An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


A Case of Classical Hodgkin’s Lymphoma Presenting With Intractable Pruritus
Gregory benn, sneha adidam, lekidelu taddesse-heath.
- Author information
- Article notes
- Copyright and License information
Sneha Adidam [email protected]
Corresponding author.
Accepted 2021 Nov 24; Collection date 2021 Nov.
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Hodgkin’s Lymphoma presenting with hypereosinophilia and intractable pruritus is a rare entity. Diagnostic and therapeutic decisions remain a challenge in such patients. Here we report a case of a 25-year-old female with a special case of Hodgkin’s lymphoma. A 25-year-old was admitted to our hospital for intractable pruritus and was found to have significant leukocytosis with eosinophilic predominance. The patient underwent a bone marrow biopsy and mediastinal lymph node biopsy, which confirmed classical Hodgkin’s lymphoma. Furthermore, the patient was given six cycles of adriamycin, bleomycin, vincristine, and doxorubicin (ABVD) chemotherapy and initially showed improvement; however, she relapsed within a short period. Post-treatment positron emission tomography (PET) scan showed interval progression of the disease, and so the patient was referred for a clinical trial with immunotherapy and Brentuximab vedotin.
Keywords: hypercellular bone marrow, metastatic lymphadenopathy, brentuximab vedotin, pruritus, hyper-eosinophilia, hodgkin lymphona
Introduction
Pruritus may arise as a primary dermatologic condition or a manifestation of a broad array of systemic diseases [ 1 ]. Intractable pruritus with unusual hypereosinophilia requires a comprehensive evaluation for an accurate diagnosis. Hodgkin’s lymphoma (HL) is a neoplasm of lymphoid tissue associated with eosinophilia in 15% of cases [ 2 ]. The exact mechanism remains unknown; however, there is some knowledge of various mediators such as interleukin 5 (IL-5) and granulocyte-macrophage colony-stimulating factor (GM-CSF) that may be implicated [ 3 , 4 ]. There is an unmet need to study the prognostic factors in such cases as it is understudied. This is a case of an unusual presentation of Hodgkin’s Lymphoma (HL) in a 25-year-old Hispanic female who presented with a three-month history of intractable pruritus and marked eosinophilia. The report aims to sensitize readers of a rare presentation of HL and to discuss the treatment response in this patient.
Case presentation
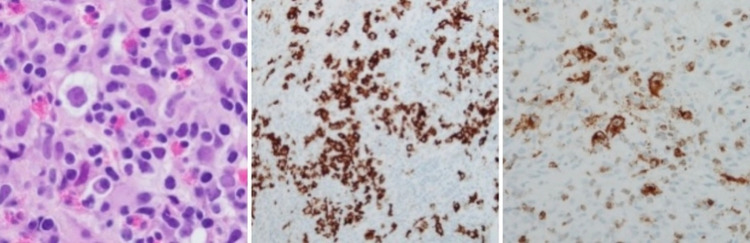
This is a case of a 25-year-old Hispanic female who presented with generalized, intractable pruritus for three months. She endorsed areas of purplish discoloration where she had itching and that the itching subsided temporarily in the shower and with topical emollients but worsened with towel drying. Notably, the patient denied any triggers, such as a change in detergents or perfumes. During the outpatient evaluation, she was prescribed hydroxyzine and loratadine. She denied any family history of hematological conditions, including lymphoma/leukemia or urticaria. On arrival, vitals include blood pressure 113/66mmHg, heart rate 126, temperature 98.9 F, respiratory rate 18, and saturation of 100% on room air. Physical examination revealed diffuse petechiae on skin examination, and respiratory examination revealed crackles in the left lower lobe. The rest of the examination was otherwise within normal limits. Laboratory investigations showed that she had a significant leukocytosis of 68.5 x 10^3 with a predominant eosinophilic count of 17.9 x 10^3. The basic metabolic panel was within normal limits. The stool work-up was positive for Dientamoeba Fragilis and was treated with a course of paromomycin. Leukocyte count remained persistently elevated, with an eosinophilic count peaking at 41.93 x10^3. Initial imaging obtained was chest X-ray (Figure 1 ) which revealed large mediastinal adenopathy. This was followed up with chest computed tomography (CT) (Figure 2 ), which showed extensive prominent bulky heterogenous lymph nodes in the mediastinum. There was vascular compromise due to extensive involvement of pre-tracheal and perivascular spaces. Further investigations were performed. Bone marrow biopsy (Figure 3 ) showed mildly hypercellular bone marrow (80%-85%) with marked eosinophilia, decreased iron storage, and negative platelet-derived growth factor receptor (PDGFR). Mediastinal mass biopsy (Figure 4 ) showed classical HL, CD30+, and CD15+. (Due to a limited sample, it was difficult to subclassify). flow cytometry, fluorescence in situ hybridization (FISH), and cytogenetic of peripheral blood showed no platelet-derived growth factor receptor α (PDGFRA) mutation, no monoclonality, and a normal tryptase level. The PET scan for interim staging showed extensive mediastinal lymphadenopathy, hypermetabolic activity within the lymph nodes standardized uptake value (LN SUV) 4.3-5.8, mass size 5.7cmx4.8cm, another activity noted with enlarged 2.3 cm lymph nodes (LN) adjacent to the cardiac apex, with a comparison with the initial CT it showed a significant reduction in the size of the mass.
