources for this week and specifically review the clinical guideline resources specific to your assigned case study.
- Use the Focused SOAP Note Template found in the Learning Resources to support your Discussion. Complete a SOAP note and critically analyze this and focus your attention on the diagnostic tests. You are NOT to post your SOAP note. This is for your information only to help you develop your differential diagnosis and additional questions.
DO NOT POST A SOAP NOTE. Post your primary diagnosis. Include the additional questions you would ask the patient and explain your reasons for asking the additional questions. Then, explain the types of symptoms you would ask. Be specific and provide examples. ( Note: When asking questions, consider sociocultural factors that might influence your question decisions.)
Based on the preemptive diagnosis, explain which treatment options and diagnostic tests you might recommend. Use your Learning Resources and/or evidence from the literature to support your recommendations.
Respond to at least two of your colleagues’ posts on two different days and explain how you might think differently about the types of diagnostic tests you would recommend and explain your reasoning. Use your Learning Resources and/or evidence from the literature to support your position NRNP 6552: Advanced Nurse Practice in Reproductive Health Care.
To access your rubric: Week 4 Case Study Discussion Rubric
To Participate in this Discussion: Week 4 Case Study Discussion What’s Coming Up in Week 5?
Next week, you will continue to explore common gynecologic conditions as they relate to reproductive health issues as well as other conditions.
Specifically, for next week’s Discussion, you will propose a case study scenario for instructor approval. Please review the Week 5 Discussion instructions and be ready to submit your proposed case study scenario by Day 1 of Week 5. Plan your time accordingly.
In Week 5, you will complete your next Knowledge Check which covers the topics from Weeks 3, 4 and 5 of Module 2. Please refer to the Week 5 Knowledge Check Assignment for further details related to the topics covered. Plan your time accordingly. NRNP 6552: Advanced Nurse Practice in Reproductive Health Care
Why We Are the Best
- 100% non-plagiarized Papers
- Dedicated nursing and healthcare writers
- 24/7 /365 Service Available
- Affordable Prices
- Money-back and Privacy guarantees
- Unlimited Amendments upon request
- Satisfaction guarantee

- Online Nursing Assignment Help
- Nursing Assignment Help
- Nursing Dissertation Writing Services
- Nursing Capstone Project Writing Services
- Best Nursing Essay Writing Company
- Best Online Nursing Assignment Help
- Nursing Term Paper Writing Services
- Nursing Report Writing Services
- Nursing Annotated Bibliography by Professional
- Nursing Essay Assignments
- Nursing Assignment Writing
- Nursing Case Study Writing Services
- Nursing Coursework Writing
- Online Nursing Research Paper writing service
- PICO Question Examples
- Nursing Thesis Writing Services
- Nursing Research Paper Writing Services
- Nursing Presentation Writing
- Terms and Conditions
- Epidemiology assignment help
- Write my nursing dissertation for Me
- Nursing Essay Writing Service

Provide details on what you need help with along with a budget and time limit. Questions are posted anonymously and can be made 100% private.

Studypool matches you to the best tutor to help you with your question. Our tutors are highly qualified and vetted.