Figure 1. Initial Chest X-ray Revealed Large Mediastinal Adenopathy .
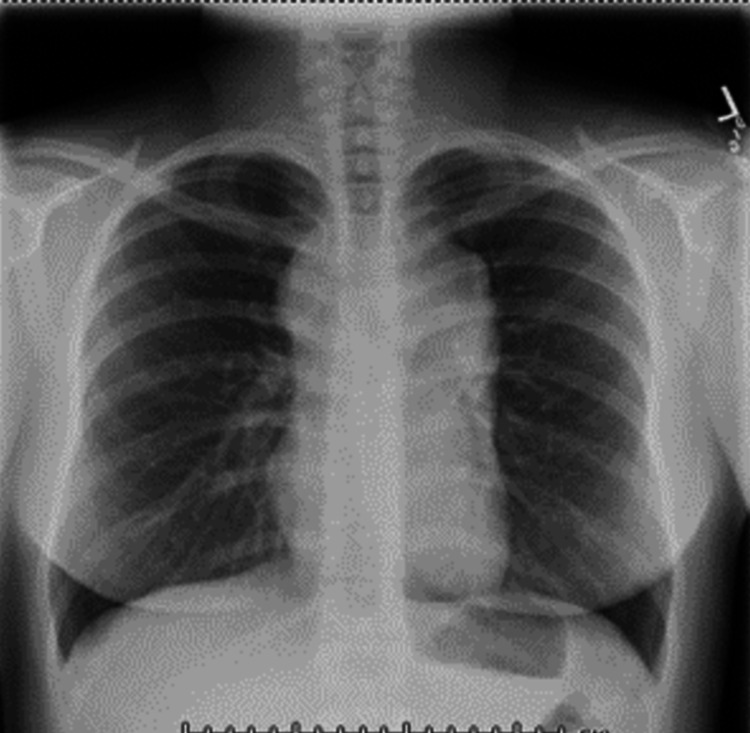
Figure 2. Chest Computed Tomography showing extensive prominent bulky heterogenous lymph nodes in the anterior and middle mediastinum (measures 8 cm in AP dimension and 7 cm transversely), including involvement of the pre-tracheal and perivascular spaces. As a result of the extensive involvement, there is significant narrowing of the left brachiocephalic vein as it traverses the mediastinum. There is also narrowing of the superior vena cava. No clear evidence of hilar adenopathy.
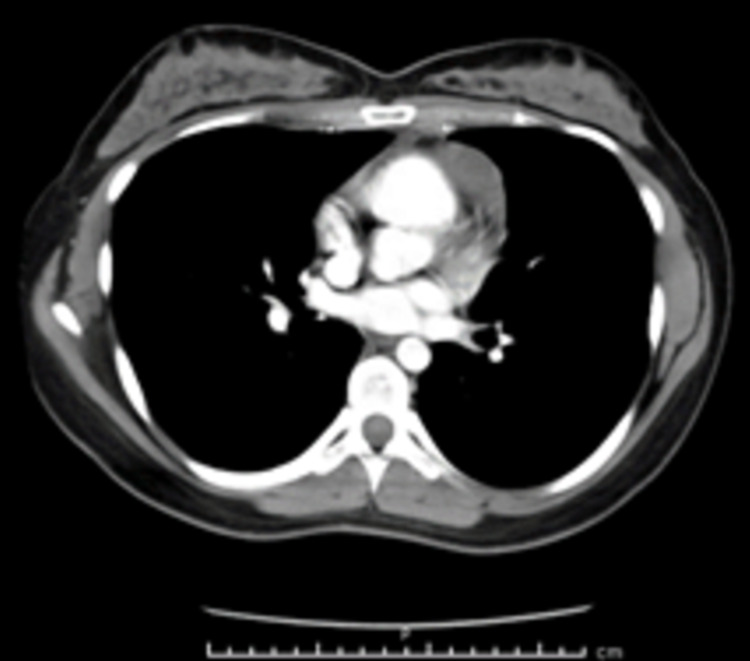
Figure 3. Peripheral smear and bone marrow biopsy. There was a marked increase in eosinophils peripheral smear (left), bone marrow aspirate (middle) and core biopsy (right) .
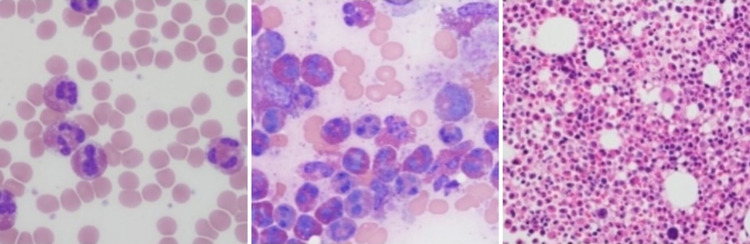
Figure 4. Mediastinal lymph node biopsy. The core biopsy showed marked tissue eosinophilia with scattered large, atypical cells. The large cells had large nuclei and prominent nucleoli. The neoplastic cells were positive for CD 30 and CD 15.
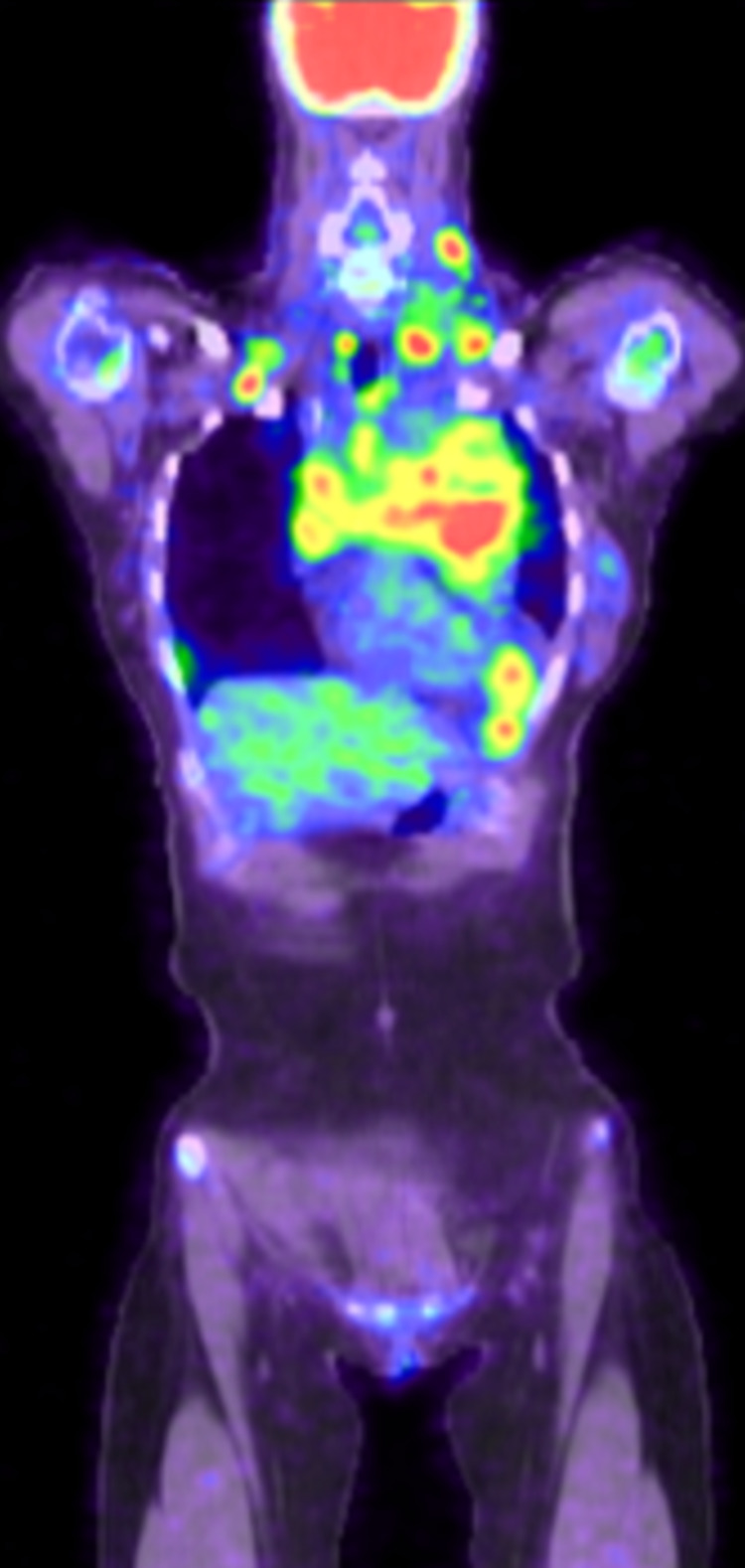
She currently follows up in the Hematology clinic and is being managed for classical HL with eosinophilic predominance. She was assigned stage IIA Bulky disease. She received an ABVD regime (adriamycin, bleomycin, vincristine, and doxorubicin) which she tolerated well. Symptomatic treatment (singular, prednisone) for her pruritus was initiated. Gradually, her symptoms progressively improved since the initiation of chemotherapy. Furthermore, her hospital course was complicated by one re-admission for fatigue, tachycardia, and dyspnea, which was later diagnosed as an acute pulmonary embolism on CT pulmonary angiogram and was treated with therapeutic enoxaparin. She was stabilized and discharged with continued follow-up in the hematology clinic. After completion of her six cycles of treatment, she was noted to have normal WBC with normal eosinophil level. However, three weeks after treatment completion, it was noted that her eosinophils level rose again, and her post treatment PET scan (Figures 5 , 6 ) showed interval progression of her disease for which she was referred for a clinical trial that involved the usage of immunotherapy plus brentuximab vedotin.