Your matched tutor provides personalized help according to your question details. Payment is made only after you have completed your 1-on-1 session and are satisfied with your session.
Walden University Gynecologic Health Case Study
User Generated
fgryynqnivq
Health Medical
Walden University
Description
Case Study 2
Elaine Goodwin is a 38-year-old G5 P5 LC 6 presenting to your clinic today to discuss contraceptive options. She states that she is not interested in having more children but her new partner has never fathered a child. Her medical history is remarkable for exercise-induced asthma, migraines, and IBS. Her surgical history is remarkable only for tonsils as a child. Her social history is negative for alcohol, tobacco, and recreational drugs. She has no known drug allergies and takes only vitamin C. Hospitalizations were only for childbirth. Family history reveals that her maternal grandmother is alive with dementia, while her maternal grandfather is alive with COPD. Her paternal grandparents are both deceased due to an automobile accident. Her mother is alive with osteopenia and fibromyalgia, and her dad is alive with a history of skin cancer (basal cell). Elaine has one older sister with no medical problems and one younger brother with no reported medical problems.
- Height 5’ 7” Weight 148 (BMI 23.1), BP 118/72 P 68
- HEENT: wnl
- Neck: supple without adenopathy
- Lungs/CV: wnl
- Breast: soft, fibrocystic changes bilaterally, without masses, dimpling or discharge
- Abd: soft, +BS, no tenderness
- VVBSU: wnl, except 1 st degree cystocele
- Cervix: firm, smooth, parous, without CMT
- Uterus: RV, mobile, non-tender, approximately 10 cm,
- Adnexa: without masses or tenderness
Case Study Discussion: Gynecologic Health
Case studies provide the opportunity to simulate realistic scenarios involving patients presenting with various health problems or symptoms. Such case studies enable nurse learners to apply concepts, lessons, and critical thinking to interviewing, screening, diagnostic approaches, as well as the development of treatment plans.
Photo Credit: Teodor Lazarev / Adobe Stock
For this Case Study Discussion, you will review a case study scenario to obtain information related to a comprehensive well-woman exam and determine differential diagnoses, diagnostics, and develop treatment and management plans.
To prepare:
- By Day 1 of this week, you will be assigned to a specific case study scenario for this Discussion. Please see the “Course Announcements” section of the classroom for your case study assignment from your Instructor.
- Review the Learning Resources for this week and pay close attention to the media program related to the basic microscope skills. Also, consider re-reviewing the media programs found in Week 1 Learning Resources.
- Carefully review the clinical guideline resources specific to your assigned case study.
- Use the Focused SOAP Note Template found in the Learning Resources to support Discussion. Complete a FOCUSED SOAP note and critically analyze this and focus your attention on the diagnostic tests. Please post your SOAP note. This will help you develop your differential diagnosis and additional questions
Please POST your FOCUSED SOAP NOTE with your differential diagnosis. Include the additional questions you would ask the patient. Be sure to include an explanation of the tests you might recommend, ruling out any other issues or concerns and include your rationale. Be specific and provide examples. Use your Learning Resources and/or evidence from the literature to support your explanations.
Read a selection of your colleagues’ responses.
Respond to at least two of your colleagues’ posts on two different days and explain how you might think differently about the types of tests you might recommend and explain why. Use your Learning Resources and/or evidence from the literature to support your position.
Note: For this Discussion, you are required to complete your initial post before you will be able to view and respond to your colleagues’ postings. Begin by clicking on the "Post to Discussion Question" link and then select "Create Thread" to complete your initial post. Remember, once you click on Submit, you cannot delete or edit your own posts, and you cannot post anonymously. Please check your post carefully before clicking on Submit! Learning Resources Required Readings (click to expand/reduce) Schuiling, K. D., & Likis, F. E. (2022). G ynecologic health c are (4th ed.). Jones and Bartlett Learning. Chapter 10, “Women’s Health After Bariatric Surgery” (pp. 165 – 171)
Agency for Healthcare Research and Quality (AHRQ). Intimate partner violence screening: Fact sheet and resources . https://www.ahrq.gov/ncepcr/tools/healthier-pregna...
Fanslow, J., Wise, M. R., & Marriott, J. (2019). Intimate partner violence and women’s reproductive health. Obstetrics, Gynaecology & Reproductive Medicine, 29 (12), 342–350. https://go.openathens.net/redirector/waldenu.edu?u...
Lockwood, C. J. (2019). Key points for today’s ‘well-woman’ exam: A guide for ob/gyns. Contemporary OB/GYN, 64 (1), 23–29. https://search.ebscohost.com/login.aspx?direct=tru...
American College of Obstetricians and Gynecologists (ACOG). (2020). https://www.acog.org/
American Cancer Society, Inc. (ACS). (2020). Information and Resources about for Cancer: Breast, Colon, Lung, Prostate, Skin. https://www.cancer.org/
American Nurses Association (ANA). (n.d.). https://www.nursingworld.org/
Centers for Disease Control and Prevention. (CDC). (n.d.). https://www.cdc.gov/
HealthyPeople 2030. (2020). Healthy People 2030 Framework . https://www.healthypeople.gov/2020/About-Healthy-P...
The American Association of Nurse Practitioners (AANP). What’s happening at your association. (2020). https://www.aanp.org/
Document : Focused SOAP Note Template (Word document)
Unformatted Attachment Preview