Figure 5. Post treatment PET with disease progression. Neck: shows numerous hypermetabolic lymph nodes. Largest node measures 2.4cm in diameter. Chest: extensive bulky mediastinal adenopathy/soft tissue.
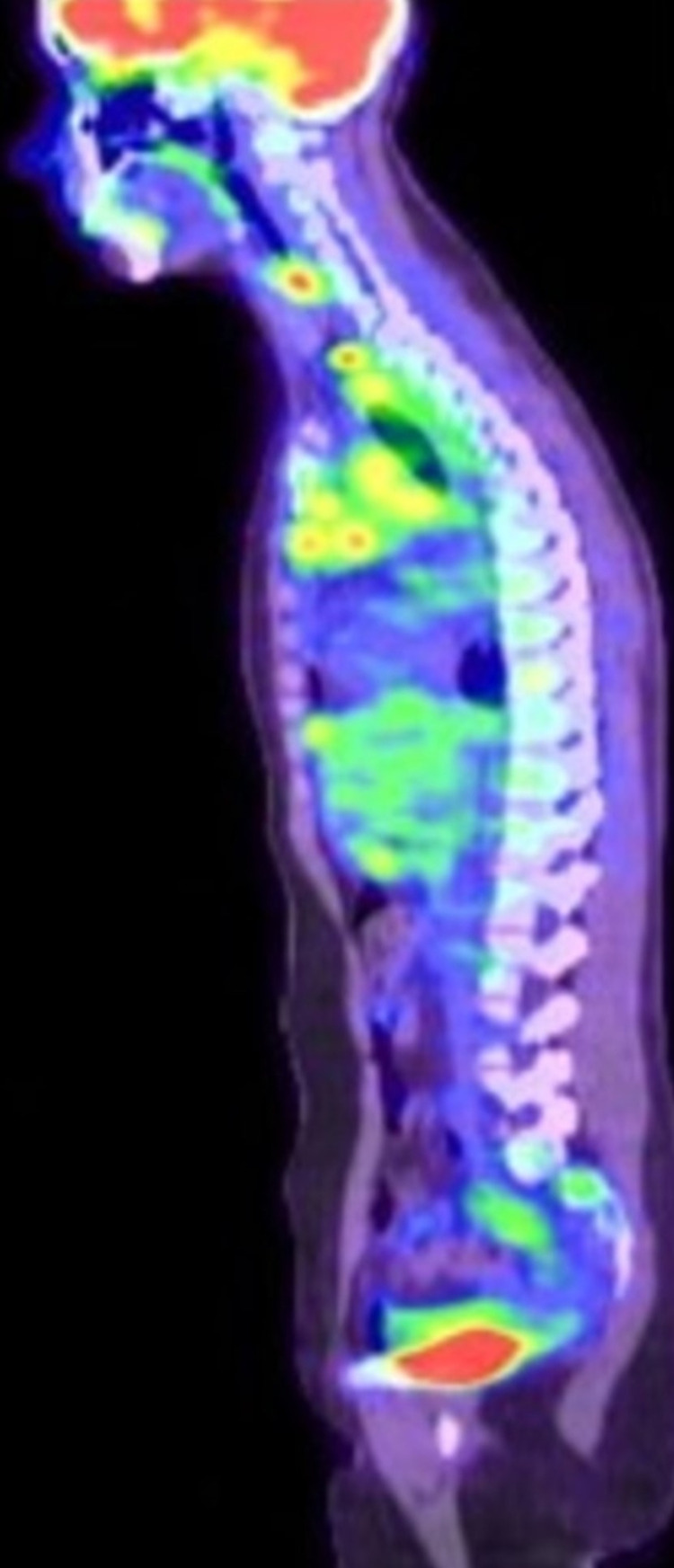
Figure 6. Post treatment PET with disease progression. Neck: shows numerous hypermetabolic lymph nodes. Largest node measures 2.4cm in diameter. Chest: extensive bulky mediastinal adenopathy/soft tissue.
Upon literature review, the supporting evidence for HL in our index case are as follows: intractable pruritis being the initial symptom, labs that revealed marked leukocytosis with eosinophilia, and a CT chest that showed extensive bulky lymph nodes in the anterior and middle mediastinum with pre-tracheal/vascular involvement. As a result, there was a significant narrowing of the left brachiocephalic vein and superior vena cava.
HL has an incidence of approximately 15% [ 3 ] and is characterized by the presence of Reed-Sternberg (RS) cells which are also CD 30 positive in all cases. They are CD15 positive on immunohistochemical staining in 80%-85% of cases. Definitive diagnosis is made by the presence of RS cells and immunophenotyping. Furthermore, primary mediastinal large B-cell lymphoma, anaplastic large cell lymphoma (ALCL), and gray zone lymphoma are some differentials for CD-30 lymphomas. AVD-A (which is brentuximab vedotin, doxorubicin, vinblastine, and dacarbazine) combination has been compared with ABVD combination in a prospective randomized phase III trial [ 5 ].
Eosinophilia is an uncommon finding in HL. Thus, there are very few cases reported in the literature [ 6 ]. Eosinophilia may be either mild, moderate, or severe based on the number of eosinophils. Hypereosinophilia is defined by two readings of eosinophil level of >1.5 x10^9 with an interval of >1 month between each reading. Furthermore, another entity called hypereosinophilia syndrome is defined by hypereosinophilia and organ damage [ 7 ].
Eosinophilia with lymphadenopathy raises the differentials of parasitic infection, especially in certain populations, including immigrants. Furthermore, Gotlib et al. described the identification of the FIP1L1-PDGFRA fusion gene. This may assist in distinguishing chronic eosinophilic leukemia from idiopathic hypereosinophilia. Our index case was negative for PDGFRA [ 8 , 9 ].
The index case was labelled as early-stage IIA bulky disease, which is an unfavorable factor and responded well initially to the ABVD regimen with initial abatement of her symptoms only to recur after six cycles. The standard ABVD regimen usually is associated with a good therapeutic response. However, unfavorable factors and associated hypereosinophilia may have played a role in early relapse. Eosinophils may act as important elements in the pathology of HL by providing cellular ligands for TNF-superfamily receptors (CD40, CD30, CD95/Fas). They can transduce proliferation and antiapoptotic signals at the surface of Hodgkin and Reed/Sternberg (H-RS) cells. Eosinophils may contribute to the disregulated network of interactive signals between H-RS cells, T cells, and other surrounding reactive cells [ 10 ].
Due to relapse of symptoms of the disease, our index patient was referred to a clinical trial with brentuximab vedotin and immunotherapy. In a phase II study, brentuximab vedotin was trialed in 102 patients with CD 30 positive HL who relapsed/refractory to autologous stem cell transplant. The overall response rate was found to be 75%, with complete remissions in 34% of patients [ 11 ].
Conclusions
This paper reports the case of a female Hispanic patient in her third decade of life with an atypical presentation of having severe intractable pruritus, skin lesions, hypereosinophilia, and mediastinal adenopathy. The patient quickly relapsed after an initial good response to the standard ABVD regimen for stage II bulky disease. She required treatment with a trial combination of brentuximab vedotin and immunotherapy. Hypereosinophilia, along with bulky disease, may have contributed to her early relapse. This case also serves to provide a rare scenario of eosinophilia and intractable pruritus in HL, which sensitizes physicians to think of HL in similar case presentations in the future.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained or waived by all participants in this study
- 1. Diagnosis and treatment of pruritus. Nowak D, Yeung J. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5729138/ Can Fam Phys. 2017;63:918–924. [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 2. Eosinophilia as a first sign of Hodgkin's lymphoma - a case report. Milošević R, Leković D, Antonijević N, Bogdanović A. http://www.doiserbia.nb.rs/img/doi/0042-8450/2017/0042-84501600245M.pdf Vojno Pregl. 2017;74:581–585. [ Google Scholar ]
- 3. Hypereosinophilia in hodgkin lymphoma. Cyriac S, Sagar TG, Rajendranath R, Rathnam K. Indian J Hema Blo Transf. 2008;24:67–68. doi: 10.1007/s12288-008-0031-x. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Selective peripheral blood eosinophilia associated with survival advantage in Hodgkin's disease (BNLI Report No 31). British National Lymphoma Investigation. Hudson VB, Linch DC, Macintyre AE, Bennett HM, MacLennan AK, Hudson VG, Jelliffe MA. J Clin Pathol. 1987;40:247–250. doi: 10.1136/jcp.40.3.247. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 5. Hodgkin's lymphoma: the pathologist's viewpoint. Pileri SA, Ascani S, Leoncini L, et al. J Clin Pathol. 2002;55:162–176. doi: 10.1136/jcp.55.3.162. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 6. Hodgkin’s lymphoma concomitant with hypereosinophilia as atypical presentation. Moreno-Urbina SI, Ramos-Estrada JG, Valdez-Payán NH. https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=77571 Rev Hematol Mex. 2018;19:50–53. [ Google Scholar ]