Explanation & Answer

Please view explanation and answer below. 1 Focused SOAP Note Name Institution Affiliation Date 2 Focused SOAP Note Patient Information: EG, 38yo, Female, White S. CC (Chief Complaint): Contraceptive options. HPI: The patient is a 38-year-old white female who has yet to decide on the best contraceptive options that she should take. She states that she doesn't want more children and has a new partner who has yet to father a child. Current Medications: Vitamin C. Allergies: She doesn’t have any drug allergies. PMHx: She has a medical history of irritable bowel syndrome (IBS), migraines, and exerciseinduced asthma. She was hospitalized when she was a child. Soc. & Substance Hx: She doesn’t use alcohol, tobacco, or other recreational drugs. Fam Hx: Her younger brother and older sister are alive with no reported medical problems. Both her parents are also alive. Her mother has fibromyalgia and osteopenia. On the other hand, her dad has a family history of basal cell cancer. Her maternal grandmother and grandfather live with dementia and chronic obstructive pulmonary disease (COPD), respectively. Her paternal grandparents died after a car accident. Surgical Hx: She had a tonsillectomy (surgery for tonsils) when she was a child. 3 Mental Hx: No known mental health issues. Violence Hx: No concerns or issues about safety. Reproductive Hx: Her gravidity is equal to five, and her parity is equal to five (G5 P5). She isn’t interested in having more children. She has vaginal intercourse and prefers males. Her new partner hasn’t fathered a child. ROS: GENERAL: Within normal limits (WNL). Her body is strong. She has a normal appetite, no chills, weight loss, and fatigue. HEENT: Head: WNL; Eyes: WNL, She doesn’t have any sight impairments, such as blurred vision, visual loss, and double vision; Ears: WNL, She hasn’t experienced any hearing impairments; Nose: WNL, Currently, she doesn’t have a runny nose, and she hasn’t coughed or sneezed recently; Throat: WNL, No sore throat. SKIN: WNL, She doesn’t itch or have any rashes. CARDIOVASCULAR: WNL, Her chest is healthy, with no discomfort, pressure, or pain. She has a normal heartbeat rate (P = 68), and her body doesn’t have any swellings. RESPIRATORY: WNL, She isn’t short of breath, mucus, and cough. GASTROINTESTINAL: WNL, She doesn’t have any abdominal pain or blood. In addition, she has no nausea, diarrhea, vomiting, and...

24/7 Study Help
Stuck on a study question? Our verified tutors can answer all questions, from basic math to advanced rocket science !

Similar Content
Related tags.
teaching plan personal training health and medical prevention articles nursing theories project health Thyroid disorders poison, GLOMERULONEPHRITIS united states
The Age Of Light
by Whitney Scharer
Of Mice and Men
by John Steinbeck
The Woman in the Window
by A. J. Finn
Fahrenheit 451
by Ray Bradbury
Shutter Island
by Dennis Lehane
by Ayn Rand
The Rhythm Section
by Mark Burnell
by George Orwell
What Happened
by Hillary Clinton
working on a study question?

Studypool is powered by Microtutoring TM
Copyright © 2024. Studypool Inc.
Studypool is not sponsored or endorsed by any college or university.
Ongoing Conversations
Access over 35 million study documents through the notebank
Get on-demand Q&A study help from verified tutors
Read 1000s of rich book guides covering popular titles

Sign up with Google
Sign up with Facebook
Already have an account? Login
Login with Google
Login with Facebook
Don't have an account? Sign Up

IMAGES
VIDEO