- 7. Approach to eosinophilia. Liapis K. https://haema-journal.gr/?p=1507 HAEMA. 2019;10:116–127. [ Google Scholar ]
- 8. Eosinophilic leukemia and idiopathic hypereosinophilic syndrome are mutually exclusive diagnoses. Bain JB. https://ashpublications.org/blood/article/104/12/3836/89070/Eosinophilic-leukemia-and-idiopathic . Blood. 2004;104:3836–3837. doi: 10.1182/blood-2004-07-2680. [ DOI ] [ PubMed ] [ Google Scholar ]
- 9. The FIP1L1-PDGFRalpha fusion tyrosine kinase in hypereosinophilic syndrome and chronic eosinophilic leukemia: implications for diagnosis, classification, and management. Gotlib J, Cools J, Malone JM 3rd, Schrier SL, Gilliland DG, Coutré SE. Blood. 2004;103:2879–2891. doi: 10.1182/blood-2003-06-1824. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. The role of eosinophils in the pathobiology of Hodgkin's disease. Pinto A, Aldinucci D, Gloghini A, et al. https://pubmed.ncbi.nlm.nih.gov/9209649/ Ann Oncol. 1997;8:89–96. [ PubMed ] [ Google Scholar ]
- 11. Results of a pivotal phase II study of brentuximab vedotin for patients with relapsed or refractory Hodgkin's lymphoma. Younes A, Gopal AK, Smith SE, et al. J Clin Oncol. 2012;30:2183–2189. doi: 10.1200/JCO.2011.38.0410. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (1.0 MB)
- Collections

Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Follow us on :

Take a look at the Recent articles
A classical presentation of hodgkin's disease in a 27-year-old healthy female, massimo bolognesi.
General Practitioner, AUSL della Romagna District of Cesena, Via Ungaretti 494 47521 Cesena, Italy
E-mail : [email protected]
Diletta Bolognesi
Junior Fellow Doctor General Practice, Territorial Medicine AUSL della Romagna District of Cesena C.so Cavour 180, Italy
Giampiero Pasini
DOI: 10.15761/GIMCI.1000102
Herein, we report a case of classical Hodgkin’s lymphoma (HL) in an otherwise healthy 27- year-old female who came to the office of her general practitioner with flu-like illness and left supraclavicular swelling of uncertain nature, without other symptoms. An ultrasound of the neck detected many enlarged lymph nodes in the left supraclavicular region, and a chest X-ray showed left mediastinal enlargement. Subsequent Computed Tomography scan of the chest and abdomen confirmed the presence of many enlarged lymph nodes in the neck, mediastinum and liver, and a FDG-PET/CT scan showed multiple scattered consolidation lesions involving also the bones. The diagnosis of classical Hodgkin’s lymphoma, nodular sclerosis subtype, was made on a subsequent cervical lymph node biopsy.
Hodgkin's lymphoma, nodular sclerosis CHL (NSCHL), asymptomatic lymphadenopathy
Introduction
The modern classification of Hodgkin’s disease was introduced by Lukes and Butler [1].
The Revised European American Lymphoma (REAL) classification in 1994 included Hodgkin’s lymphoma as one of the lymphoid neoplasms, and distinguished between 2 major types: nodular lymphocyte predominant Hodgkin’s lymphoma (NLPHL) and classical Hodgkin’s lymphoma (CHL). CHL was further classified into 4 subtypes: nodular sclerosis CHL (NSCHL), mixed cellularity CHL (MCCHL), lymphocyte-rich CHL (LRCHL), and lymphocyte-depleted CHL (LDCHL) [2].
The terminology recommended in the REAL classification was incorporated into the World Health Organization (WHO) classification of tumors of hematopoietic and lymphoid tissues, including the substitution of the term Hodgkin’s lymphoma for Hodgkin’s disease [3,4].
There are five types of Hodgkin lymphoma classified by the World Health Organization: nodular sclerosing, mixed cellularity, lymphocyte depleted, lymphocyte rich and nodular lymphocyte-predominant [3]. Clinical presentation of Hodgkin lymphoma [5] is the following:
- a) Asymptomatic lymphadenopathy may be present (above the diaphragm in 80% of patients);
- b) Constitutional symptoms ( i.e., unexplained weight loss [>10% of total body weight], unexplained fever, night sweats) are present in 40% of patients; these are known as "B symptoms";
- c) Intermittent fever is observed in approximately 35% of cases;
- d) Chest pain, cough, shortness of breath, or a combination of those may be present due to a large mediastinal mass or lung involvement;
- e) Patients may present with pruritus; pain at sites of nodal disease, precipitated by drinking alcohol, occurs in fewer than 10% of patients but is specific for Hodgkin lymphoma;
- f) Back or bone pain may rarely occur.
A family history is also helpful; in particular, nodular sclerosis Hodgkin lymphoma (NSHL) has a strong genetic component and has often been previously diagnosed in the family. Hodgkin lymphoma is a potentially curable lymphoma.
Here the authors report a classical presentation of Hodgkin's disease in an otherwise healthy 27-year-old female.
Case report
In August 2015 an otherwise healthy 27-year-old female comes to the General Practitioner's office after experiencing flu-like symptoms with swelling on the left side supraclavicular region of the neck. Her past and recent medical histories were fine and no other remarkable co-morbidities were reported. Her family history was unremarkable.
The patient did not report any systemic symptoms including night sweats; weight loss or fever. The physical examination confirmed the presence of fixedlymph nodes of hard consistency in the left latero-cervical and supraclavicular area with an estimated size of 2.4 cm and without the evidence of any other superficial lymphadenopathy or organomegaly.
Subsequently laboratory test analysis were prescribed: complete blood count with differential, hepatic and renal function tests; protein electrophoresis; lactate dehydrogenase (LDH); serum electrolytes; protein electrophoresis; serology tests for Epstein-Barr virus (EBV), toxoplasmosis, HIV, and erythrocyte sedimentation rate (ESR); and C-reactive protein (CRP) inflammatory tests. An ultrasound exam of the neck and a chest X-ray were also prescribed. The biochemical results showed increased ESR and CRP as well as a neutrophilic leukocytosis of approximately 13,000 leukocytes per microliter. The neck ultrasound confirmed the presence of enlarged lymph nodes in the left supraclavicular side (2.4 × 1.3 cm) of the neck, with pathological aspects that were consistent with a lymphoproliferative disorder. The chest X-ray showed a left mediastinal enlargement (Figure 1).

Figure 1. Chest X-ray showed a marked left mediastinal enlargement.
To accelerate diagnostic procedures the patient was admitted to the internal medicine department. Chest Computed Tomography (Figure 2) showed enlarged nodes in the left supraclavicular and cervical regions, in the upper mediastinum including paratracheal prevascular, subcarinal, bilateral lung hilum sites, and bilaterally in the axillas. The largest node was 10 × 5 cm in diameter.
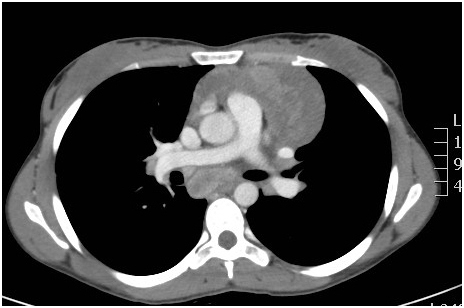
Figure 2. Chest CT scan showed enlarged nodes in the supraclavicular and cervical regions, in the upper mediastinum including paratracheal prevascular, subcarinal, bilateral lung hilum sites, and bilaterally in the axillas.
The spleen was normal buta focal liver lesion of 3 × 2.7 cm inside the 4 th segment was detected. Also a FDG-PET/CT scan (Figure 3) confirmed the presence of multiple pathological accumulations of enlarged lymphoadenopathy already described, but also more skeletral localizations.
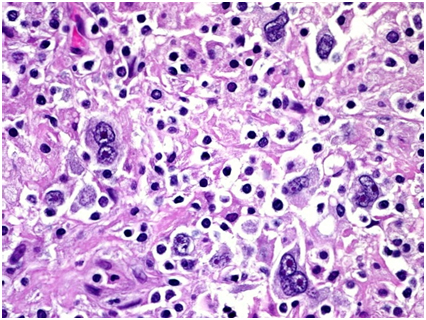
Figure 3. FDG-PET/CT scan revealed marked hypermetabolic nodes bilaterally in the laterocervical, supraclavicular and axillary regions, in the mediastinum, and within the left para-aortic space. The spleen was normal. An area of slightly increased glucose metabolism was also described in the IV° segment of the liver.
Supraclavear lymph node biopsy, histologic examination and immunohistochemical analysis made the diagnosis of classical Hodgkin’s lymphoma (nodular sclerosis subtype) by finding the diagnostic Reed-Sternberg cells and CD30 positive (Figure 4).
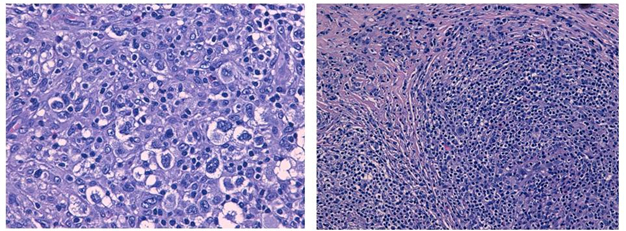
Figure 4. The histologic examination of lymph node biopsy specimens showed Reed-Sternberg cells and CD30 positive
Finally, a bone marrow biopsy was done but was negative for lymphoma. Based on the complete staging workup the final diagnosis for this 27-year-old patient was classical HL, nodular sclerosis, stage IV A. Her international prognostic score was 1 due to the advanced stage.
Usually Hodgkin’s lymphoma occurs in the mediastinum and head and neck regions but its presentation may be insidious. Therefore the diagnosis could be tardive.
Because Hodgkin lymphoma is considered a curable malignancy and the differential diagnosis is broad, medico-legal problems may arise from failure to diagnose the disease in a timely manner, possibly due to the following factors: 1)The misinterpretation of B symptoms; A lack of follow-up for abnormal chest radiographs or physical examination findings; 3) A missed pathologic diagnosis because a needle biopsy was obtained rather than an excisional lymph node biopsy [6].
As this case study reportsa histologic diagnosis of Hodgkin lymphoma is always required. An excisional lymph node biopsy is recommended because the lymph node architecture is important for histologic classification.
Furthermore, the Ann Arbor classification [7] is used most often for Hodgkin lymphoma, as follows:
- Stage I: A single lymph node area or single extra-nodal site
- Stage II: 2 or more lymph node areas on the same side of the diaphragm
- Stage III: Lymph node areas on both sides of the diaphragm
- Stage IV: Disseminated or multiple involvement of the extra-nodal organs
Based on the clinical scenario, staging and degree of end-organ damage in patients with HL can be categorized into the following 3 groups:
- Early-stage favorable
- Early-stage unfavorable (bulky and non-bulky)
- Advanced-stage (this classification has impact in treatment selection and must be performed carefully in every patient with HL)
Our patient was promptly investigated and diagnosis of HL was timely. She was affected by Hodgkin's Disease (Nodular sclerosis classic HL) in advanced-stage (Stage IVA), but her prognostic score, based on the IPS score, can be categorized at good risk (IPS 0-1) [8].
In conclusion, this case report is anecdotal but emblematic because it stresses once again the importance of early diagnosis, staging and risk stratification of Hodgkin's disease in primary care settings and internal medicine, to improve the survival rate of patients.
Acknowledgements
The authors thank Dr. Luca Riccioni, pathologist, for his courtesy.
The authors declare no conflict of interest.
- Lukes R, Butler J, Hicks E (1966) Natural history of Hodgkin’s disease as related to its patholgical picture. Cancer 19: 317–344
- Harris NL, Jaffe ES, Stein H, Banks PM, Chan JK, et al. (1994) A revised European-American classification of lymphoid neoplasms: a proposal from the International Lymphoma Study Group. Blood 84: 1361–1392. [ Crossref ]
- Jaffe ES, Harris NL, Stein H, Vardiman JW (2001) Pathology and Genetics of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press, Lyon, France.
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, et al. (2008) WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. International Agency for Research on Cancer, Lyon, France.
- Eichenauer DA, Engert A, Dreyling M, ESMO Guidelines Working Group (2014) Hodgkin's lymphoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 6: iii55-58. [ Crossref ]
- NCCN Clinical Practice Guidelines in Oncology: Hodgkin Lymphoma. Version 2.2015. National Comprehensive Cancer Network.
- Carbone PP, Kaplan HS, Musshoff K, Smithers DW, Tubiana M (1971) Report of the Committee on Hodgkin's Disease Staging Classification. Cancer Res 31: 1860–1861. [ Crossref ]
- Hasenclever D, Diehl V (1998) A prognostic score for advanced Hodgkin's disease. International Prognostic Factors Project on Advanced Hodgkin's Disease. N Engl J Med 339: 1506-1514. [ Crossref ]
Editorial Information
Editor-in-chief.
Dario Marchetti Baylor College of Medicine
Article Type
Case Report
Publication history
Received date: October 04, 2015 Accepted date: October 19, 2015 Published date: October 22, 2015
©2015 Bolognesi M. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Bolognesi M, Bolognesi D, Pasini G (2015). A classical presentation of Hodgkin's disease in a 27-year-old healthy female. Gen Int Med Clin Innov 1: doi: 10.15761/GIMCI.1000102
Corresponding author
General Practitioner, AUSL della Romagna District of Cesena, Via Ungaretti 494 47521 Cesena, Italy.
Journal Home
- Article Info
- Author Info
- Figures & Data
- Privacy Policy
- Terms & conditions
© 2018 Copyright OAT. All rights reserved.

IMAGES